Sodium bicarbonate on severe metabolic acidosis during prolonged cardiopulmonary resuscitation: a double-blind, randomized, placebo-controlled pilot study
Introduction
Previous guidelines recommended the use of sodium bicarbonate for preexisting hyperkalemia (Class I intervention), preexisting metabolic acidosis or tricyclic or barbiturates overdose (Class IIA), and for prolonged intervals of cardiopulmonary resuscitation (CPR) (Class IIB) (1). Some studies have shown favorable results in terms of increased return of spontaneous circulation (ROSC) and hospital admission rates (2-4), while the majority of studies have found that sodium bicarbonate administration may be counter-productive because it increases tissue and central venous blood carbon dioxide (CO2) tension, leading to paradoxical increase in respiratory acidosis (5-10). As a result, the 2010 advanced cardiac life support (ACLS) guidelines for adults did not recommend the routine use of sodium bicarbonate during CPR, except for preexisting metabolic acidosis, hyperkalemia, or tricyclic antidepressant overdose (11). These guidelines were not reviewed or revised in the latest update, published in 2015, because the International Liaison Committee on Resuscitation (ILCOR) task force determined that there was not a sufficient amount of new information to readdress this question (12-14). Nevertheless, sodium bicarbonate has been commonly used during resuscitation of out-of-hospital cardiac arrest (OHCA) patients (15) on the grounds that its use may be appropriate in patients with prolonged CPR as this can lead to severe acidosis which may trigger hemodynamic instability as a result of reduced left ventricular contractility and impaired responsiveness to catecholamines (16-18). In addition, recent studies have shown promising effects of sodium bicarbonate and, specifically, improved chances of ROSC and high survival rates with prolonged cardiac arrest (19,20).
In the context of this unclear clinical picture, we conducted a clinical trial to evaluate the effects of sodium bicarbonate with transient hyperventilation on the outcome of OHCA adult patients who failed to achieve ROSC and with severe metabolic acidosis (pH <7.1 or bicarbonate <10 mEq/L) after 10 minutes of CPR performed in the emergency department (ED) following OHCA resuscitation attempts. The null hypothesis was that the use of sodium bicarbonate with transient hyperventilation in these patients may improve acidosis without CO2 burden and enhance the rates of ROSC, survival to hospital admission, and good neurologic survival.
Methods
Study population
Between January 1 2015 and December 31 2015, all consecutive adult (≥18 years of age) patients admitted with non-traumatic OHCA to the Asan Medical Center were screened to determine whether they met the study criteria. The Asan Medical Center is a tertiary referral center in Seoul, Korea, with 108,000 patient admissions per year, according to a ED census. The inclusion criteria were as follows: patients who failed to achieve ROSC after 10 minutes of CPR in the ED and with severe metabolic acidosis (pH <7.1 or bicarbonate <10 mEq/L) on arterial blood gas analysis (ABGA). Exclusion criteria were patients with a previous do-not-resuscitate order, extracorporeal-CPR, ROSC within 10 minutes of ACLS, and absence of severe metabolic acidosis on ABGA after 10-minutes of CPR in the ED.
Study protocol
This study was designed as a double-blind, prospective, randomized, placebo-controlled clinical trial. The protocol was approved by the Institutional Review Boards of Asan Medical Center (No. 2014-0968), and the requirement for informed consent was waived in accordance with the ethical standards of the institutional review board. This study was registered under clinicaltrials.gov as protocol NCT02303548.
Patients received standard ACLS, including chest compression, intubation, ventilation, defibrillation, drug administration, including epinephrine and antiarrhythmic drugs if indicated, in the ED. After 10 minutes of ACLS, femoral arterial blood samples were obtained for ABGA from patients who failed to achieve ROSC. Blood samples were analyzed by a point-of-care-testing blood gas analyzer [GEM Premier 3,000 analyzer (Instrumentation Laboratory, Lexington, MA, USA)]. Patients with severe metabolic acidosis (pH <7.1 or bicarbonate <10 mEq/L) on ABGA were enrolled. A research associate generated a random sequence using Excel software. Patients fulfilling the study inclusion criteria were randomly assigned (1:1) to the study group, receiving sodium bicarbonate 50 mEq/L, or to the control group, receiving normal saline 50 mL injection over 2 minutes, in a double-blinded fashion. It is well known that sodium bicarbonate administration leads to CO2 burden (7), therefore, in order to prevent respiratory acidosis, we increased the ventilation rate from 10 to 20/minutes for 2 minutes after the drug (sodium bicarbonate in the study group or normal saline in the placebo group) administration. After 20 minutes of CPR in the ED, femoral ABGA was repeated.
Study end point
The primary end point was the change of acidosis, evaluated as the pH and bicarbonate levels. The secondary end points were sustained ROSC, defined as the restoration of a palpable pulse ≥20 minutes, survival to hospital admission, and good neurologic survival at 1 and 6 months, defined as cerebral performance category (CPC) 1 or 2; CPC scores are categorized as follows: 1 (no significant impairment), 2 (moderate impairment but able to complete activities of daily living), 3 (severe impairment but conscious), 4 (vegetative state or coma) and 5 (death).
Statistical analysis
An estimation of the number of patients needed was not derived because of the lack of any previous study in this clinical situation and the ethical issue of bicarbonate injection. This study was a pilot study, intended to test the feasibility of a larger study. A sample size of 50 subjects (25 subjects per group) was determined. Data were presented as means ± standard deviation (SD) or median with interquartile range (IQR), for continuous variables, and as number and percentages, for categorical variables. Student t-test, Fisher exact test, and Pearson’s χ2 test were used for intergroup comparisons. The Wilcoxon matched-pairs signed rank test was used to compare the blood gas results before and after drug administration. A two-sided P value <0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA).
Results
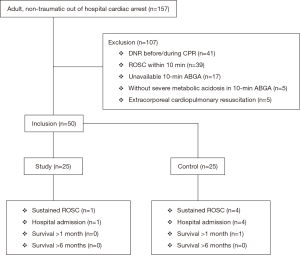
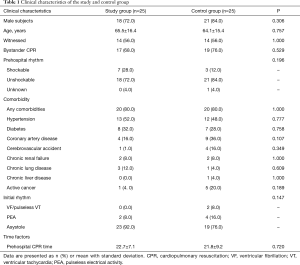
During the study period, 50 patients with OHCA were enrolled according to previously determined criteria. A total of 107 subjects were excluded (Figure 1). Clinical characteristics of patients are summarized in Table 1. There was no significant difference between the study group and control group in demographic characteristics, past medical history, witnessed arrest, performance of CPR by bystanders, and pre-hospital and initial cardiac rhythm. Duration of pre-hospital CPR was also not significantly different between the two groups.
Full table
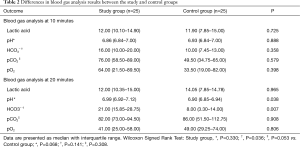
Before randomization, results of ABGA at 10 minutes were not significantly different between the study group and control group. At 20 minutes, pH [6.99 (6.92–7.12) vs. 6.90 (6.85–6.94), P=0.038] and HCO3− [21.00 (15.85–28.75) vs. 8.00 (3.30–14.00) mEq/L, P=0.007] levels were higher in the study group than in the control group, while pCO2 [82.00 (73.00–94.50) vs. 86.00 (51.50–112.75), P=0.908] levels were not significantly different (Table 2). The ABGA results before and after drug administration showed a significant increase in sodium bicarbonate levels in the study group [16.00 (10.00–20.00) vs. 21.00 (15.85–28.75), P=0.036]. However, changes were not significant in the control group, and pH and pCO2 changes were also not significant in either group.
Full table
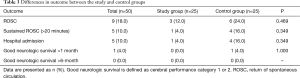
Sustained ROSC (>20 minutes) rate for the 50 enrolled patients was 10.0%. Overall, there was no difference in ROSC of any duration [3 (12.0) vs. 6 (24.0), P=0.469], sustained ROSC [1 (4.0%) vs. 4 (16.0%), P=0.349], hospital admission [1 (4.0%) vs. 4 (16.0%), P=0.349], and survival >1 month [0 (0.0%) vs. 1 (4.0%), P=1.000] between the study and the control group. No patient survived for >6 months (Table 3).
Full table
Discussion
We evaluated the effects of sodium bicarbonate administration based on blood gas analysis (pH <7.1 or bicarbonate <10 mEq/L) and duration of CPR (>10 minutes of CPR in the ED) in OHCA patients. The results indicated that the use of sodium bicarbonate improve the acid-base state, while it had no effect on the improvement of the rate of ROSC and good neurologic survival.
Only one prospective controlled clinical trial on buffer therapy in CPR has been reported since 2000 (4). Between 1994 and 1998, researchers from the University of Pittsburgh evaluated the effect of sodium bicarbonate on OHCA patients by comparing an experimental group (administered 1 mEq/kg of bicarbonate) and a control group (administered equal volume of normal saline) (4). Overall, there was no difference in survival between the groups (7.4% vs. 6.7%, P=0.88). However, in the subgroup of patients with prolonged (>15 minutes) pre-hospital arrest, survival rates were higher in the bicarbonate group than in the control group (32.8% vs. 15.4%, P=0.007). Although our study included only patients with prolonged CPR and severe metabolic acidosis, we found that sodium bicarbonate had no effect on the overall outcomes. This is in agreement with the findings of a retrospective cohort study by Wing et al., that sodium bicarbonate administration during prolonged CPR did not improve the sustained ROSC in OHCA patients [6.7% (2/30) vs. 19.4% (12/90), P=0.13] (21). It is interesting to note that the median time interval from CPR to sodium bicarbonate administration in Weng’s cohort and in our study were 36 minutes and 31 minutes, respectively. In addition, survival discharge rates were only 2.1% (2/92) and 2.0% (1/50), respectively, indicating that the outcome of prolonged CPR (>30 minutes) in patients with acidosis is poor. These data do not address the possibility of combining sodium bicarbonate along with extracorporeal membrane support or administration earlier in the resuscitation. We have previously reported most favorable outcomes are achieved with shorter resuscitation intervals (22,23).
The adverse effects associated with the use of sodium bicarbonate include metabolic alkalosis and the generation of CO2, which could induce respiratory acidosis; furthermore, CO2, by rapidly crossing the blood brain barrier may result in cerebrospinal fluid acidosis and cerebral edema (5). To our knowledge, this is the first study evaluating the effects of sodium bicarbonate with transient hyperventilation to overcome increased CO2 production. We increased the ventilation rate to 20/minutes for 2 minutes after the drug administration, and elevated pCO2 levels were found in both the study and control groups. These changes were not significant (P<0.05 in both groups). However, the administration of a single bolus of sodium bicarbonate with transient hyperventilation did not cause significant pCO2 elevation, which is one of the adverse effects of sodium bicarbonate administration of greatest concern. A 50 mL bolus of sodium bicarbonate will raise serum pH by approximately 0.1 of a pH unit (11). Serum pH in the bicarbonate group increased from 6.86 to 6.99, although in the control group the pH decreased from 6.93 to 6.90. Sodium bicarbonate administration with transient hyperventilation may increase serum pH without significant pCO2 elevation. However, despite the benefits of sodium bicarbonate administration according to blood gas analysis, sustained ROSC (>20 minutes), hospital admission, and survival >1 or 6 months did not improve.
The major limitation of our study relates to the small number of subjects. Administration of a single bolus of sodium bicarbonate with transient hyperventilation has not been previously evaluated and may cause unexpected harm to study subjects. Thus, the institutional review board did not allow a large clinical trial to be conducted. A further consideration is the use of a single empirical dosing of bicarbonate, such as 50 mEq/L, rather than weight-based administration. It is possible that smaller patients could have received an excessive dose of sodium bicarbonate, which, theoretically, may have mitigated adverse effects. Although the study protocol set a 10-minute interval of ABGA of blood samples drawn from the femoral artery, there is a chance that venipuncture during sampling under CPR conditions could lead to erroneously low acidic results (4). Finally, in our view, ABGA after 10-minute of ACLS in the ED would be a more precise indicator of the patient’s acid-base status than ABGA performed on patient arrival at the ED (24). We concede that there may also be another optimal time-point for ABGA. However, our cohort may be in a unique position for the study of the effects of bicarbonate on acidosis, for following reasons. Bicarbonate administration is not permitted in prehospital resuscitation in Korea; therefore, we could control bicarbonate administration until a specific time point. According to previous study conducted by our group (24-26), blood gas analysis or arterial line monitoring during CPR is a routine process in our ED.
Conclusions
Among adult non-traumatic OHCA patients with prolonged CPR and severe metabolic acidosis, the use of sodium bicarbonate during CPR with transient hyperventilation improve acid-base status without CO2 elevation which is one of the most concerned adverse effects of sodium bicarbonate administration, but it had no effect on the improvement of the rate of ROSC and good neurologic survival. At this point, we could not advise for or against its administration, our pilot data could be used to help design a larger trial to verify the efficacy of sodium bicarbonate.
Acknowledgements
We would like to thank the experts who were involved as an advisor for this research project: Prof. Jon C. Rittenberger and Clifton W. Callaway of Department of Emergency Medicine, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania. We thank Sung Sook Kim, on the behalf of Clinical Nurse Specialist at Emergency Department in Asan Medical Center, for their passionate participation and assistance. Without their passionate assistance and support, this trial could not have been successfully conducted.
Funding: This study was supported by a grant (2014-0968) from the Asan Institute for Life Sciences, Asan Medical Center, Seoul, Korea.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The protocol was approved by the Institutional Review Boards of Asan Medical Center (No. 2014-0968), and the requirement for informed consent was waived in accordance with the ethical standards of the institutional review board.
References
- Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care. Part 6: advanced cardiovascular life support: section 6: pharmacology II: agents to optimize cardiac output and blood pressure. Circulation 2000;102:I129-35. [PubMed]
- Weaver WD, Fahrenbruch CE, Johnson DD, et al. Effect of epinephrine and lidocaine therapy on outcome after cardiac arrest due to ventricular fibrillation. Circulation 1990;82:2027-34. [Crossref] [PubMed]
- Bar-Joseph G, Abramson NS, Kelsey SF, et al. Improved resuscitation outcome in emergency medical systems with increased usage of sodium bicarbonate during cardiopulmonary resuscitation. Acta Anaesthesiol Scand 2005;49:6-15. [Crossref] [PubMed]
- Vukmir RB, Katz L. Sodium Bicarbonate Study G. Sodium bicarbonate improves outcome in prolonged prehospital cardiac arrest. Am J Emerg Med 2006;24:156-61. [Crossref] [PubMed]
- White SJ, Himes D, Rouhani M, et al. Selected controversies in cardiopulmonary resuscitation. Semin Respir Crit Care Med 2001;22:35-50. [Crossref] [PubMed]
- Brown C, Wiklund L, Bar-Joseph G, et al. Future directions for resuscitation research. IV. Innovative advanced life support pharmacology. Resuscitation 1996;33:163-77. [Crossref] [PubMed]
- Neumar RW, Otto CW, Link MS, et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S729-67. [Crossref] [PubMed]
- Weil MH, Ruiz CE, Michaels S, et al. Acid-base determinants of survival after cardiopulmonary resuscitation. Crit Care Med 1985;13:888-92. [Crossref] [PubMed]
- Bishop RL, Weisfeldt ML. Sodium bicarbonate administration during cardiac arrest. Effect on arterial pH PCO2, and osmolality. JAMA 1976;235:506-9. [Crossref] [PubMed]
- Kette F, Weil MH, Gazmuri RJ. Buffer solutions may compromise cardiac resuscitation by reducing coronary perfusion presssure. JAMA 1991;266:2121-6. [Crossref] [PubMed]
- Vanden Hoek TL, Morrison LJ, Shuster M, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S829-61. [Crossref] [PubMed]
- Lavonas EJ, Drennan IR, Gabrielli A, et al. Part 10: Special Circumstances of Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132:S501-18. [Crossref] [PubMed]
- Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132:S444-64. [Crossref] [PubMed]
- Truhlar A, Deakin CD, Soar J, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 4. Cardiac arrest in special circumstances. Resuscitation 2015;95:148-201. [Crossref] [PubMed]
- Glover BM, Brown SP, Morrison L, et al. Wide variability in drug use in out-of-hospital cardiac arrest: a report from the resuscitation outcomes consortium. Resuscitation 2012;83:1324-30. [Crossref] [PubMed]
- Kraut JA, Madias NE. Treatment of acute metabolic acidosis: a pathophysiologic approach. Nat Rev Nephrol 2012;8:589-601. [Crossref] [PubMed]
- Marsh JD, Margolis TI, Kim D. Mechanism of diminished contractile response to catecholamines during acidosis. Am J Physiol 1988;254:H20-7. [PubMed]
- Orchard CH, Kentish JC. Effects of changes of pH on the contractile function of cardiac muscle. Am J Physiol 1990;258:C967-81. [Crossref] [PubMed]
- Kim J, Kim K, Park J, et al. Sodium bicarbonate administration during ongoing resuscitation is associated with increased return of spontaneous circulation. Am J Emerg Med 2016;34:225-9. [Crossref] [PubMed]
- Chung CW, Lui CT, Tsui KL. Role of sodium bicarbonate in resuscitation of out-of-hospital cardiac arrest. Emergency Medicine 2015;22:281-90.
- Weng YM, Wu SH, Li WC, et al. The effects of sodium bicarbonate during prolonged cardiopulmonary resuscitation. Am J Emerg Med 2013;31:562-5. [Crossref] [PubMed]
- Reynolds JC, Frisch A, Rittenberger JC, et al. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies? Circulation 2013;128:2488-94. [Crossref] [PubMed]
- Reynolds JC, Grunau BE, Rittenberger JC, et al. The association between duration of resuscitation and favorable outcome after out-of-hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Kim YJ, Lee YJ, Ryoo SM, et al. Role of blood gas analysis during cardiopulmonary resuscitation in out-of-hospital cardiac arrest patients. Medicine (Baltimore) 2016;95:e3960. [Crossref] [PubMed]
- Kim YJ, Kim WY. Emerging role of arterial blood gases during cardiopulmonary resuscitation: Another reason for invasive arterial pressure monitoring. Resuscitation 2016;107:e15. [Crossref] [PubMed]
- Ahn S, Kim WY, Sohn CH, et al. Potassium values in cardiac arrest patients measured with a point-of-care blood gas analyzer. Resuscitation 2011;82:e25-6. [Crossref] [PubMed]


