Thoracoscopic lobectomy for massive hemoptysis caused by complete pulmonary vein occlusion after radiofrequency ablation for atrial fibrillation
Introduction
Transcatheter radiofrequency ablation is a common and effective treatment strategy for recurrent and drug-resistant atrial fibrillation. Pulmonary vein stenosis and occlusion are rare complications of ablation. Severe pulmonary vein stenosis and occlusion can cause hemoptysis; however, only a few cases of massive hemoptysis caused by pulmonary vein occlusion have been reported to date. We here report a patient with massive hemoptysis caused by complete pulmonary vein occlusion after radiofrequency ablation for atrial fibrillation who was successfully treated by thoracoscopic lobectomy.
Case presentation
A 37-year-old man was referred to our Thoracic Surgery Department after experiencing intermittent massive hemoptysis for the previous 2 weeks, during which time he had been treated in the Emergency Department. His medical records showed he had a 3-year history of drug-refractory paroxysmal atrial fibrillation. Transcatheter radiofrequency ablation had been performed twice, 3 years and 1 year previously, at another institution. Sinus rhythm had been restored by the transcatheter radiofrequency ablation 1 year previously and his clinical course had been uneventful until 2 weeks previously, when he had expectorated about 1,000 mL of blood over 24 hours. An emergency computed tomographic scan showed patchy areas of ground-glass opacity in the left upper lobe, suggesting pulmonary alveolar hemorrhage (Figure 1). Bronchial artery angiography was arranged. Polyvinyl alcohol particle and stainless steel platinum coil embolization was performed to control the massive hemoptysis and hemostatic drugs and blood products were administered, resulting in a decrease in the volume of expectorated blood to 100 mL per 24 hours.
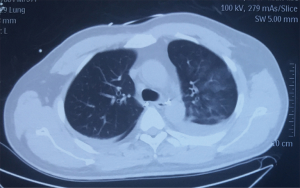
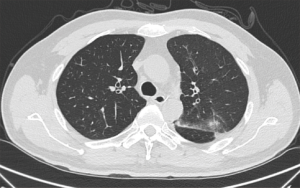
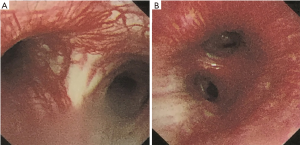
When the patient was admitted to our Thoracic Surgery Department, he was stable and expectorating 30–50 mL of blood daily. A contrast computed tomographic scan showed fewer areas of ground-glass opacity and less consolidation of the left upper lobe than a previous chest computed tomographic scan taken 2 weeks earlier in the Emergency Department (Figures 1,2) and revealed total occlusion of the left superior pulmonary vein (Figure 3A,B) and mild stenosis of the left inferior pulmonary vein (Figure 3C,D). Bronchoscopy showed hyperemic left main and left upper lobe bronchi and severe dilation of submucosal blood vessels (Figure 4). An echocardiogram showed normal pulmonary arterial pressure. The patient was diagnosed as having massive hemoptysis as a result of left superior pulmonary vein occlusion caused by transcatheter radiofrequency ablation on the basis of these findings.

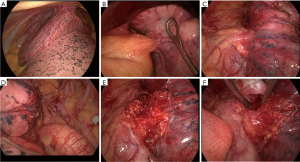
Left upper lobectomy was performed by video-assisted thoracoscopy using two ports: a 10-mm port for the camera in the seventh intercostal space and a 40-mm surgical incision in the fourth intercostal space. The left upper lobe was adherent to the chest wall and the mediastinum (Figure 5A,B). Neovascularization was visible overlying the left upper lobe, hilum, and descending aorta (Figure 5A,C,D). The mediastinal pleura were incised in the hilar region. Severe adhesion was noted (Figure 5E). The left superior pulmonary vein was completely obliterated, having been replaced with dense fibrotic tissues. It proved impossible to dissect the left superior pulmonary vein from the left upper lobe bronchus (Figure 5F) and it was feared that forced isolation might tear the superior pulmonary vein. The proximal branches of the pulmonary artery were difficult to access from the anterior perspective without isolation and division of the superior pulmonary vein. The oblique fissure was therefore dissected to expose the interlobar pulmonary artery and its branches. When they had been identified, the arterial branches to the left upper lobe were divided and the posterior and anterior fissure stapled, leaving the left superior pulmonary vein and left upper lobe bronchus. Finally, an Endo-GIA 45 purple Tri-stapler (Medtronic, Minneapolis, MN, USA) was used to staple both the bronchus and obliterated pulmonary vein. The surgery was successful with intraoperative bleeding of 150 mL and the postoperative course was uneventful, with no complications such as recurrence of hemoptysis or development of a bronchopleural fistula. The patient spent two days in ICU. The chest tube was removed on postoperative Day 5, the daily drainage having been 200 mL, and was discharged on postoperative Day 8 with a normal chest radiograph. Outpatient clinic follow-up was arranged at 2 weeks, 3 months and 6 months after discharge. The patient remained free of symptoms, such as hemoptysis or dyspnea, and recovered well.
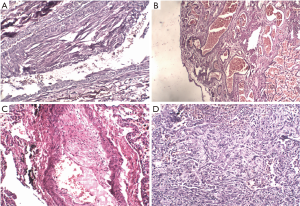
Histologic examination of hematoxylin and eosin stained-sections demonstrated thrombosis and obliteration of the left upper pulmonary vein (Figure 6A), dilatation of tortuous pleural vessels (Figure 6B), obliterative fibromuscular thickening of arteries (Figure 6C), and inflammatory pseudotumor formation caused by proliferation of myofibroblasts (Figure 6D).
Discussion
Pulmonary vein stenosis and occlusion are rare causes of hemoptysis. The present patient was unique in his presentation with massive hemoptysis that necessitated surgical intervention. The incidence of pulmonary vein stenosis after transcatheter radiofrequency ablation is 1% to 3% and that of total pulmonary vein occlusion even less (1). A diagnosis of pulmonary vein occlusion should be considered when a patient presents with hemoptysis and has a history of transcatheter radiofrequency ablation for atrial fibrillation.
There is no consensus on the management of pulmonary vein stenosis or occlusion. Early pulmonary vein stenosis and limited involvement of pulmonary vein may be suitable for balloon dilation or stenting; however, restenosis rates are high (2). Chronic pulmonary vein stenosis and total pulmonary vein occlusion may cause irreversible intrapulmonary vascular changes. The intimal hyperplasia and medial thickening of both pulmonary veins and arteries leads to pulmonary vascular remodeling, which can result in severe pulmonary hypertension (3). Resection of the involved lung may be more appropriate with this scenario.
Our patient had a completely occluded left superior pulmonary vein for which video-assisted thoracoscopic left upper lobectomy was performed. Severe inflammatory adhesion prevented dissection of the completely obliterated left superior pulmonary vein from the left upper lobe bronchus. Stapling both the bronchus and obliterated pulmonary vein using an Endo-GIA 45 purple Tri-stapler was achieved safely with no complications, such as bronchopleural fistula or hemoptysis. At regular follow-up the patient remained free of symptoms, such as hemoptysis or dyspnea, and recovered well. Pathological examination of the resected specimen showed obliteration of the left upper pulmonary vein, thickened arteries, and inflammatory pseudotumor formation.
Up to 38% of patients with severe stenosis or completely occlusion are asymptomatic. Others have non-specific symptoms, such as shortness of breath, cough, chest pain, or hemoptysis. The diagnosis of pulmonary vein stenosis or occlusion is usually delayed. It is strongly recommended that post-ablation patients be followed up with regular enhanced CT or MRI (4,5). Early diagnosis may provide the opportunity to perform transcatheter balloon angioplasty or stenting, thus obviating the need for surgical intervention. Delayed diagnosis allows development of irreversible pulmonary vascular remodeling, which demands surgical resection. Video-assisted thoracoscopic lobectomy is safe means of managing complete pulmonary vein occlusion and has minimal complications (6-8).
In conclusion, complete pulmonary vein occlusion is a severe complication of transcatheter radiofrequency ablation and can cause massive hemoptysis. Thoracoscopic resection of the involved lobe is feasible and safe.
Acknowledgements
We thank Dr Trish Reynolds, MBBS, FRACP, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Booher AM, Bach DS. Acquired pulmonary vein stenosis: one problem, two mechanisms. J Am Soc Echocardiogr 2010;23:904.e1-3. [Crossref] [PubMed]
- Yan J, Wang C, Du R, et al. Pulmonary vein stenosis and occlusion after radiofrequency Catheter Ablation for atrial fibrillation. Int J Cardiol 2013;168:e68-71. [Crossref] [PubMed]
- Yang HM, Lai CK, Patel J, et al. Irreversible intrapulmonary vascular changes after pulmonary vein stenosis complicating catheter ablation for atrial fibrillation. Cardiovasc Pathol 2007;16:51-5. [Crossref] [PubMed]
- Baranowski B, Saliba W. Our approach to management of patients with pulmonary vein stenosis following AF ablation. J Cardiovasc Electrophysiol 2011;22:364-7. [Crossref] [PubMed]
- Prieto LR, Kawai Y, Worley SE. Total pulmonary vein occlusion complicating pulmonary vein isolation: diagnosis and treatment. Heart rhythm 2010;7:1233-9. [Crossref] [PubMed]
- Lo CM, Lu HI, Chen YY, et al. Thoracoscopic lobectomy for pulmonary vein occlusion after radiofrequency catheter ablation of atrial fibrillation. J Cardiothorac Surg 2016;11:12. [Crossref] [PubMed]
- Lee JY, Chon GR, Park JH, et al. Massive hemoptysis due to pulmonary vein stenosis following catheter ablation for atrial fibrillation. Respir Care 2015;60:e52-5. [Crossref] [PubMed]
- Libretti L, Ciriaco P, Zannini P. Pulmonary vein stenosis requiring lobectomy after radiofrequency catheter ablation for atrial fibrillation. J Cardiovasc Surg (Torino) 2012;53:821-3. [PubMed]


