Epithelial-myoepithelial carcinoma of the trachea—a rare entity case report
Introduction
Epithelial-myoepithelial carcinoma (EMCa) is a rare low-grade malignant salivary gland neoplasm that most commonly occurs in the parotid gland but can also arise in minor salivary glands. About 120 cases have been reported in the world literature, most of which were located in salivary glands, except for a few cases occurring in unusual locations such as breast, lachrymal gland, nose, paranasal sinus, trachea, bronchus, and lung (1-3).
Myoepithelial tumors typically manifest as an endobronchial mass of a lobar bronchus, and a peripheral type of tumor has been reported as well. Although histologically bland, myoepitheliomas show frequent distant metastasis. EMCa is pathologically characterized by a dual-cell population, including an inner layer of cuboidal epithelial cells that are peripherally bounded by a layer of myoepithelial cells (4,5).
We report a case of a 34-year-old man who presented to our hospital with vigorous cough and dyspnoea.
Case report
A 34-year-old Caucasian man presented at our hospital due to dyspnoea and vigorous cough for more than1year period. The patient did not have a history of asthma in childhood but he had been treated for asthma-like symptoms during the last six months. He was already taking maintenance therapy with an inhaled corticosteroid twice daily and when needed, an inhaled short-acting beta 2 sympathomimetic agent. Apart from these medications, he took no other drugs. He was an ex-smoker (30 packs/year) with no other lung related medical history. Physical examination was remarkable for severe stridor, wheezing heard in upper fields of both lungs, tachycardia (110 b/min) and tachypnea (respiratory rate 30/min). Wheezing heard not only during auscultation but also by patient himself and had no correlation with physical exertion. An arterial blood gas analysis yields the following findings: PO2 =75 mmHg, PCO2 =25 mmHg, pH =7.41. Pulmonary function tests reveal a Forced Expiratory Volume in second (FEV1) that is 75% of the normal value and an FEV1/IVC ratio of 70%. He denied having other symptoms such as hemoptysis, difficulty swallowing, hoarseness, fatigue and weight loss. There were no palpable lymph nodes. Laboratory findings were unremarkable.
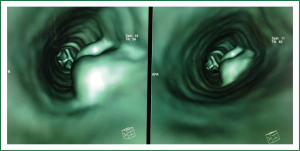
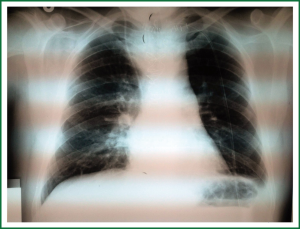
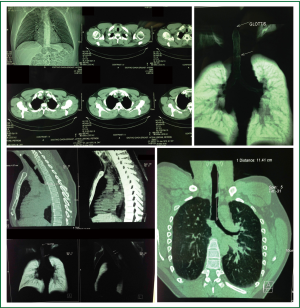
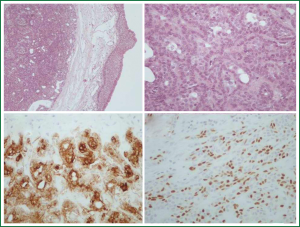
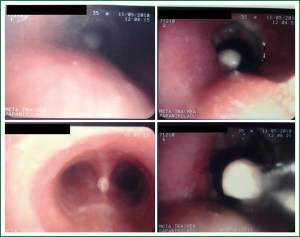
The patient’s chest X-ray was normal except from an intraluminal defect not easily recognized in the mid trachea (Figure 1). A computed topographic scan of the neck and chest showed an endotracheal mass of 1.15 cm in diameter originating from left lateral wall, occluding 80-90% of the lumen. The distance of the tumor from the cricoid cartilage was about 4.4 cm and the distance between the cricoids cartilage and the carina was about 11.4 cm (Figure 2) it was smoothly shaped, well-margined, uniformly dense, arising from the membranous wall of the trachea. There was not any mediastinal lymph node enlargement. Fiberoptic bronchoscopy revealed an intraluminar tumor of tracheal wall, which was bleeding to touch (Figure 3). The movable tumor obstructed nearly 90% of the lumen and the scope couldn’t pass easily through the narrowed route. Biopsy revealed neoplasm formed by biphasic cell population arranged by an inner layer of duct—forming epithelial cells and an out layer of myoepithelial cells over a fibrous, mucinous stroma (Figure 4A). The epithelial-myoepithelial dualism was confirmed using immunohistochemical methods: the epithelial cells were positive for Ck7 (Figure 4B) and Ck8/18; the myoepithelial cells were positive for S-100 protein, SMA (smooth muscle actin) and p63 (Figure 4C). Expression of proliferation index Ki-67 was particularly low (Figure 4D).
Surgical resection was advised. The patient underwent surgery. A median incision was performed followed a median sternotomy. The trachea was mobilized from the neck to the carina, sleeve resection comprising five tracheal rings was performed, and an end-to-end anastomosis was accomplished. The patient remained intubated for a day and extubated with success without having any difficulties. To protect the trachea, neck expansion was restricted until postoperative day 7th.
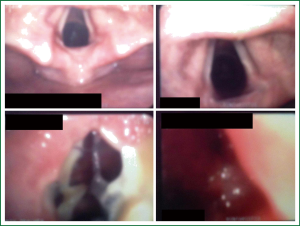
The postoperative course was uneventful till the day 8th were he noticed that each time oral feeding was initiated the patient cough vigorously and complain of breathing difficulty. Possibility of a tracheoesophageal fistula (TEF) was considered. Routine laboratory examinations were unremarkable. X-ray disclosed a widened mediastinum (Figure 5). A bronchoscopic inspection demonstrated a small-sized TEF (Figure 6).
All this time he had normal temperature, with normal hemodynamics and respiration. The patient was nursed semi upright, was established on total parenteral nutrition (TPN) and treated conservatively. He had no more respiratory problems and his condition gradually stabilized.
One week after, the patient developed back pain, chest pain, sputum production, paroxysms of coughing and become hypoxaemic. During physical examination deep cervical emphysema was found. Fiberoptic bronchoscopy revealed a rupture in the place of anastomosis (Figure 7). Due to tracheal laceration with severe respiratory disorder he underwent emergent repair and reconstruction of the trachea. There was a successful closure of TEF. Following this procedure, aspiration remitted, and there was no leakage through the fistula by esophagography. Soon after surgery the patient was extubated, and he healed without any other complication. He was discharged on day 25th. There was no evidence of recurrence at two years after surgery.
Discussion
Primary tumors of the trachea are rare and account for 0.1% of all malignancies. In adults, approximately 90% of the primary tracheal tumors are malignant, whereas in children, the majority of these tumors are benign. Primary tracheal tumors can arise from the respiratory epithelium, salivary glands and mesenchymal structure of the trachea (6). EMCa was described in the 1991 WHO international classification of salivary tumors. EMCa is an uncommon, biphasic salivary gland malignancy composed of ductal epithelial cells and myoepithelial cells with a broad morphologic spectrum. In the classic definition of EMCa, the myoepithelial component consists of polygonal cells with clear cytoplasm, whereas the ductal component is composed of small lumina lined by cuboidal, mildly eosinophilic cells reminiscent of intercalated ducts (7).
The tracheobronchial glands are considered to be counterparts of the minor salivary glands in the respiratory tract and can develop similar tumors (tumors of salivary gland type). Within this group of neoplasia EMCa of the respiratory tract is very rare and the diagnosis is often difficult (8).
Myoepithelial tumors typically manifest as an endobronchial mass of a lobar bronchus and a peripheral type of tumor has been reported as well. Although histologically bland, myoepitheliomas show frequent distant metastasis. EMCa is pathologically characterized by a dual-cell population, including an inner layer of cuboidal epithelial cells that are peripherally bounded by a layer of myoepithelial cells (4). The differential diagnosis of this neoplasms is quite broad and depends on the relative predominance of the myoepithelial cells (especially of those with clear appearance), or of the biphasic pattern (9,10).
These tumors usually are showing slow progression that’s why may be easily misdiagnosed as other disease. They can mimic asthma therefore tracheal tumors may be considered in the differential diagnosis of patients with intractable asthma-like symptoms. From pathological perspective, differential diagnosis of EMCa includes a pleomorphic adenoma, adenoid cystic carcinoma, myoepithelyoma and the other primary salivary gland-type tumors. Furthermore, primary and metastases of clear cell carcinoma must be distinguished from EMCa. In our case, the tumor has neither recurred nor metastasized, which is an evidence supporting the current opinion that EMCa is a tumor of low-grade malignancy (4,11,12).
Fiberoptic bronchoscopy is part of the evaluation for most tracheal tumors. Its role is to help identify obstructions, either intrinsic to tracheal lumen or extrinsic and causing compression. Bronchoscopy should be performed under optimal conditions because the risk of acute airway compromise is high (4).
Surgical resection with reconstruction of trachea is the mode of treatment with the best results.
Conclusions
EMCa is a low-grade malignant tumour. According to literature, most commonly occurs in salivary glands, particularly in parotic gland, but it can also occur in unusual locations such as breast, lachrymal gland, nose, paranasal sinus, lung, and bronchus, as in our case, trachea. It should be kept in mind in order to prevent delay in diagnosis that this rare entity may mimic intractable asthma.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Jin XL, Ding CN, Chu Q. Epithelial-myoepithelial carcinoma arising in the nasal cavity: a case report and review of literature. Pathology 1999;31:148-51. [PubMed]
- Tsuji N, Tateishi R, Ishiguro S, et al. Adenomyoepithelioma of the lung. Am J Surg Pathol 1995;19:956-62. [PubMed]
- Muñoz G, Felipo F, Marquina I, et al. Epithelial-myoepithelial tumour of the lung: a case report referring to its molecular histogenesis. Diagn Pathol 2011;6:71. [PubMed]
- Xu HT, Lin XY, Li QC, et al. The alveolar epithelial differentiation of glandular inner lining cells in a mucoepidermoid carcinoma of the lung: a case report. Diagn Pathol 2012;7:137. [PubMed]
- Yamada S, Noguchi H, Nabeshima A, et al. Basaloid carcinoma of the lung associated with central cavitation: a unique surgical case focusing on cytological and immunohistochemical findings. Diagn Pathol 2012;7:175. [PubMed]
- Chowdhury Q, Rahman MA, Sultana L, et al. Tracheal adenocarcinoma treated with adjuvant radiation: a case report and literature review. Case Rep Oncol 2013;6:280-4. [PubMed]
- Seethala RR, Richmond JA, Hoschar AP, et al. New variants of epithelial-myoepithelial carcinoma: oncocytic-sebaceous and apocrine. Arch Pathol Lab Med 2009;133:950-9. [PubMed]
- Morresi-Hauf AT, Reu S, Fertl A. Epithelial-myoepithelial carcinoma of the trachea. Case report and review of the literature. Pathologe 2013;34:56-64. [PubMed]
- Pelosi G, Fraggetta F, Maffini F, et al. Pulmonary epithelial-myoepithelial tumor of unproven malignant potential: report of a case and review of the literature. Mod Pathol 2001;14:521-6. [PubMed]
- Szczepanek-Parulska E, Szkudlarek M, Majewski P, et al. Thyroid nodule as a first manifestation of Hodgkin lymphoma-report of two cases and literature review. Diagn Pathol 2013;8:116. [PubMed]
- Maounis N, Chorti M, Legaki S, et al. Metastasis to the breast from an adenocarcinoma of the lung with extensive micropapillary component: a case report and review of the literature. Diagn Pathol 2010;5:82. [PubMed]
- Borriello M, Lucidi A, Carbone A, et al. Malignant transformation of Madelung’s disease in a patient with a coincidental diagnosis of breast cancer: a case report. Diagn Pathol 2012;7:116. [PubMed]