The burden of heart failure in the general population: a clearer and more concerning picture
The syndrome of heart failure constitutes a major global health problem. Patients with heart failure exhibit substantial morbidity and poor survival which at best, is similar to cancer (1,2). In addition, heart failure causes enormous healthcare expenditure. A number of recent reports suggest that the overall number of people living with heart failure is increasing due to sizable increases in predisposing diseases or comorbidities (such as diabetes, obesity and hypertension) and due to an aging population in general (3,4). Precise knowledge on the epidemiology of heart failure is required to inform policymakers on how most wisely utilize available resources.
In a recent paper, Conrad et al. provide contemporary insight into the magnitude of heart failure (HF) burden in a representative sample of the general population of the UK (5). Using electronic health records on over 4 million individuals between 2002 and 2014 which were standardized to the 2013 European Standard population they showed that incidence (standardized by age and gender) decreased by 7%, from 358 to 332 per 100,000 population, resulting in an incidence ratio of 0.93. This reduced incidence appeared to be mainly driven by a lower incidence of heart failure in people between 60 and 84 years of age. By contrast, the incidence in people aged 85 and older had increased substantially over the observation period. Moreover, the authors found that the number of individuals with newly diagnosed HF had increased by 12% and the absolute prevalence (i.e., absolute number of individuals living with heart failure) by 23%. The latter corresponded to approximately 170,000 more patients living with heart failure in 2014 than in 2002 (from 750,127 to 920,616). The authors attributed this very substantial increase to population growth and aging, in addition to more people surviving a myocardial infarction.
This data is consistent with a report from Olmsted County, MN, which demonstrated a significant decline in the age- and sex-adjusted incidence of HF from 315.8 to 219.3 per 100,000 in 2010 (6). Those authors also found that, due to the population growth and increased longevity, the overall prevalence and associated total burden of heart failure had markedly increased.
Other important findings by Conrad et al. are significant increases from 2002 to 2014 in the age (mean ± standard deviation) at first diagnosis of heart failure (from 76.5±12.0 to 77.0±12.9 years), and in the number of comorbid disorders (from 3.4±1.9 to 5.4±2.5). In other words, in addition to a rise in overall number, there appears to be a substantial increase in complexity of HF cases with time in the current cohort. More comorbidities generally mean more clinical events including hospitalizations both for HF and other causes although the comorbidity burden may differ according to age, gender and HF phenotype (7,8). The reported increased comorbidity burden in the work by Conrad et al. is worthy of further comment. Approximately two thirds of subjects suffered from comorbid hypertension, almost half had underlying ischemic heart disease, and 24% had kidney dysfunction or failure. By current definitions 30% to 50% of the adult population suffers from elevated (higher than normal) blood pressure, a number which is projected to increase steadily (3). Hypertension itself is a major cause of heart failure (also reflected in the current study) and ischemic heart disease. Many hypertensives go undiagnosed, and many hypertensives on pharmacological treatment do not meet blood pressure goals defined by guidelines bodies (9). Numerous studies show an association between adherence to guidelines and outcome (10,11). According to recent statistics jointly published by the American Heart Association and American College of Cardiology, one third of the adult population in the US has stage A HF, defined as the presence of predisposing conditions for HF (3).
Different phenotypes of HF are known which are commonly categorized according to the left ventricular ejection fraction (EF), a measure of pump function, and may differ in the way they respond to medical and other therapy (10,12). The current paper by Conrad et al. did not distinguish between heart failure with reduced EF (HFrEF) and midrange (HFmrEF) or preserved EF (HFpEF). Such data would have been of interest because many reports suggest that patients in higher EF categories tend to die more frequently from non-cardiovascular comorbidities than from heart failure and cardiovascular disease (6).
According to Conrad et al., the contemporary burden of HF in the UK corresponds to the burden of the four most common forms of cancer. Comparisons such as these help to put the current paper into context: while mortality from cancer has decreased over recent decades, mortality from HF has not (1,2). It is also worthwhile pursuing the analogy to cancer when it comes to utilization of potentially preventive strategies. Many cancer types do not evolve from longstanding risk factors which are highly modifiable through lifestyle or pharmalogical intervention; rather they result from inherited or spontaneously occurring gene mutations and under the influence of environmental factors which for the most part cannot be modulated.
By contrast, a sizable proportion of HF cases result from longstanding, often inadequately managed hypertension or ischemic heart disease; major cardiovascular disease entities which themselves often evolve from unhealthy lifestyle. In the current paper by Conrad et al. 67% suffered from hypertension, 49% from ischemic heart disease and 28% and 22% from dyslipidemia and diabetes, respectively. Unhealthy lifestyles are modifiable risk factors (as opposed to genetic factors) and therefore present an opportunity for intervention. In fact, data from Olmstead county suggest that ischemic heart disease, hypertension, diabetes, obesity and smoking underlie over half of incident HF cases (13).
In the international REACH registry, the presence of DM conferred a greater risk for HF hospitalization (14). Potentially modifiable, unhealthy lifestyles are more prevalent in lower socioeconomic classes. More deprived people were more likely to develop HF, did so earlier on, and had more comorbidities despite younger age than non-deprived individuals. The widening socioeconomic gap described by Conrad et al. therefore underscores the necessity to strengthen preventive strategies:
Not even half of the adult hypertensive population is meeting guidelines recommended blood pressure treatment goals. The lack of disabling symptoms in stand-alone hypertension may sometimes facilitate a lenient attitude of clinicians and poor medication compliance of patients (15,16).
By contrast, HF is a highly symptomatic, disabling condition. Yet, the possibility to actually prevent HF frequently attracts less public attention than the latest pill or device. This is striking because prevention may well be the most impactful area to improve HF care. The data by Conrad et al. should revitalize efforts to inform and educate the public in order to prevent HF.
The success with antismoking campaigns and subsequent reductions in the number of smokers as well as in the number of myocardial infarctions underscores the feasibility of targeted preventive measures in cardiovascular medicine. The HF community needs to more rigorously develop preventive programs specific to HF and implement these in the population. At age 45 years through age 95 years, lifetime risk for HF is estimated at 20% to 45%, and substantially higher with higher blood pressure and body mass index (3).
HF prevention efforts should target highest risk groups to maximize gain. In general, such programs should enhance public knowledge on HF and center around the value of healthy lifestyle including diets and on physical activity as those are associated with lower risk to develop HF.
Once HF is permitted to advance to symptomatic stages, the prognosis becomes grim. Co-authoring the current study, Jhund et al. reported long-term trends of HF hospitalization for the entire population of Scotland between 1986 and 2004 (17). Although they found modest decreases in first-time hospitalization for HF and case-fatality rates with time, median survival after hospitalization for a first episode of HF remained poor and averaged only just over 2 years (17). Hospitalizations are often recurrent in nature and represent the single most important driver of cost in heart failure care. Research efforts have been made into monitoring and early detection of deteriorating heart failure, with overall mixed results (18).
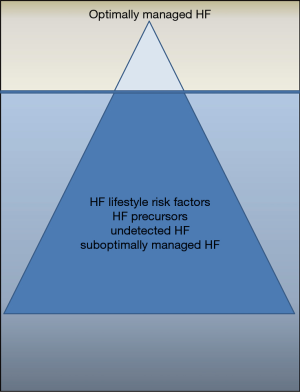
Taken together, despite a better insight that Conrad et al. provide into the magnitude of the burden caused by heart failure we have to acknowledge the tremendous challenges that follow: the proportion of patients with adequately diagnosed and phenotyped heart failure and on contemporary optimal guidelines-conform medical and non-medical (devices etc.) therapy is just a fraction of what it should be; perhaps at best corresponding to the tip of the “HF iceberg” versus its submerged mass (Figure 1).
How can the data by Conrad et al. help us to understand and improve our contemporary handling of the problem, and how should this data inform our futures strategies to bring down morbidity, mortality and expenditure caused by HF?
First, the wider public needs to acknowledge the tremendous increase in people living with heart failure and a decreasing ability to care for them due to budgetary constraints and logistical challenges. Quality of HF are should not have to decrease so that caregivers can put up with more patients. As outlined above, we need to increase our efforts to prevent HF through managing preventable predisposing conditions such as hypertension and discourage unhealthy lifestyles leading to obesity (9). If the prevention of HF as deadly and disabling condition was added as primary goal in the management of hypertension treatment, and that goal was clearly communicated to the wider public, likely many HF cases may be prevented. Medication non-adherence may be even greater in HF than in hypertension due to a higher percentage of polypharmacy. Moreover, there is likely going to be a greater discrepancy between the number of subjects living with HF and the number of specialized HF specialists and dedicated HF centers. Other key efforts should include a more timely diagnosis and earlier initiation and up-titration of therapies proven to reduce clinical event rates. Important pathophysiological mechanisms affecting the cardiovascular system may be incompletely modulated by standard medical therapies. Novel dual-acting neurohormonal antagonists, which more comprehensively target important maladaptive processes have been recently introduced into clinical practice (19-21). Most importantly, with global healthcare budgets under strain, disease entities predisposing to HF such as hypertension and ischemic heart disease deserve even greater vigilance.
The work by Conrad is a timely reminder that the medical community needs to step up its efforts to tackle HF. With regards to evolution of specific HF preventive strategies, we are probably only witnessing the end of the beginning.
Acknowledgements
None.
Footnote
Conflicts of Interest: TG von Lueder has received lecture honoraria from Novartis, St Jude Medical, AstraZeneca and Vifor Pharma. S Agewall has no conflicts of interest to declare.
References
- Stewart S, MacIntyre K, Hole DJ, et al. More 'malignant' than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail 2001;3:315-22. [Crossref] [PubMed]
- Stewart S, Ekman I, Ekman T, et al. Population impact of heart failure and the most common forms of cancer: a study of 1 162 309 hospital cases in Sweden (1988 to 2004). Circ Cardiovasc Qual Outcomes 2010;3:573-80. [Crossref] [PubMed]
- Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017;135:e146-603. Erratum in: Circulation 2017;135:e646. Circulation 2017;136:e196. [Crossref] [PubMed]
- Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 2013;6:606-19. [Crossref] [PubMed]
- Conrad N, Judge A, Tran J, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet 2018;391:572-80. [Crossref] [PubMed]
- Gerber Y, Weston SA, Redfield MM, et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med 2015;175:996-1004. [Crossref] [PubMed]
- Mentz RJ, Kelly JP, von Lueder TG, et al. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol 2014;64:2281-93. [Crossref] [PubMed]
- Hopper I, Kotecha D, Chin KL, et al. Comorbidities in Heart Failure: Are There Gender Differences? Curr Heart Fail Rep 2016;13:1-12. [Crossref] [PubMed]
- Kjeldsen SE. Hypertension and cardiovascular risk: General aspects. Pharmacol Res 2018;129:95-9. [Crossref] [PubMed]
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2016;18:891-975. [Crossref] [PubMed]
- Agewall S. Adherence to guidelines and registry data. Eur Heart J Cardiovasc Pharmacother 2017;3:183-4. [Crossref] [PubMed]
- Pitt B, Pedro Ferreira J, Zannad F. Mineralocorticoid receptor antagonists in patients with heart failure: current experience and future perspectives. Eur Heart J Cardiovasc Pharmacother 2017;3:48-57. [Crossref] [PubMed]
- Dunlay SM, Weston SA, Jacobsen SJ, et al. Risk factors for heart failure: a population-based case-control study. Am J Med 2009;122:1023-8. [Crossref] [PubMed]
- Cavender MA, Steg PG, Smith SC Jr, et al. Impact of Diabetes Mellitus on Hospitalization for Heart Failure, Cardiovascular Events, and Death: Outcomes at 4 Years From the Reduction of Atherothrombosis for Continued Health (REACH) Registry. Circulation 2015;132:923-31. [Crossref] [PubMed]
- Eskås PA, Heimark S, Eek Mariampillai J, et al. Adherence to medication and drug monitoring in apparent treatment-resistant hypertension. Blood Press 2016;25:199-205. [Crossref] [PubMed]
- Lip GYH, Coca A, Kahan T, et al. Hypertension and cardiac arrhythmias: executive summary of a consensus document from the European Heart Rhythm Association (EHRA) and ESC Council on Hypertension, endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE). Eur Heart J Cardiovasc Pharmacother 2017;3:235-50. [PubMed]
- Jhund PS, Macintyre K, Simpson CR, et al. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: a population study of 5.1 million people. Circulation 2009;119:515-23. [Crossref] [PubMed]
- von Lueder TG, Krum H. Current modalities for invasive and non-invasive monitoring of volume status in heart failure. Heart 2012;98:967-73. [Crossref] [PubMed]
- von Lueder TG, Sangaralingham SJ, Wang BH, et al. Renin-angiotensin blockade combined with natriuretic peptide system augmentation: novel therapeutic concepts to combat heart failure. Circ Heart Fail 2013;6:594-605. [Crossref] [PubMed]
- Wang BH, von Lueder TG, Kompa AR, et al. Combined angiotensin receptor blockade and neprilysin inhibition attenuates angiotensin-II mediated renal cellular collagen synthesis. Int J Cardiol 2015;186:104-5. [Crossref] [PubMed]
- von Lueder TG, Wang BH, Kompa AR, et al. Angiotensin receptor neprilysin inhibitor LCZ696 attenuates cardiac remodeling and dysfunction after myocardial infarction by reducing cardiac fibrosis and hypertrophy. Circ Heart Fail 2015;8:71-8. [Crossref] [PubMed]


