Application of a three-dimensional video system in the training for uniportal thoracoscopic surgery
Introduction
With the development of video-assisted surgery, thoracoscopic surgical procedures had also been popularized and replaced by current open procedures (1). In training for thoracic surgery, video-assisted thoracoscopic surgery (VATS) has been an important curriculum for thoracic surgical training of residents and medical students and crucial for clinical research (2). The acquisition of the basic skills for thoracoscopic surgery has become challenging despite the recent technical advances in endoscopic camera systems, which include high-definition video systems or three-dimensional (3D) video systems that were introduced in the early 1990s (3,4). In addition, with recent widespread application of robotic surgery in thoracic surgery, 3D operative views in robotic surgery provided better surgical fields compared to two-dimensional (2D) views in conventional thoracoscopy (5,6). In addition, recent surgical video systems could also provide real-time 3D views with potential benefits, such as improved depth perception, similar to the current robotic system (7,8). Many studies have reported comparable results between 2D and 3D views for laparoscopic surgery (9-11) and thoracoscopic surgery (12,13). They suggested that the greatest benefit is enhanced depth perception, which enables precise performance of the procedure within shorter procedural times. Moreover, the 3D system has been known to trainees shorten their learning curves for acquiring surgical skills (14).
However, the current 3D video system is still not popular and has not been used regularly in the thoracic surgical field. This might be the result of previous experiences of discomfort when using early 3D video systems, poor image quality, uncomfortable 3D glasses, and low cost-effectiveness in performing VATS (15). In addition, 3D displays did not always present optimized views for every surgeon. Such cases resulted in fatigue, dizziness, and eye disturbances among inexperienced surgeon (8,16). At present, despite the proposed enthusiasm for the use of 3D over 2D displays in endoscopic surgery, conflicting evidence exists, and the benefits of 3D video systems and their potential advantages in endoscopic surgery remains controversial.
Our study aimed to investigate the effectiveness of 3D displays in the training for uniportal VATS procedures because the improved depth perception provided by 3D displays might be accentuated in the uniportal approach. Based on our experiences of uniportal VATS in thoracic surgery since 2012, our center adopted the 3D video system from 2013 to overcome the loss of depth perception. Therefore, we launched the uniportal VATS training program with the 3D video system for surgery residents and medical students. In the uniportal VATS approach, the operative views and instrumentation are quite different from the current conventional multi-port VATS approach (17,18). The major differences include the cranio-caudal direction through the projectile plane of the camera and surgical devices which are similar to the operative view of open thoracotomy (19,20). With such optical differences associated with multiport and uniportal VATS, those who perform uniportal VATS usually encounter hand and eye discordance and require different psychomotor skills because they must perform the VATS procedure in a 3D space guided by 2D displays, which result in a loss of depth perception when using the current conventional 2D video system.
This study aimed at: evaluating the efficiency of 3D displays (in comparison to 2D video systems) in the uniportal VATS simulation for novice surgeons; defining the exact role of 3D video systems in thoracoscopic surgery; and determining its benefits, especially for the uniportal VATS approach.
Methods
Participants
From May 2014 to February 2015, 85 residents in surgical training (first and second year) and 28 medical students who were interested in uniportal endoscopic surgery were enrolled in this study (Table 1). The study was approved by our institutional review board (IRB No. KUGH15143-01). All participants consented by signing a document approved by the institutional board of Korea University Guro Hospital, which explained the study protocols via a survey prior to performing simulation. All participants had no experience of performing endoscopic surgery with 3D video systems. They were asked to complete three tasks in a uniportal endoscopic training module using 2D and 3D views. With limited time, they completed three tasks with alternating 2D and 3D views.
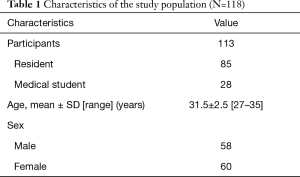
Full table
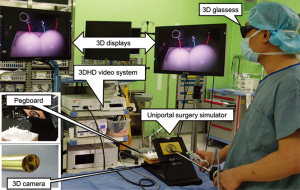
Training modules for uniportal VATS and equipment
Our simulation system consisted of 3-cm single hole board for single incisional laparoscopic surgery (Covidien, Norwalk, CT, USA), training module (pegboard with five pegs and 4-mm ring pins, surgical sutures, and tailor-made skin model for suturing), and endoscopic devices (5-mm endoscopic grasper, dissectors, curved grasper, and endoscopic needle holder). For 2D and 3D views, a surgical video system (Viking Systems, Inc., Westborough, MA, USA) with a 10-mm diameter 0° thoracoscope was used by alternating 2D and 3D vision in each task. Dual high-definition video monitors (32 inch; Sony, Japan) were used. All participants wore passive, polarized glasses to view 3D images during 3D tasks. The monitors were placed at 200 cm and 150 cm from the ground to maximize the imaging perception (Figure 1).
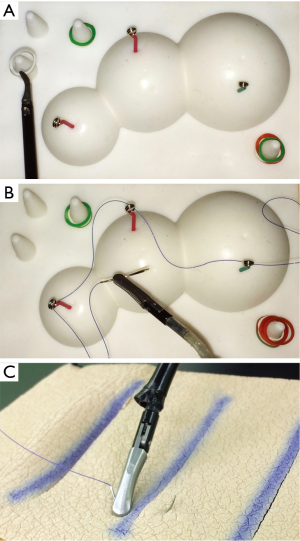
Task description
Three surgical tasks, based on the Fundamental Laparoscopic Surgery Program, were completed by all participants to evaluate their performances in the basic endoscopic skills using 3D views. Task 1 was peg transfer within 200 s. Five rubber rings were placed on the right-side pole of the pegboard, and these rings should be transferred to the poles positioned on the left side by using endoscopic graspers (Figure 2A). Timing for this task began when the participants touched the first ring and ended upon completion of the last ring. Task 2 was needle (curved 3-0) transfer through four small holes (3-mm diameter) from left to right using needle holder or grasper (Figure 2B). The time limit was 300 s, and timing began upon grasping the needle and ended upon passing the last hole. Task 3 was suturing within 100 s in a tailor-made skin model prepared with 2-mm thick polyurethane patch to mimic the tactile property of real skin (Figure 2C). The completion time for participants to place a single stitch with an endoscopic needle holder was recorded in this task. All participants performed the three tasks, each using a 2D and a 3D view.
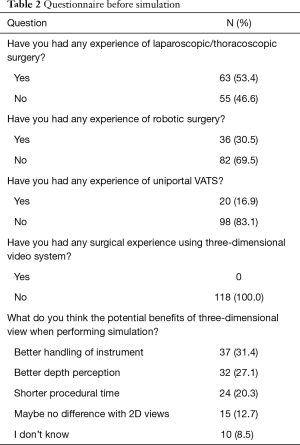
Surveillance of subjective data
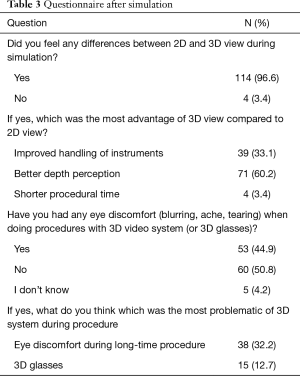
All participants enrolled in this study completed questionnaires before and after simulation. Before simulation, the participants were asked about their previous experiences of 3D views during surgery, VATS, robotic surgery, and predicted benefits or disadvantages of 3D system in training. After completion of all tasks, questions included subjective rating of visual quality of 3D compared to 2D, depth perception, any discomfort including eye burn, ache, or tearing, and other physical discomfort.
Statistical analysis
Two parameters, namely, completion time and failure rate in each task performed in the 2D and 3D views, were compared using the paired t-test. Statistical analysis was performed using GraphPad software (version 6, GraphPad software, Inc., CA, USA), and statistical significance was defined as P<0.05.
Results
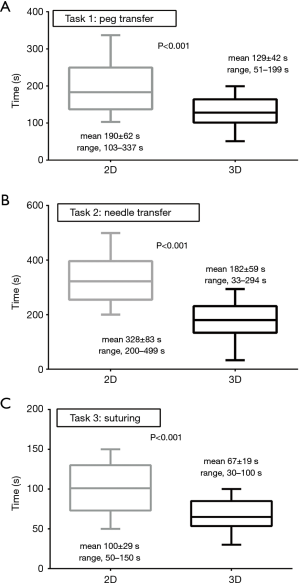
In pre-simulation survey, the participants responded that expected benefits of 3D video system compared to 2D were better handling of instrument (n=37, 31.4%), better depth perception (n=32, 27.1%), and shorter procedural time (n=24, 20.3%) (Table 2). At simulation, the mean performance time decreased in all tasks using 3D video system (Figure 3). In task 1, 37 participants (31.4%) could not complete the task within 200 s using 2D video system. Using 3D video system, 92 participants (80.0%) showed improved performance time (mean, 129±42 s) compared to 2D (mean, 190±62 s; P<0.001), and all participants completed the task within the time limit (P<0.001). In task 2, 102 participants (86.4%) showed shorter performance time (mean, 182±59 s) and lower failure rate within the time limit (n=5) when using 3D compared to 2D (mean, 328±83 s; P<0.001) in which 45 participants failed (38.1%; P<0.001). Moreover, using the 2D video system, 60 participants (50.8%) could not perform task 3 within 100 s, and the mean performance time was 100±29 s. However, in the 3D system, all participants completed the task within 100 s (mean, 67±19 s; P<0.001) and 30 (25.4%) showed shorter performance time (P<0.001).
Full table
On post-simulation survey, participants answered that the differences were improved depth perception (n=71, 60.2%), improved handling of instrument (n=39, 33.1%), and shorter procedural time (n=4, 3.4%). Sixty participants (50.8%) felt no discomfort with 3D view and wearing 3D glasses. However, 53 (44.9%) reported visual discomfort including eye fatigue, blurred vision, and tearing during simulation in 3D view (Table 3). There was no physical deterioration among participants during simulation using 3D video system.
Full table
Discussion
Three-dimensional display has been evaluated in various simulation programs and clinical studies in order to define its exact role in surgery (21,22). To date, studies comparing 2D and 3D video systems using different surgical simulation models suggested that 3D vision could provide improved depth perception when performing endoscopic surgery and it is advantageous for shorter procedural time (10,23).
To our knowledge, no previous study evaluating 3D video system under uniportal environment has ever been reported. We hypothesized that described benefits of 3D views (especially improved depth perception) might be determined by individuals performing uniportal surgical simulation. In this study, the use of 3D video system during uniportal simulation showed improved procedural times and success rate of the surgical skill within a limited time in novice who had no experience of endoscopic and robotic surgery. This implicate that 3D video system might benefit trainees during the initial learning period. Moreover, many participants wearing 3D glasses could view the actual surgical field in 3D, which is advantageous for surgical training. Studies on the effectiveness of simulated training also had suggested that using 3D displays improved surgical performance for both surgeons and trainees (10). Enhanced depth perception is remarkable when performing very delicate surgical procedures, such as dissection of pulmonary vessel or lymph node or suturing of vessel or bronchus, because of the projectile instrumental movement in different optical views in uniportal environment than in conventional multi-port VATS. In addition, uniportal thoracoscopic surgery is a challenging approach even for experienced multi-port VATS surgeon. Specific training from experienced uniportal VATS surgeon is required to perform complex procedures such as bronchoplastic or vascular reconstruction. Three-dimensional views might be helpful to a surgeon in training these complex procedures through uniportal approach because the depth perception is limited due to parallel movement of the instruments.
Nevertheless, the results of our post-simulation survey indicated that 3D displays might produce eye discomfort during simulation (15) even within a short time period. Subjective data regarding physical stress, especially in the eye, was one of the major limitations, although recent 3D devices had changed to simple eyeglasses from initial heavy, bulky head-mounted devices. Such eye discomfort including visual blurring, pain, or tearing might not be clinically significant and even could be decreased with repeated training.
There have been conflicting evidences in clinical application of 3D displays because most major surgeries in VATS might need more than 2–3 h of wearing 3D glasses despite different individual responses to physical stress by 3D displays. On the contrary, recent studies have indicated that 3D display has many advantages, such as improved performance time and short learning curve, at least in using simulation module in novices (24). For training of basic techniques in uniportal surgery, a trainee should be familiar with the geometric characteristics of the uniportal surgical field, which is different from those of multi-port thoracoscopic surgery. The instrument or scope moves in a parallel manner during uniportal surgery, and this provides direct view of the scope in the same direction, mimicking the open surgery. In such situation, 3D views might help the trainee to practice the uniportal surgery with improved depth perception and enhanced target discrimination.
The actual advantage of 3D displays in the actual surgical field is yet to be established (8,25,26). The stereoscopic view could offer a precise operative field and improved surgical performance (27). However, mostly, these outcomes have been reported from their 3D experiences during laparoscopic surgery. For thoracoscopic surgery, a few studies had described the utilization of 3D system and showed a minor effect on VATS surgery. Currently, it has been reported that a major VATS procedure (such as lobectomy) could be performed with less surgical time using a 3D video system. Moreover, no significant difference was found in perioperative outcomes such as complication, blood loss, chest drainage, hospital stay, and mortality (12,28). Potentially, we could assume that 3D views during VATS lobectomy might be advantageous for systemic lymph node dissection, which is an essential part of lung cancer surgery from the experiences of 3D views in robotic surgery. However, the number of lymph node dissected was not different between 2D and 3D VATS in randomized trials and observational studies (13). Until now, except for shortening operation times, it is unclear whether 3D video systems are superior to 2D systems in the actual surgical field. In addition, experienced surgeons who were familiar with 2D displays might not prefer the unfamiliar 3D displays due to a significant side effect attenuated in a long operation time. Nonetheless, 3D display, although it was not widespread among real surgical field and even among active VATS surgeons, has potential benefits as surgical tool in future technical development such as 3D high-definition display without 3D glasses (29).
The limitations of this study are its study design, procedures performed, and presented questions during simulation course. We designed our study for junior resident and medical students who have few experiences of VATS or laparoscopic surgery. Hence, the simulation tasks were composed of relatively basic procedures because the participants could not handle the endoscopic devices appropriately through a 3-cm single port for the first time. In our study, we measured the completion time at each task only once in both 2D and 3D views without interval to minimize the learning effect of the prior task. However, the learning effect of prior tasks in 2D view might affect the study result in 3D view. In addition, we surveyed the subjective experiences of participants after simulation. The scoring or grading was not used in the survey form to evaluate their symptoms, such as eye discomfort or inconveniences, because our aim was to evaluate the first impression and the feasibility of 3D views during simulation among the participants. We considered that the scoring or grading of ocular symptoms might not be appropriate for relevant outcomes in our study.
In conclusion, compared to the 2D video system, the 3D video system showed improved performance time and reduced the number of errors in uniportal VATS simulation. Subjective data among participants in this study also indicated that 3D displays are advantageous for uniportal VATS simulation with better depth perception and better handling of endoscopic devices, especially for trainees. The physical stress associated with using 3D views, such as eye discomfort, should be resolved in the current 3D endoscopic systems. Future studies are needed to evaluate the benefits of 3D displays in the actual surgical field among experienced VATS surgeon.
Acknowledgements
Funding: This work was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI17C0654), and a National Research Foundation of Korea (NRF) grant funded by the Ministry of Education, Science and Technology (NRF-2015R1A2A2A04005760).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by our institutional review board (IRB No. KUGH15143-01). All participants consented by signing a document approved by the institutional board of Korea University Guro Hospital, which explained the study protocols via a survey prior to performing simulation.
References
- Whitson BA, Andrade RS, Boettcher A, et al. Video-assisted thoracoscopic surgery is more favorable than thoracotomy for resection of clinical stage I non-small cell lung cancer. Ann Thorac Surg 2007;83:1965-1970. [Crossref] [PubMed]
- Rocco G, Internullo E, Cassivi SD, et al. The variability of practice in minimally invasive thoracic surgery for pulmonary resections. Thorac Surg Clin 2008;18:235-47. [Crossref] [PubMed]
- Hagiike M, Phillips EH, Berci G. Performance differences in laparoscopic surgical skills between true high-definition and three-chip CCD video systems. Surg Endosc 2007;21:1849-54. [Crossref] [PubMed]
- Buchs NC, Volonte F, Pugin F, et al. Three-dimensional laparoscopy: a step toward advanced surgical navigation. Surg Endosc 2013;27:692-3. [Crossref] [PubMed]
- Kent M, Wang T, Whyte R, et al. Open, video-assisted thoracic surgery, and robotic lobectomy: review of a national database. Ann Thorac Surg 2014;97:236-42; discussion 42-4. [Crossref] [PubMed]
- White YN, Dedhia P, Bergeron EJ, et al. Resident training in a new robotic thoracic surgery program. J Surg Res 2016;201:219-25. [Crossref] [PubMed]
- Kong SH, Oh BM, Yoon H, et al. Comparison of two- and three-dimensional camera systems in laparoscopic performance: a novel 3D system with one camera. Surg Endosc 2010;24:1132-43. [Crossref] [PubMed]
- Sørensen SM, Savran MM, Konge L, et al. Three-dimensional versus two-dimensional vision in laparoscopy: a systematic review. Surg Endosc 2016;30:11-23. [Crossref] [PubMed]
- Collins D, Ashraf A, Whelan M, et al. 3-Dimensional (3D) vs 2-Dimensional (2D) Simulation Enhances Surgical Skills in Standardized Laparoscopic Tasks. J Am Coll Surgeons 2014;219:S114-S5. [Crossref]
- Cologne KG, Zehetner J, Liwanag L, et al. Three-dimensional Laparoscopy: Does Improved Visualization Decrease the Learning Curve Among Trainees in Advanced Procedures? Surg Laparosc Endosc Percutan Tech 2015;25:321-3. [Crossref] [PubMed]
- Chiu CJ, Lobo Prabhu K, Tan-Tam CC, et al. Using three-dimensional laparoscopy as a novel training tool for novice trainees compared with two-dimensional laparoscopy. Am J Surg 2015;209:824-7 e1; discussion 7.
- Yang C, Mo L, Ma Y, et al. A comparative analysis of lung cancer patients treated with lobectomy via three-dimensional video-assisted thoracoscopic surgery versus two-dimensional resection. J Thorac Dis 2015;7:1798-805. [PubMed]
- Xu Y, Chen N, Ma A, et al. Three-dimensional versus two-dimensional video-assisted thoracic surgery for thoracic disease: a meta-analysis. Interact Cardiovasc Thorac Surg 2017;25:862-71. [Crossref] [PubMed]
- Cicione A, Autorino R, Laguna MP, et al. Three-dimensional Technology Facilitates Surgical Performance of Novice Laparoscopy Surgeons: A Quantitative Assessment on a Porcine Kidney Model. Urology 2015;85:1252-6. [Crossref] [PubMed]
- Sakata S, Watson MO, Grove PM, et al. The Conflicting Evidence of Three-dimensional Displays in Laparoscopy: A Review of Systems Old and New. Ann Surg. 2016;263:234-9. [Crossref] [PubMed]
- Ko JK, Li RH, Cheung VY. Two-dimensional versus three-dimensional laparoscopy: evaluation of physicians' performance and preference using a pelvic trainer. J Minim Invasive Gynecol 2015;22:421-7. [Crossref] [PubMed]
- Bertolaccini L, Rocco G, Pardolesi A, et al. The Geometric and Ergonomic Appeal of Uniportal Video-Assisted Thoracic Surgery. Thorac Surg Clin 2017;27:331-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5 Suppl 3:S234-45. [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [PubMed]
- Bertolaccini L, Rizzardi G, Terzi A. Single-port video-assisted thoracic surgery resection: the Copernican revolution of a geometrical approach in thoracic surgery? Interact Cardiovasc Thorac Surg 2011;12:516. [Crossref] [PubMed]
- Feng X, Morandi A, Imvised T, et al. Three-Dimensional Versus Two-Dimensional Imaging in Adult Versus Pediatric Laparoscopy: A Simulator Box Study. J Laparoendosc Adv Surg Tech A 2015;25:1051-6. [Crossref] [PubMed]
- Zdichavsky M, Schmidt A, Luithle T, et al. Three-dimensional laparoscopy and thoracoscopy in children and adults: A prospective clinical trial. Minim Invasive Ther Allied Technol 2015;24:154-60. [Crossref] [PubMed]
- Alaraimi B, El Bakbak W, Sarker S, et al. A randomized prospective study comparing acquisition of laparoscopic skills in three-dimensional (3D) vs. two-dimensional (2D) laparoscopy. World J Surg 2014;38:2746-52. [Crossref] [PubMed]
- Tanagho YS, Andriole GL, Paradis AG, et al. 2D versus 3D visualization: impact on laparoscopic proficiency using the fundamentals of laparoscopic surgery skill set. J Laparoendosc Adv Surg Tech A 2012;22:865-70. [Crossref] [PubMed]
- Wagner OJ, Hagen M, Kurmann A, et al. Three-dimensional vision enhances task performance independently of the surgical method. Surg Endosc 2012;26:2961-8. [Crossref] [PubMed]
- Gurusamy KS, Sahay S, Davidson BR. Three dimensional versus two dimensional imaging for laparoscopic cholecystectomy. Cochrane Database Syst Rev 2011. [PubMed]
- Chan AC, Chung SC, Yim AP, et al. Comparison of two-dimensional vs three-dimensional camera systems in laparoscopic surgery. Surg Endosc 1997;11:438-40. [Crossref] [PubMed]
- Dong S, Yang XN, Zhong WZ, et al. Comparison of three-dimensional and two-dimensional visualization in video-assisted thoracoscopic lobectomy. Thorac Cancer 2016;7:530-4. [Crossref] [PubMed]
- Kyriazis I, Ozsoy M, Kallidonis P, et al. Integrating Three-Dimensional Vision in Laparoscopy: The Learning Curve of an Expert. J Endourol 2015;29:657-60. [Crossref] [PubMed]