Original “double-step” technique for large superior sulcus tumors invading the anterior chest wall without subclavian vessels involvement
Introduction
In N0-1 non-small cell lung cancer (NSCLC) infiltrating the chest wall, en-bloc chest wall and lung resection generally leads to satisfactory oncologic results, provided that wide clear margins have been achieved (1). The surgical approach is selected on the basis of different parameters and particularly for superior sulcus tumors, the choice of surgical access is variable, depending on the tumor infiltration site and anatomical structures involved. An ideal surgical approach has yet to be defined for patients with very large lung tumors which infiltrate anteriorly the first ribs without subclavian vessels invasion. For these uncommon situations we have developed a simple "double-step" technique to facilitate resection and reduce surgical trauma. The possible bony thorax reconstruction is also facilitated.
The technique and the preliminary experience are herein described.
Methods
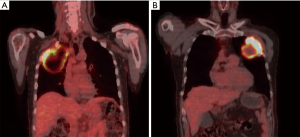
From 2010 to 2017, five patients with large size cN0-1M0 non-small cell lung cancer with apical anterior chest wall invasion were successfully treated using the technique described below. Four out of five patients had a Superior Sulcus tumor involving for infiltration of the second rib or above. All patients were scheduled for en-bloc lobectomy and chest wall resection after a standard preoperative work-up, including a complete blood count, biochemical blood analyses, and blood gas analyses. Cardiovascular and respiratory functions were inspected by electrocardiography, Doppler echocardiography, and pulmonary tests. The clinical stage was assessed through chest X-rays, total body contrast computed tomography (CT), videobronchoscopy, and a fluorodeoxyglucose positron emission tomography (FDG-PET) scan. Infiltration of the subclavian vessels was excluded with Magnetic Resonance Imaging in three of the patients. Preoperative histological diagnosis was performed through trans-thoracic needle biopsy. Cisplatinum-based induction chemoradiotherapy was administered in all cases, except in two patients with infected cavitating tumors (Figure 1) who had undergone primary surgery. Patients undergoing induction treatment were then re-staged at the end of treatment with CT and/or FDG-PET.
Technique
First step: anterior access
The patient is placed in a supine position. Through a short longitudinal parasternal incision the medial limit of the thoracectomy is exposed. The cartilages of the involved ribs are sectioned, transecting the first rib using by a Gigli saw, at its costochondral junction beneath the medial attachment of the clavicle (2). The anterior scalene muscle is sectioned, caudally pulling the first rib stump.
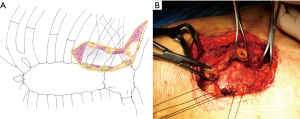
Before wound closure, a variable number of heavy non-absorbable stitches are placed through the peristernal tissues and temporarily left inside the chest. These stitches will provide a solid medial fixation of the prosthesis (Figure 2A,B).
Second step: posterior access
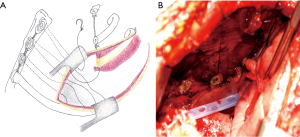
A Shaw-Paulson thoracotomy is performed, allowing full exposure of the posterior limit of the thoracectomy. The entire first rib is quickly resected as its costochondral junction has already been sectioned and the stump has become relatively mobile. The lung attached to the resected ribs can be rotated inside the chest so that the lobectomy and mediastinal node dissection are accomplished without hindrance. After the radical en-bloc lung and chest wall resection has been completed, the stitches placed on the peristernal tissues are collected and used to anchor the medial edge of the prosthesis (Figure 3A,B), which is then fixed under tension to the lateral and inferior edges of the defect.
Results
Maximum tumor diameter ranged from 65 to 102 mm (>7 cm in four patients). Pathological staging showed: four tumors pT4N0 and 1 tumor pT3N1 according to IASCL 8th TNM edition. Complete resection was achieved with upper lobectomy en-bloc with a wide thoracectomy involving I-II-III rib (four patients) and II-III-IV rib (one patient). All patients underwent prosthetic reconstruction of the extensive anterior chest wall defect using a polypropylene mesh or a PTFE soft patch. Histology showed: four primary pulmonary adenocarcinomas and one squamous carcinoma G1. Neither significant flail chest nor postoperative respiratory complications were observed; two patients with preoperative low pulmonary reserve received a mini-tracheostomy (Portex® Minitrach II MT, Smiths Medical International Ltd., Hythe, UK) positioned at the end of the procedure and removed on postoperative day 8.
Discussion
Superior sulcus tumors (SST) which do not require surgical exposure of the subclavian vessels are commonly managed with a posterior approach, even in the case of anterior infiltration of the bony thorax (3). Technical problems can occur in the management of very bulky tumors infiltrating the anterior bony thorax, as the large mass can hide the anterior limits of the chest wall infiltration, particularly if approached posteriorly (4), therefore making this surgical route inadvisable or unsuitable. Tatsumura (5) proposed extending the posterior incision anteriorly and upwards to the nipple, so as to expose the sternoclavicular joints, but this approach is rarely chosen because of its invasiveness. Accordingly, for these types of situations there are no reasonable alternatives to an anterior approach. A variety of transmanubrial or transclavicular approaches have been described for the treatment of SST invading the anterior compartment of the thoracic inlet (6,7). Though providing excellent exposure to the subclavian vessels, these incisions damage the sternum and/or clavicle and generally do not allow the best access to the radical lobectomy, which could be performed through the hole resulting from the chest wall resection or through further enlargement of the incision (8). Therefore, traumatic anterior access, which damages the sternum or clavicle, is futile if the complete exposure of subclavian vessels is not required. Furthermore, most anterior incisions do not allow the correct handling of the mass correctly, especially when a large tumor attached to the resected ribs is released within the chest.
A combination of surgical accesses may be indicated, even though additional surgical trauma must be imposed (9). In order to reduce the invasiveness of the procedure, the combination of a VATS approach with an anterior incision might be a reasonable alternative, although this choice is appropriate mainly for relatively small tumors requiring a limited thoracectomy (10). Certainly the large size of the mass attached to multiple resected ribs is an obstacle for the VATS approach.
We began to develop our technique based on the fact that the first rib can be interrupted at its costo-chondral junction by a minimal subclavicular incision (2), thus preserving the shoulder function and the integrity of the sternum and clavicle. We adopted this technical practice to reduce the surgical invasiveness in selected patients and to make the procedure easier. The only drawback of our technique is related to the change of the patient’s position. After the involved ribs have been sectioned anteriorly, the en-bloc lung-chest wall resection is simply completed through the subsequent Shaw-Paulson thoracotomy, which allows the straightforward handling of very large masses.
Indeed, both the anterior and posterior incisions have their advantages.
The limited anterior incision allows:
- transection of the first rib at the costochondral junction, leaving the sternum and clavicle intact;
- ideal exposure of the anterior chest wall infiltration;
- easy conversion into a transmanubrial approach, if required by the intraoperative findings.
The sequential posterior access allows:
- easy posterior rib section, especially at the level of the first rib;
- undemanding upper lobectomy and en-bloc chest wall resection.
Chest wall reconstruction is a matter of choice in these situations and most of the apical bony thorax defects are generally left unrepaired. However, extensive anterior chest wall resection may cause physiological and cosmetic damage, which can be prevented through a reliable reconstruction. The proposed technique makes the potential reconstructive phase easier and more effective. In our experience, reconstruction with non-rigid prosthesis was generally adequate to avoid the postoperative paradox and to achieve an acceptable cosmetic result. In fact, the use of a rigid curved prosthesis is not mandatory for the reconstruction of an apical-anterior defect since the shape of the chest, at the apical level, is determined by the shoulder girdle structures rather than by the bony thorax.
We found the procedure valid and effective, even in a patient with a very large lung tumor infiltrating anteriorly the chest wall, which was not classifiable as a “Pancoast Tumor” as it did not invade the tissues above the second rib. In this case the procedure was even easier because it was not necessary to resect the first rib.
Acknowledgements
None.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: According to National and institutional regulations patients have signed informed consent for data review. Institutional ethic board allowed for retrospective data analysis and publication for scientific purposes.
References
- Puma F, Vannucci J. Chest Wall Resection/Reconstruction for Tumors. In: Mathisen DJ, Morse C. Master Techniques in Surgery: Thoracic Surgery: Transplantation, Tracheal Resections, Mediastinal Tumors, Extended Thoracic Resections. Wolters Kluwer, 2014.
- Murphy TO, Piper CA, Kanar EA, et al. Subclavicular approach to first rib resection. Am J Surg 1980;139:634-6. [Crossref] [PubMed]
- Nikolaos P., Vasilios L, Efstratios K, et al. Therapeutic modalities for Pancoast tumors. J Thorac Dis 2014;6 Suppl 1:S180-93. [PubMed]
- Parissis H, Young V. Treatment of Pancoast tumors from the surgeons prospective: re-appraisal of the anterior-manubrial sternal approach. J Cardiothorac Surg 2010;5:102. [Crossref] [PubMed]
- Tatsumura T, Sato H, Mori A, et al. A new surgical approach to apical segment lung diseases, including carcinomas and inflammatory diseases. J Thorac Cardiovasc Surg 1994;107:32-6. [PubMed]
- Dartevelle PG, Chapelier AR, Macchiarini P, et al. Anterior transcervical-thoracic approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 1993;105:1025-34. [PubMed]
- Grunenwald D, Spaggiari L. Transmanubrial osteomuscular sparing approach for apical chest tumors. Ann Thorac Surg 1997;63:563-6. [Crossref] [PubMed]
- Masaoka A, Ito Y, Yasumitsu T. Anterior approach for tumor of the superior sulcus. J Thorac Cardiovasc Surg 1979;78:413-5. [PubMed]
- Foroulis CN, Zarogoulidis P, Darwiche K, et al. Superior sulcus (Pancoast) tumors: current evidence on diagnosis and radical treatment. J Thorac Dis 2013;5 Suppl 4:S342-58. [PubMed]
- Yokoyama Y, Chen F, Aoyama A, et al. Combined operative technique with anterior surgical approach and video-assisted thoracoscopic surgical lobectomy for anterior superior sulcus tumours. Interact Cardiovasc Thorac Surg. 2014;19:864-6. [Crossref] [PubMed]


