Xiphoid-sparing midline sternotomy reduces wound infection risk after coronary bypass surgery
Introduction
Midline sternotomy was first described by Milton in 1897 (1). The Milton procedure remained unused until it was recommended by Julian et al. in the 1950s (2). Since then, midline sternotomy has become the most common approach for coronary artery bypass surgery (1-3). It provides full access to almost all mediastinal structures and to all branches of the coronary system. Moreover, it is easily performed and learned by younger surgeons, and is well tolerated by patients. In the last two decades, many surgeons have applied partial sternotomy (upper or lower) for minimal access cardiac surgery; however, the role of this approach in reducing sternal wound infections is unclear (4,5). Midline sternotomy is also preferred by many thoracic surgeons (6). Manubrium-sparing midline sternotomy is less utilized and is usually performed to provide better cosmetic results compared to standard sternotomy (7). Mainly due to biomechanical factors, physical activity after midline sternotomy always results in varying amounts of lateral distraction between the sternal edges. Because immobilization is mandatory for bony union, the wound healing of full midline sternotomy is likely to be less optimal compared with that of orthopaedic fractures (8). Additionally, the wound healing of this approach majorly depends on many risk factors, which may affect the stabilization or circulation state of the healing sternum (9). The cartilaginous xiphoid process (XIP) is usually avascular. Consequently, wound healing in the region of the xiphoid could be slower compared to other segments of the sternum. A study of cadaveric humans showed a greater displacement at the xiphoid region than at other segments of the sternum, with lateral distraction after midline sternotomy (10). In this study, we aimed to clarify if the preservation of XIP with its muscular attachment may play a role in improving the healing process after midline sternotomy and reducing the risk of deep sternal wound infections (DSWIs).
Methods
Study design
The study was conducted in accordance with the Declaration of Helsinki and was approved by the regional ethics committee (approval No. 10/2018). Clinical data were collected from the hospital record system at St. Rafael Zala County Hospital, Zalaegerszeg, Hungary. We included only patients who underwent coronary artery bypass grafting by one surgeon, with the use of the left internal thoracic artery via midline sternotomy. We excluded all patients who underwent harvesting of the right or bilateral internal thoracic artery, minimally invasive direct coronary artery bypass grafting, coronary revascularization alone with venous conduits, surgeries other than coronary artery bypass grafting, and redo operations. A preliminary retrospective analysis of data from 202 cardiac surgical patients that underwent coronary bypass grafting with the left internal thoracic artery by one surgeon from 2007–2011 (preliminary group) was conducted to ascertain the prevalence of DSWI. Following, we conducted a cohort study to estimate the impact of the preservation of XIP unit integrity on the development of DSWI; data from 244 patients, who were operated by the same surgeon and met the criteria for inclusion in the period between January 2012 and May 2017 (contemporary group) were prospectively collected and retrospectively analyzed.
No structural differences were made or observed between the preliminary and contemporary groups. Prophylactic antibiotic therapy was the same in both groups.
Definitions
DSWIs were defined in accordance with the Centers for Disease Control and Prevention guidelines (11). We defined the “XIP unit” as the anatomical unit, which consists of the bony-cartilaginous anatomical XIP and its muscular attachments, the bifurcation of the internal thoracic artery and the skin overlying the XIP. XIP-sparing sternotomy was defined as midline sternotomy with the preservation of the XIP unit. Standard midline sternotomy was defined as midline sternotomy without the preservation of the XIP unit.
Surgical technique
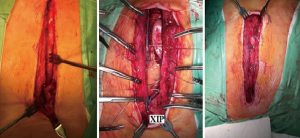
During XIP-sparing midline sternotomy, a skin incision was made from the jugular notch to just above the border of XIP. Soft tissue between the right 7th costal cartilage and XIP was bluntly dissected to ensure the hooking of the power saw. The sternum was then cut first to the midline of the sternum, then upwards till the jugular notch, in a “J” shape. The left internal thoracic artery was harvested from its origin to just above its bifurcation. Sternal closure was performed with eight sternal wires in a crisscross formation without introducing wires through the XIP (Figures 1,2).
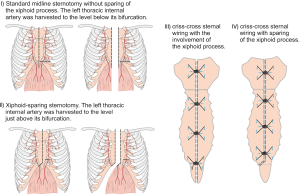
In the standard longitudinal midline sternotomy, the skin incision ended below the lower edge of XIP. Midline sternotomy was initiated at the jugular notch and continued downwards to cut XIP in the middle. The left internal thoracic artery was then harvested from its origin to the level below its bifurcation. Sternal wires were also introduced into XIP to reunite the split XIP halves (Figure 1).
Statistical analysis
Continuous variables are expressed as mean ± standard deviations and categorical variables as percentages. The Chi-square test was used to compare the prevalence of DSWI between the XIP-sparing and traditional sternotomy group. The differences in the baseline and operative characteristics of the patients in both groups were compared using the independent sample t-test for continuous variables and the Chi-square test for categorical variables. To reduce the impact of treatment selection bias and potential confounding, we balanced the distribution of covariates between the XIP-sparing and traditional sternotomy groups with the inverse probability of treatment weighting (IPTW). Using XIP unit sparing as a dependent variable, related outcomes and confounding (related to treatment) covariates (obesity, diabetes mellitus, chronic obstructive pulmonary disease, peripheral vascular disease, red blood cells transfusion, combined procedures, fresh frozen plasma transfusion) were included in the binary logistic regression analysis to compute the propensity score. The model was well calibrated according to the Hosmer-Lemeshow test (P=0.912). During the calculation of weighted samples, the weight for patients in the XIP-sparing group was inverse propensity score; and the weight for patients in the traditional sternotomy group was the inverse of 1-propensity score. The mean weight was 2.27±0.97. For adjusting the inflating effect of sample size to original sample size, a robust method, the Generalized Linear Model was applied in order to calculate variance and covariance in the weighted sample. To estimate the treatment effect of XIP sparing on the development of DSWI, a binary logistic model was used. All reported P values are two-sided, and P<0.05 was considered statistically significant. Statistical analysis was performed using SPSS for Windows version 20.0 (IBM Corp., Armonk, NY, USA).
Results
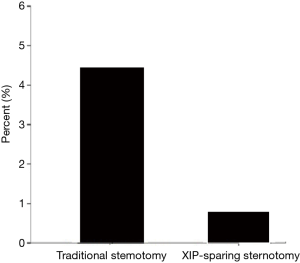
There were no significant differences in the rates of DSWI in our institution between all patients, underwent coronary bypass grafting by all surgeons, in the preliminary and contemporary groups, 3.8% (72/1,903) and 4.8% (68/1,412), respectively (P=0.162). Among the study population, the DSWI rates decreased from 4.5% (standard sternotomy, preliminary group) to 0.8% (XIP-sparing sternotomy, contemporary group) (P=0.014), (Figure 3).
Baseline and operative characteristics and clinical outcome data of the patients in the XIP-sparing and standard sternotomy groups are shown in Table 1. The number of freshly frozen plasma transfusions and combined procedures was higher in the XIP group. These variables were included as confounding variables in the binary logistic regression analysis during the computation of the propensity score.
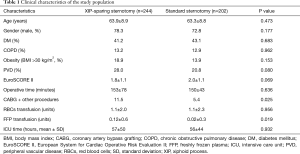
Full table
Based on the binary logistic model using inverse propensity score-weighted samples, the XIP-sparing approach had a significant therapeutic impact on DSWI rates after coronary artery surgery compared to standard sternotomy. The adjusted odds ratio of DSWI in the XIP sparing-group was 0.171 (95% confidence interval, 0.036–0.806, P=0.026).
Discussion
In our surgical experience, discharge from the sternal wounds appears, in most cases, at the lower part of these wounds. This observation led us to suspect the possible role of XIP in the development of these wounds. Instead of traditional midline sternotomy, patients in the contemporary group underwent XIP-sparing sternotomy. Although DSWI rates among all patients underwent coronary bypass grafting via midline sternotomy in our institution did not differ significantly in the preliminary and contemporary period, XIP-sparing sternotomy in this study population contributed to significant decrease in DSWI rates.
The prevalence of midline sternotomy as the most commonly used surgical approach in open heart surgery has resulted in post-sternotomy deep wound infections remaining a major challenge. Recently, there have been several efforts to reduce the prevalence of wound infections. These preventive measures were initially introduced in other fields of surgery and were subsequently employed in cardiac surgery. Platelet-rich autologous plasma, gentamycin-coated sponge or vancomycin paste, or incisional negative pressure wound therapy are among those approaches that reportedly reduce the risk of wound infections (12-18). However, these measures do not target the surgical technique, which is a non-negligible risk factor, but are rather aimed at reducing microbiological contamination or promoting wound granulation. It is well known that surgical technique can markedly affect the risk of wound infection (19). In this respect, wound infections after sternotomy can be distinguished from infections that develop at the sites of other surgical incisions. The peculiarities of median sternotomy show that risk factors such as chronic pulmonary disease, obesity, or peripheral vascular disease have a greater impact on the healing process of sternal wounds compared to other wounds.
The division of the sternum by an oscillating saw is usually standardized; however, the methods for reuniting the sternal halves are diverse. Sternal reunion can be performed by wires or plates. Wires can be used as simple or figure-of-eights and passed transsternally or peristernally, and in the horizontal or longitudinal direction (20,21). The main endpoint is to reach an unimpaired ossification of the divided sternum, which will result in a biomechanically stable thorax and uncompromised wound healing. To reach this goal, sternal wound infection should be prevented because if infection ensues, the bone healing process would be interrupted and dehiscence of the sternal halves would develop. Sternotomy closure with wires may not provide a perfectly stable osteosynthesis and sternal plating may be one of the preventive approaches that target the surgical technique, and it reportedly reduces the risk of sternal wound infections in high-risk patients (22).
XIP is usually cartilaginous in the adult. If it ossifies, the ossification process is usually more visible at the margins, with the core remaining cartilaginous (23,24). The healing process of cartilage tissue usually differs from that of bone. This is mainly because cartilage is avascular and the repair process after damage of this tissue type is slow (25). Lachman et al. reported the existence of a xiphoid branch deriving from a trifurcation of the internal thoracic artery (26). However, in most cases, the cartilage still has no or little direct blood supply. We considered that dividing XIP in the middle would possibly result in poor cartilage healing and cartilage necrosis may develop. This may be one of the initial steps that trigger infections of sternal wounds. We supposed that sparing the cartilaginous XIP with its muscle attachments, anteriorly to the linea alba and abdominal rectal muscle and posteriorly to the diaphragm, during midline sternotomy, would assist in reducing the risk of sternal wound infections.
Unfortunately, patients whose bilateral internal thoracic arteries were harvested were excluded from our study as they composed only 1% of the total patient population that underwent coronary bypass grafting in our institution. In our opinion, apart from the basic factors of bacterial colonization and risk factors, both biomechanical and microvascular conditions are responsible for the development of DSWI.
DSWIs are rare but serious complications after coronary artery bypass surgery performed via midline sternotomy. In addition to its impact on morbidity, mortality, and hospital costs, DSWI reduces the survival rate after coronary bypass surgery (27). This is an especially important issue in the era when long-term survival after surgical revascularization has been emphasized as the main goal in almost all reports dealing with complete arterial revascularization (28,29). Sternal wound infections, as other surgical wound infections, have also a significant impact on patients’ psychological and social status (30). Thus, we suggest that applying a combination of measures to prevent DSWIs is a substantial step towards maintaining the advantages of surgical revascularization.
Recently, we considered XIP as a complex anatomical unit, which consists of the bony-cartilaginous anatomical XIP and its muscular attachments. Conversion from traditional to XIP-sparing midline sternotomy led to significant decrease in DSWI rates in this study population.
Limitations
In addition to the known limitations of retrospective studies, the following should be considered when interpreting the above results. First, the exclusion of patients who underwent bilateral internal thoracic artery harvesting and coronary bypass grafting with only venous conduits may limit the generalizability of the above findings. Second, the study lacked randomization; however, inverse probability weighting was used to minimize this bias. These methods allowed us to account for only the measured variables and the estimates of treatment effect may be susceptible to bias due to unknown and unmeasured confounding variables. Third, the data were derived from a single institution. A prospective randomized study to assess the role of XIP unit preservation in reducing DSWI rates with broader inclusion criteria should provide more accurate information regarding our findings.
Conclusions
The decrease in DSWI rates after XIP-sparing midline sternotomy underpins the important of XIP unit preservation during midline sternotomy. In our patients, midline sternotomy with XIP unit preservation did not restrict access to any anatomical structure during surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was conducted in accordance with the Declaration of Helsinki and was approved by the regional ethics committee (approval No. 10/2018).
References
- Dalton ML, Connally SR. Median sternotomy. Surg Gynecol Obstet 1993;176:615-24. [PubMed]
- Julian OC, Lopez-Belio M, Dye WS, et al. The median sternal incision in intracardiac surgery with extracorporeal circulation; a general evaluation of its use in heart surgery. Surgery 1957;42:753-61. [PubMed]
- Dalton ML, Connally SR, Sealy WC. Julian's reintroduction of Milton's operation. Ann Thorac Surg 1992;53:532-3. [Crossref] [PubMed]
- Brown ML, McKellar SH, Sundt TM, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 2009;137:670-9.e5. [Crossref] [PubMed]
- Johnston DR, Atik FA, Rajeswaran J, et al. Outcomes of less invasive J-incision approach to aortic valve surgery. J Thorac Cardiovasc Surg 2012;144:852-8.e3. [Crossref] [PubMed]
- Urschel HC Jr, Razzuk MA. Median sternotomy as a standard approach for pulmonary resection. Ann Thorac Surg 1986;41:130-4. [Crossref] [PubMed]
- Choi JB, Yang HW. Manubrium–Sparing Median Sternotomy as a Uniform Approach for Cardiac Operations. Tex Heart Inst J 2000;27:32-6. [PubMed]
- Parker R, Adams JL, Ogola G, et al. Current activity guidelines for CABG patients are too restrictive: comparison of the forces exerted on the median sternotomy during a cough vs. lifting activities combined with valsalva maneuver. Thorac Cardiovasc Surg 2008;56:190-4. [Crossref] [PubMed]
- Grossi EA, Culliford AT, Krieger KH, et al. A survey of 77 major infectious complications of median sternotomy: a review of 7,949 consecutive operative procedures. Ann Thorac Surg 1985;40:214-23. [Crossref] [PubMed]
- McGregor WE, Trumble DR, Magovern JA. Mechanical analysis of midline sternotomy wound closure. J Thorac Cardiovasc Surg 1999;117:1144-50. [Crossref] [PubMed]
- Mangram AJ, Horan TC, Pearson ML, et al. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 1999;27:97-132. [Crossref] [PubMed]
- Patel AN, Selzman CH, Kumpati GS, et al. Evaluation of autologous platelet rich plasma for cardiac surgery: outcome analysis of 2000 patients. J Cardiothorac Surg 2016;11:62. [Crossref] [PubMed]
- Schimmer C, Ozkur M, Sinha B, et al. Gentamicin-collagen sponge reduces sternal wound complications after heart surgery: a controlled, prospectively randomized, double-blind study. J Thorac Cardiovasc Surg 2012;143:194-200. [Crossref] [PubMed]
- Hunter JE, Teot L, Horch R, et al. Evidence-based medicine: vacuum-assisted closure in wound care management. Int Wound J 2007;4:256-69. [Crossref] [PubMed]
- Kowalewski M, Pawliszak W, Zaborowska K, et al. Gentamicin-collagen sponge reduces the risk of sternal wound infections after heart surgery: Meta-analysis. J Thorac Cardiovasc Surg 2015;149:1631-40.e1-6.
- Kowalewski M, Raffa GM, Szwed KA, et al. Meta-analysis to assess the effectiveness of topically used vancomycin in reducing sternal wound infections after cardiac surgery. J Thorac Cardiovasc Surg 2017;154:1320-3.e3. [Crossref] [PubMed]
- Atkins BZ, Wooten MK, Kistler J, et al. Does negative pressure wound therapy have a role in preventing poststernotomy wound complications? Surg Innov 2009;16:140-6. [Crossref] [PubMed]
- Colli A, Camara ML. First experience with a new negative pressure incision management system on surgical incisions after cardiac surgery in high risk patients. J Cardiothorac Surg 2011;6:160. [Crossref] [PubMed]
- Lazar HL, Salm TV, Engelman R, et al. Prevention and management of sternal wound infections. J Thorac Cardiovasc Surg 2016;152:962-72. [Crossref] [PubMed]
- Schimmer C, Sommer SP, Bensch M, et al. Sternal closure techniques and postoperative sternal wound complications in elderly patients. Eur J Cardiothorac Surg 2008;34:132-8. [Crossref] [PubMed]
- Goodman G, Palatianos GM, Bolooki H. Technique of closure of median sternotomy with trans-sternal figure-of-eight wires. J Cardiovasc Surg (Torino) 1986;27:512-3. [PubMed]
- Song DH, Lohman RF, Renucci JD, et al. Primary sternal plating in high-risk patients prevents mediastinitis. Eur J Cardiothorac Surg 2004;26:367-72. [Crossref] [PubMed]
- Santhosh KN, Bravian D, More AB. Xiphoid Foramen and Its Clinical Implication. Int J Anat Res 2014;2:340-43.
- Akin K, Kosehan D, Topçu A, et al. Anatomic evaluation of the xiphoid process with 64-row multidetector computed tomography. Skeletal Radiol 2011;40:447-52. [Crossref] [PubMed]
- Kurz B, Lemke AK, Fay J, et al. Pathomechanisms of cartilage destruction by mechanical injury. Ann Anat 2005;187:473-85. [Crossref] [PubMed]
- Lachman N, Satyapal KS. Origin and incidence of xiphoid branch of the internal thoracic artery. Surg Radiol Anat 1999;21:351-4. [Crossref] [PubMed]
- Toumpoulis IK, Anagnostopoulos CE, Derose JJ Jr, et al. The impact of deep sternal wound infection on long-term survival after coronary artery bypass grafting. Chest 2005;127:464-71. [Crossref] [PubMed]
- Yi G, Shine B, Rehman SM, et al. Effect of bilateral internal mammary artery grafts on long-term survival: a meta-analysis approach. Circulation 2014;130:539-45. [Crossref] [PubMed]
- Davierwala PM, Mohr FW. Bilateral internal mammary artery grafting: rationale and evidence. Int J Surg 2015;16:133-9. [Crossref] [PubMed]
- Pinto A, Faiz O, Davis R, et al. Surgical complications and their impact on patients’ psychosocial well-being: a systematic review and meta-analysis. BMJ Open. 2016;6. [Crossref] [PubMed]