Comparison of clinical characteristics and management of asthma by types of health care in South Korea
Introduction
Asthma is a major health burden worldwide; its prevalence has increased continuously over the past decades and now affects over 10% of the global population (1-5). The economic and personal health burdens imposed by asthma are substantial in children and adolescents, particularly those in whom asthma is suboptimally controlled (6,7). The increasing prevalence of the disease and the associated socioeconomic burdens have drawn more attention to asthma control allowing patients to participate in regular activities without any restrictions (8-10). Although most patients can achieve and maintain control of the disease with appropriate treatment and upward titration of medication, significant numbers of patients have poorly controlled asthma (11-13).
Primary care is the key in the management of many chronic diseases (14). However, depending on health condition of patients, primary care patients may require referral to secondary or tertiary care (14,15). In terms of asthma, the guidelines recommend referral of patients with severe or poorly controlled asthma to specialists (1,16). However, the 2014 Royal College of Physicians’ National Review of Asthma Deaths showed that more than half of all asthma patients who died were not under specialist care during the preceding 12 months (17). Consequently, the characteristics of asthma patients by types of health care warrant investigation; currently, such information is lacking.
In the present study, we investigated clinical characteristics, management and medical cost of asthma patients in primary, secondary and tertiary medical institutions using data from the Health Insurance Review and Assessment Service (HIRA) in Korea (18).
Methods
Data sources
Korea has a single, mandatory, government-established health insurance system, and HIRA is the agency responsible for evaluating all medical claim data. HIRA collects all medical records; almost all Korean citizens are supposedly covered by the system (18-21). We retrospectively reviewed and analyzed the data from the HIRA database between July 2013 and June 2014.
Study population
We included all patients ≥15 years of age with asthma (codes J45.x-J46.x of the International Classification of Diseases 10th revision) as the principal or secondary (within the fifth position) diagnosis, and who were prescribed asthma-related medication (inhaled, oral, or injected) on at least two outpatient visits, or on at least one outpatient visit along with systemic corticosteroids prescribed on admission (20). Asthma-related medications included inhaled corticosteroids (ICSs), leukotriene receptor antagonists (LTRAs), ICSs plus long-acting β2-agonists (LABAs), short-acting β2-agonists (SABAs), short-acting muscarinic antagonists (SAMAs), SABAs plus SAMAs, long-acting muscarinic antagonists (LAMAs), systemic bronchodilators, and xanthine derivatives (21). The study was approved by the Institutional Review Board of the Catholic University of Korea, Seoul St. Mary’s Hospital (approval no. KC16RESI0560).
Definition of types of health care
Primary care (n=14,745) principally provides outpatient clinics. Secondary care (n=910) delivers to both outpatients and inpatients in hospitals with ≥30 but <100 beds. Tertiary care (n=323) delivers in general hospitals with ≥100 beds and at least three specialists among the four medical fields of internal medicine, general surgery, pediatrics, or obstetrics, together with specialists in laboratory medicine (or pathology), anesthesia, and radiology. General hospitals with ≥300 beds also have specialists in psychology and dentistry (22). Of the tertiary hospitals evaluated (n=323), 43 were comprehensive general hospitals and 280 were general hospitals.
We did not evaluate other nursing hospitals or public healthcare centers, because only small numbers of asthma patients visited such centers (0.35% for nursing hospitals and 0.40% for public healthcare centers). It is relatively easy for patients to access secondary care and tertiary care in Korea. Asthma patients who usually received primary care and were visiting secondary or tertiary care centers twice or less during the study period, were defined as being treated via primary care. When patients visited secondary or tertiary care centers at least three times, they were defined as patients treated by secondary or tertiary care. In particular, those who visited tertiary care centers at least three times were considered to be receiving tertiary care. Severe asthma exacerbation requiring hospital admission was defined as an admission to a general ward (GW), an emergency room (ER), or an intensive care unit (ICU), with a diagnosis of asthma as the principal or first additional diagnosis. Medical costs included those associated with blood tests, imaging studies, pulmonary function testing (PFT), consultations, and treatments. All costs are presented in US dollars; 1 dollar was equivalent to 1,070.80 Korean won on March 28 2018.
Statistical analyses
Data are presented as means and standard deviations for continuous variables and as numbers (with percentages) for categorical variables. Continuous variables were analyzed using one-way analysis of variance (ANOVA) and categorical data were compared using Pearson’s χ2 test or Fisher’s exact test. If variables exhibited significant differences on one-way ANOVA, we performed further bivariate comparisons between pairs of groups using the Tukey test. All tests were two-sided and a P value <0.05 was considered to indicate statistical significance. All statistical analyses were performed using SAS software (ver. 9.4; SAS Institute, Cary, NC, USA).
Results
Patients
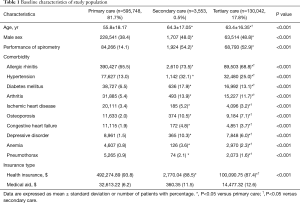
The baseline characteristics of 729,343 asthma patients are summarized in Table 1. Most (n=595,748, 81.7%) were treated via primary care, while 3,553 (0.5%) and 130,042 (17.8%) received secondary and tertiary care, respectively. The latter patients were more likely to be older and male compared with those receiving primary care (P<0.001 for age and P<0.001 for sex). In terms of spirometry, patients receiving primary care were significantly less likely to undergo PFT than patients receiving secondary or tertiary care (14.1% of primary vs. 54.2% of secondary vs. 52.9% of tertiary care patients, P<0.001). The prevalence rates of comorbidities such as allergic rhinitis, hypertension, diabetes mellitus, arthritis, ischemic heart disease, osteoporosis, congestive heart failure, depressive disorders, anemia, and pneumothorax were significantly higher in patients receiving secondary or tertiary care than primary care (P<0.001 for all comorbidities). Secondary and tertiary care patients were more likely to receive (financial) medical aid than did primary care patients (11.5% secondary vs. 12.6% tertiary vs. 6.2% primary care patients, P<0.001).
Full table
Comparison of asthma medications used in primary, secondary and tertiary care
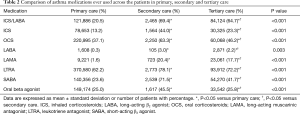
ICSs, alone and combined with LABAs, oral corticosteroids, LAMAs, LTRAs, SABAs, and oral β-agonists were used significantly more often by those in secondary and tertiary than primary care. Of patients treated via primary care, LTRAs were used by 62.2% and ICSs/LABAs, ICSs, and oral corticosteroids by 20.5, 13.2, and 37.1%, respectively. Of secondary and tertiary care patients, LTRAs were given to 78.1% and 72.2%, respectively (Table 2).
Full table
Comparison of outpatient visit, ER visit, and hospitalization among patients treated in primary, secondary and tertiary care
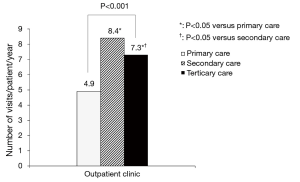
The mean number of annual outpatient visits was highest among patients receiving secondary care, followed by those receiving tertiary care and primary care (number of outpatient visits/patient/year, 8.4±9.5 vs. 7.3±6.9 vs. 4.9±5.7, respectively; P<0.001; Figure 1). Acute asthma exacerbation was most common in patients receiving secondary care (n=1,570, 44.2%), followed by those receiving tertiary (n=22,887, 17.6%) and primary care (n=11,921, 2%) during the study period (P<0.001; primary vs. secondary vs. tertiary care).
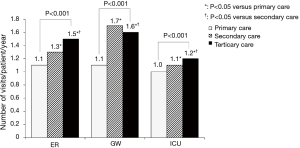
Of patients who ever visited an ER or were admitted to a GW or an ICU, the mean numbers of annual visits per patient to the ER and the mean annual admission rates per patient to GWs or ICUs differed among patients receiving primary, secondary, and tertiary care (P<0.001 for ER visits, P<0.001 for admissions to GWs, and P<0.001 for admissions to ICUs; Figure 2).
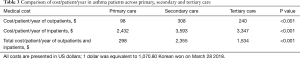
Outpatient and inpatient medical expenses
As shown in Table 3, the total medical costs/patient/year of outpatients and inpatients were highest for those receiving secondary care, followed by those receiving tertiary and primary care (P<0.001 for outpatients and P<0.001 for inpatients). The total medical (outpatient and inpatient) costs/patient/year were the highest for patients receiving secondary care, followed by those receiving tertiary and primary care (mean $2,355 vs. $1,534 vs. $298; P<0.001).
Full table
Discussion
We used HIRA data on almost all Koreans to study the clinical characteristics, the medications, utilization of medical facilities, and medical costs of asthma patients receiving primary, secondary and tertiary care. Of 729,343 patients who required treatment for asthma, most (81.7%) received primary care, while 17.8% received tertiary care and 0.5% secondary care. Asthma patients treated in secondary or tertiary care centers were older and had higher rates of comorbid diseases than did those receiving primary care. LTRAs were commonly prescribed to all patients, but the prescription rate of ICS-containing inhalers was low in primary care. The patients treated in secondary or tertiary care used more medical facilities with frequent outpatient visits, ER visits and hospital admissions than those receiving primary care. The total medical costs were over 8-fold higher for patients treated via secondary than primary care.
Although most asthma patients are managed via primary care, some with severe asthma and those who experience frequent acute exacerbations despite optimized medical therapy, should be considered for transfer to the specialists for evaluation of correctable risk factors (1,16). Accordingly, in the present study, patients receiving secondary or tertiary care utilized more medical facilities than those receiving primary care. Asthma patients treated in secondary or tertiary care centers exhibited more outpatient visits, and ER and hospital admissions (including ICU admissions) than those treated via primary care. Accordingly, the annual per-patient medical costs of secondary and tertiary care were significantly higher than those of primary care. Older age and a higher prevalence of comorbid diseases in asthma patients receiving secondary or tertiary care might have contributed to the increased medical costs.
The quality of asthma management in secondary care centers, estimated according to the use of ICS-containing inhalers and PFT performance, was similar to that of tertiary care. In addition, outpatient clinic visits and GW admissions were more common in patients receiving secondary than tertiary care. However, the proportion of patients persistently receiving secondary care was only 0.5%, much smaller than the proportion receiving tertiary care. Perhaps, this phenomenon is explained by the relatively easy access to tertiary care in Korea. Patients can directly visit tertiary care centers with only a referral note from the primary care physician. As secondary care is geographically more accessible than tertiary care, asthma patients with comorbid conditions may prefer to visit local secondary care centers. The tertiary hospitals of Korea include 43 comprehensive general hospitals with respiratory specialists and 280 general hospitals with or without such specialists. Thus, the clinical severity of asthma in tertiary hospitals with respiratory specialists might be diluted by less severe asthma patients treated in tertiary hospitals without respiratory specialists.
ICS-containing inhalers are the first-line therapy for long-term control of asthma (1). In the USA, the prescription rate of ICSs to asthma patients is 72.5% (23) and it is 43% in Europe (2). In the present study, the overall prescription rates of ICSs/LABAs and ICSs were 28.6% and 15.2%, respectively, reflecting low usage of ICS-containing inhalers by those in primary care (21% ICSs/LABAs and 13% ICSs). Given that LTRA is the most common medication prescribed to primary care patients (62.2%), primary physicians may find it difficult to explain inhaler techniques. Also, because relatively higher proportions of patients with stable or asymptomatic asthma receive primary care, patient adherence to inhalers may be poor in the real world (24,25). However, a low ICS prescription rate can trigger poor asthma control (26). Continuous education emphasizing the useful role of ICS-containing inhalers in terms of asthma control is urgently needed by physicians and primary care patients.
The GINA guidelines (1) indicate that once asthma has been diagnosed, PFT should generally be recommended both at that time and 3–6 months after treatment initiation, as lung function is a useful indicator of disease severity and a predictor of the risk of acute exacerbation (27-30). However, PFT was performed on only 14% of primary care patients, which was lower than in Canada (23%) (31). PFT was performed on approximately 55% of secondary and tertiary care patients, similar to the rate associated with specialist care in Canada (55%) (31). This may be because PFT is not easily available in primary clinic compared to secondary or tertiary care. Also, approximately half of all patients did not undergo PFT when treated in secondary or tertiary care centers. Thus, lack of knowledge of physicians regarding the importance of PFT could be possible reason for the low PFT rate. Further studies are needed to investigate the poor adherence to guidelines regarding PFT.
The medical costs associated with asthma vary widely worldwide; the mean annual per-patient cost is $1,900 in Europe and $3,100 in the USA (32). In the Asia-Pacific region, the annual per-patient direct cost ranged from $108 to $1,010, being $268 in Korea, thus similar to that of most other countries of the Asia-Pacific region (33). In our study using HIRA data, the total direct medical cost for patients in primary care was $298/patient/year, and averaged $528/patient/year for all patients (in primary, secondary, or tertiary care). The total medical costs differed by the nature of the care delivered, with a substantial economic burden being imposed by patients receiving secondary and tertiary care.
Our study had certain limitations. First, the patient adherence to inhalers could not be assessed because the HIRA database does not record such information. Second, the definition of patients belonged to each health care was arbitrarily based on the number of visits to clinics due to mixed visits among primary, secondary or tertiary care. This is explained by a unique feature of the Korean healthcare system, which allows patients to freely visit any specialist once the primary care physician writes a referral note. Finally, the reasons for the low-level prescription of ICSs and performance of PFT by primary clinics remain unclear. Further studies are necessary to investigate obstacles to appropriate management. Despite these limitations, the large amount of nationwide data evaluated in the present study provided useful information on asthma management in daily practice in Korea and can aid in the development of improved asthma management.
Conclusions
Most patients with asthma were managed in primary care, but those receiving secondary or tertiary care utilized more medical facilities with higher medical costs. Given the low use of diagnostic measures and the low rate of prescription of inhalants containing corticosteroids to patients in primary care, we suggest that continuous education of both patients and physicians is required to improve the quality of asthma management.
Acknowledgments
This study was supported by HIRA (the Joint Project on Quality Assessment Research).
Funding: Republic of Korea and Samsung Medical Center Foundation for Medical Research (grant No. SMX1151371).
Footnote
Conflicts of Interest: Chin Kook Rhee has received consulting/lecture fees from MSD, AstraZeneca, Novartis, GSK, Takeda, Mundipharma, Sandoz, Boehringer-Ingelheim, and Teva-Handok. Hye Yun Park has received lecture fees from AstraZeneca, Novartis, and Boehringer-Ingelheim. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of the Catholic University of Korea, Seoul St. Mary’s Hospital (approval no. KC16RESI0560).
References
- GINA. Global Strategy for Asthma Management and Prevention (2017 update). Available online: http://wwwginasthmaorg/. Assessed September 1, 2017.
- Cazzoletti L, Marcon A, Janson C, et al. Asthma control in Europe: a real-world evaluation based on an international population-based study. J Allergy Clin Immunol 2007;120:1360-7. [Crossref] [PubMed]
- To T, Stanojevic S, Moores G, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health 2012;12:204. [Crossref] [PubMed]
- Chu LM, Pahwa P. Prevalence and associated factors for self-reported asthma in a Canadian population: The Canadian Community Health Survey, 2014. J Asthma 2018;55:26-34. [Crossref] [PubMed]
- de Marco R, Cappa V, Accordini S, et al. Trends in the prevalence of asthma and allergic rhinitis in Italy between 1991 and 2010. Eur Respir J 2012;39:883-92. [Crossref] [PubMed]
- Anis AH, Lynd LD, Wang XH, et al. Double trouble: impact of inappropriate use of asthma medication on the use of health care resources. CMAJ 2001;164:625-31. [PubMed]
- Sadatsafavi M, Lynd L, Marra C, et al. Direct health care costs associated with asthma in British Columbia. Can Respir J 2010;17:74-80. [Crossref] [PubMed]
- Bahadori K, Doyle-Waters MM, Marra C, et al. Economic burden of asthma: a systematic review. BMC Pulm Med 2009;9:24. [Crossref] [PubMed]
- Bateman E, Bousquet J, Keech M, et al. The correlation between asthma control and health status: the GOAL study. Eur Respir J 2007;29:56-62. [Crossref] [PubMed]
- Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004;59:469-78. [Crossref] [PubMed]
- Nathan RA, Thompson PJ, Price D, et al. Taking Aim at Asthma Around the World: Global Results of the Asthma Insight and Management Survey in the Asia-Pacific Region, Latin America, Europe, Canada, and the United States. J Allergy Clin Immunol Pract 2015;3:734-42.e5. [Crossref] [PubMed]
- Price D, Fletcher M, van der Molen T. Asthma control and management in 8,000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med 2014;24:14009. [Crossref] [PubMed]
- Demoly P, Annunziata K, Gubba E, et al. Repeated cross-sectional survey of patient-reported asthma control in Europe in the past 5 years. Eur Respir Rev 2012;21:66-74. [Crossref] [PubMed]
- Jose BP, Camargos PA, Cruz Filho AA, et al. Diagnostic accuracy of respiratory diseases in primary health units. Rev Assoc Med Bras (1992) 2014;60:599-612. [Crossref] [PubMed]
- Lenney W, Clayton S, Gilchrist FJ, et al. Lessons learnt from a primary care asthma improvement project. NPJ Prim Care Respir Med 2016;26:15075. [Crossref] [PubMed]
- Chang YS. Practical Guideline of Asthma Management-Korean Guideline for Asthma 2015. Korean J Med 2016;90:298-306. [Crossref]
- Levy ML. The national review of asthma deaths: what did we learn and what needs to change? Breathe (Sheff) 2015;11:14-24. [Crossref] [PubMed]
- Kim L, Kim J-A, Kim S. A guide for the utilization of health insurance review and assessment service national patient samples. Epidemiol Health 2014;36. [Crossref] [PubMed]
- Lee H, Rhee CK, Lee BJ, et al. Impacts of coexisting bronchial asthma on severe exacerbations in mild-to-moderate COPD: results from a national database. Int J Chron Obstruct Pulmon Dis 2016;11:775-83. [PubMed]
- Choi JY, Yoon HK, Lee JH, et al. Current status of asthma care in South Korea: nationwide the Health Insurance Review and Assessment Service database. J Thorac Dis 2017;9:3208-14. [Crossref] [PubMed]
- Rhee CK, Yoon HK, Yoo KH, et al. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. COPD 2014;11:163-70. [Crossref] [PubMed]
- National Law information center. Available online: http://www.lawkorea.com/client/asp/lawinfo/law/lawview.asp?type=l&lawcode=d636349. Assessed on Oct. 14. 2017.
- Adams RJ, Fuhlbrigge A, Guilbert T, et al. Inadequate use of asthma medication in the United States: results of the asthma in America national population survey. J Allergy Clin Immunol 2002;110:58-64. [Crossref] [PubMed]
- Thomas M, Murray-Thomas T, Fan T, et al. Prescribing patterns of asthma controller therapy for children in UK primary care: a cross-sectional observational study. BMC Pulm Med 2010;10:29. [Crossref] [PubMed]
- Wisnivesky JP, Lorenzo J, Lyn-Cook R, et al. Barriers to adherence to asthma management guidelines among inner-city primary care providers. Ann Allergy Asthma Immunol 2008;101:264-70. [Crossref] [PubMed]
- Laforest L, Licaj I, Devouassoux G, et al. Prescribed therapy for asthma: therapeutic ratios and outcomes. BMC Fam Pract 2015;16:49. [Crossref] [PubMed]
- Ulrik CS. Outcome of asthma: longitudinal changes in lung function. Eur Respir J 1999;13:904-18. [Crossref] [PubMed]
- Fuhlbrigge AL, Kitch BT, Paltiel AD, et al. FEV(1) is associated with risk of asthma attacks in a pediatric population. J Allergy Clin Immunol 2001;107:61-7. [Crossref] [PubMed]
- Kitch BT, Paltiel AD, Kuntz KM, et al. A single measure of FEV1 is associated with risk of asthma attacks in long-term follow-up. Chest 2004;126:1875-82. [Crossref] [PubMed]
- Munoz-Cano R, Torrego A, Bartra J, et al. Follow-up of patients with uncontrolled asthma: clinical features of asthma patients according to the level of control achieved (the COAS study). Eur Respir J 2017.49. [PubMed]
- Gershon AS, Victor JC, Guan J, et al. Pulmonary function testing in the diagnosis of asthma: a population study. Chest 2012;141:1190-6. [Crossref] [PubMed]
- Nunes C, Pereira AM, Morais-Almeida M. Asthma costs and social impact. Asthma Res Pract 2017;3:1. [Crossref] [PubMed]
- Lai CKW, Kim YY, Kuo SH, et al. Cost of asthma in the Asia-Pacific region. Eur Respir Rev 2006;15:10-6. [Crossref]