Effect of different thoracic anesthesia on postoperative cough
Introduction
Sore throat and cough are common complications of tracheal intubation. It is reported that the incidence of postoperative sore throat is 14.4% to 50% and cough is 50% to 94.7% (1). Postoperative cough is a great challenge for patients owing to its delaying rehabilitation after thoracic surgery. Chronic and intractable coughs seriously affect postoperative rehabilitation and lower the quality of patients’ life. It has been reported that cough after pulmonary resection (CAP) is a common complication. The occurrence probability of CAP is as high as 25% to 50%. The occurrence probability of CAP will be more than 50% within 1 year after operation, and will be 18% within 5 years. At the same time, the researchers found that there was 25% probability of CAP in patients who are long-term survival after lung cancer (2-4). According to Brouillette, the probability of cough after tracheal intubation was 94.87%, compared with 17.94% in the LMA group (5). The Ramanathan team’s findings were consistent with Brouillette. They divided 60 patients randomly into tracheal intubation group and laryngeal mask group. The results showed that the postoperative cough rate was 83.3% in the tracheal intubation group and 20% in the laryngeal mask group. Based on 76 cases of total thyroidectomy, such as Jung-Hee Ryu, also found that cough in the tracheal intubation group was more likely to happen than in the laryngeal mask group (6). Therefore, many scholars tried to reduce the complications of sore throat and cough after intubation by using prophylactic topical drugs such as beclomethasone and lidocaine spray in tracheal catheter, or by intravenously injecting dexamethasone and other systemic drugs, but all these failed to avoid intubation injury. Double lumen tube (DLT) is a traditional thoracic anesthesia. DLT has a large diameter, a large cuff, and requires a rotation angle to reach the target bronchus through the glottis, which makes it easier to cause complications, such as postoperative cough, sore throat, than a single-lumen catheter. Previous studies found that the operations of thoracic surgery, such as tracheal stump exposure, lymph node dissection, bronchial deformation, diaphragmatic displacement, loss of lung capacity, residual lung deformation and lung distention traction are the important causes of postoperative cough.
In non-intubated thoracic surgery, spontaneous breathing anesthesia is performed under moderate sedation and analgesia (or composite regional nerve block) without endotracheal intubation or just with supraglottic artificial airway (such as laryngeal mask). These factors enable patients to avoid pressure or volume damage that may exist during unilateral pulmonary mechanical ventilation, improve pulmonary shunt, and avoid the adverse effects caused by residual muscle relaxation. A series of recent studies show that non-tracheal intubation and anesthesia with spontaneous breathing can be safely applied to video-assisted thoracic surgery, thymus, and other operations (7).
Will spontaneous respiration anesthesia be effective to reduce thoracic postoperative cough problems when performing thoracic surgery without an endotracheal tube? Previous studies have failed to distinguish the effects of surgery (such as lung tissue trauma) and anesthetic factors (such as tracheal intubation) on cough. In this retrospective analysis, we analyze the postoperative cough status of these two anesthesia methods, compare the degree of influence of anesthesia and surgical factors, and find out whether spontaneous respiration anesthesia could reduce the probability of cough.
Methods
General information
Case admission requirement:
- Age 18–65 years old, ASA I–II grade;
- Mallampati airway grading: Grades I–II;
- Lung function tests pass, without asthma, serious cardiovascular disease, COPD, blood system diseases, or mental illness history;
- Body mass index (BMI) <25 kg/m2;
- Without preoperative respiratory infection, chronic cough, history of cough, history of acid reflux, or postnasal drip syndrome;
- Surgery is limited to VAST bullectomy, wedge resection, segmentectomy and lobectomy.
Excluding cases include:
- Refusal to postoperative follow-up (the patient or family member is reluctant to accept the postoperative follow-up);
- Loss of contact: cases of death or loss of contact.
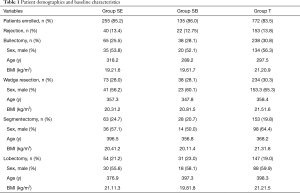
The anesthesia protocol was reviewed and approved by the Institutional Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University. From July 2011 to December 2015, a total of 1,162 cases of the Center met the above conditions and were able to complete postoperative follow-ups. All cases were divided into DLT intubation anesthesia group (group T, n=925 cases) and spontaneous respiratory anesthesia group (group S, n=456 cases), and group S was further divided into intravenous composite intercostal nerve block anesthesia group (group SB, n=157 cases) and intravenous compound epidural anesthesia group (group SE, n=299 cases).
Anesthesia method
All patients received intramuscular midazolam (0.04–0.06 mg/kg) and atropine (0.01 mg/kg) 30 mins before anesthesia, and the upper extremity venous access opens after admission. Noninvasive arterial blood pressure (NBP), II lead electrocardiogram (ECG), heart rate (HR), pulse oxygen saturation (SpO2), respiratory frequency (RR) and bispectral index (BIS) were monitored with a Philips InteliVue MP40 monitor. After induction of anesthesia with placing the central venous catheter, the radial artery pressure (IBP) was recorded and blood gas analysis was performed when necessary. Patients in group T were monitored continuously for exhaled carbon dioxide pressure (PetCO2).
Group T: the endotracheal diameter values were measured according to the preoperative chest image and the corresponding model of DLT was selected. After the mask was deoxygenated for 3 minutes, plasma target-controlled infusion (TCI) propofol 2–3 µg/mL, sufentanil 0.3–0.5 µg/kg, and cisatracurium 0.2 mg/kg. After placement of DLT, the bronchoscope was placed at the end of the tube, with IPPV tidal volume (VT) 6–8 mL/kg, and frequency (RR) 10–15 beats/min. Anesthesia was maintained with inhale of sevoflurane (1–2%), propofol (TCI, 0.5–2 µg/mL), and remifentanil (0.05~0.1 µg/kg/min) and intermittently adding cisatracurium (induced amount of 1/5–1/10) maintain muscle relaxation. At the end of the operation, a chest drainage tube was left inside.
Group SB: intravenous anesthesia was performed with propofol (TCI, 1.5–3.5 µg/mL) and remifentanil (0.03–0.05 µg/kg/min), and a single dose of sufentanil was administered according to the course of the surgery as necessary (2–5 µg). Local anesthesia (1% lidocaine 2–5 mL) was performed on the surgical incision. After thoracotomy, 2% lidocaine 5 mL was sprayed on the visceral pleura, and T2–T8 intercostal nerve block was performed under direct intrathoracic view (0.75% ropivacaine and 2% lidocaine in a 1:1 mixture, approximately 0.5 mL per intercostal space), and intraoperative thoracic vagal nerve block stagnation (about 3 mL of 1:1 mixture of 0.75% ropivacaine and 2% lidocaine). During the surgery, spontaneous breathing was maintained and nasal oxygen was used (3–5 L/min) without any artificial airway. At the end of the operation, a chest drainage tube was left inside.
Group SE: after T7–8 or T8–9 line epidural puncture, the catheter was placed into the epidural space 3 cm into the head, the test volume was 2 mL of 2% lidocaine, and 0.5% ropivacaine 4 to 5 mL (total 8–10 mL) was given in 5 min intervals, adding 3 to 5 mL every 45 minutes. After intravenous anesthesia with propofol (TCI, 1.5–3.5 µg/mL) and remifentanil (0.03–0.05 µg/kg/min), a single dose of sufentanil (2–5 µg) was given if necessarily depending on the course of the surgery. Visceral pleura, vagal nerve block, intraoperative breathing, airway management, and end of surgery were the same as group SB.
Observation indicators
- Record the number of rejects;
- Record the gender, age and BMI of each case;
- Record the postoperative antibiotic application time (days), chest drainage tube indwelling time (days) and hospital stay (days);
- Record the cough status of each case on the first day (T1), the second day (T2), the third day (T3), and the first month (T4), and the third month (T5), the six month (T6), and the twelve months (T7) after thoracoscopic surgery. Chronic cough refers to a status mainly with cough as the only symptom or main symptoms lasting more than 8 weeks, without any other cause related to the surgery, and without any other lesions in X-ray.
For the T6 chronic cough, the cough symptom score survey, the Leicester cough questionnaire (LCQ) and the visual analogue scale (VAS) test were conducted and the results was recorded. The cough symptom score table reflects the cough frequency, intensity, and conditions affecting the quality of life. The higher the score, the more serious it reflects frequency, intensity, and effects. LCQ evaluates the impact of cough on quality of life from three parts: physiological, psychological, and social. The higher the score is, the lower the influence is, and the greater the effect is (8). VAS uses a linear scoring method (0–10 points). The larger the value, the heavier the cough is.
Statistical methods
All data are analyzed using statistical software SPSS 19.0. The statistics of measurement data are expressed x ± s. Count data are expressed as a percentage, using χ2 and groups comparison and Fisher’s exact test. P<0.05 is considered statistically significant.
Results
- There is no statistically significant difference in the rejection rate among the groups (P>0.05) (shown in Table 1);
- There is no significant difference in the number of different anesthetic methods in various surgical procedures (P>0.05) (shown in Table 1);
- There is no significant difference in age and BMI between groups (P>0.05). There was no statistically significant difference in age and BMI within each group (P>0.05) (shown in Table 1);
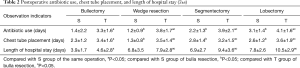
- In all types of surgical procedures, the number of postoperative days of antibiotic use, number of days of chest drains, and days of hospital stay in group S were all less than in group T. Thus there is a statistically significant difference between groups (P<0.05) (shown in Table 2).
Full table
Full table
Postoperative cough
The incidence of cough in each group (shown in Table 3)

Full table
The incidence of cough at each time point in each group shows a decreasing trend with the increase of the postoperative time, and there is a statistically significant difference between groups (P<0.05).
There is no significant difference in the incidence of cough between group SE and group SB at each time point (P>0.05). The incidence of cough at each time point in group T is significantly higher than that in other groups. There is a statistically significant difference between groups (P<0.05).
Probability of chronic cough in different types of surgery of the middle and long term (T5, T6 and T7) (shown in Table 4)
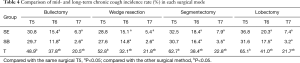
Full table
In all surgical procedures the incidence of chronic cough in all groups shows a decreasing trend with the increase of postoperative time. There is a statistically significant difference among the groups (P<0.05). The incidence of chronic cough in each time point of group T is greater than that of other groups. There is statistical difference between groups (P<0.05).
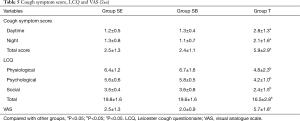
Cough symptom score, LCQ and VAS
- The scores of cough symptoms in group T are higher than those in other groups. There is a statistically significant difference between groups (P<0.05), while there is no statistical difference between group SE and group SB (P>0.05) (shown in Table 5);
- The scores and total scores of the physiological, psychological, and social components of the LCQ in group T are lower than those in the other groups. There is a statistically significant difference between the groups (P<0.05), while the VAS scores are higher than those in the other groups. There is a statistically significant difference between the groups (P<0.05) (shown in Table 5).
Discussion
Postoperative cough is a common complication after thoracic surgery. Chronic, intractable coughs seriously affect postoperative rehabilitation and the quality of life. Some studies have reported that about 50% of patients with lung cancer undergo lobectomy, there is cough happening within 1 year, and 25% of patients suffer from it more than 5 years after surgery (1). The two main factors affecting postoperative cough are anesthesia and the surgery process. Anesthesia is mainly endotracheal intubation, and surgical trauma includes bronchial stump exposure, lung lymph node dissection, bronchial deformity, diaphragmatic displacement, loss of lung capacity, residual lung deformation and lung bulging, and preoperative cough and gastroesophageal acid reflux aggravate, etc. (9). However, due to the necessity of endotracheal intubation in past thoracic anesthesia, the relevant cough studies failed to distinguish between anesthetic and surgical factors, thus they can’t be independently analyzed and compared.
In this study, the incidence of cough gradually decreases with the increase of postoperative time. With spontaneous respiratory anesthesia, the incidence of cough is lower in all stages within 1 year after surgery under the same surgical approach. The incidence of cough is about 27% to 36% at 3 months after different surgical, and about 2.6% to 7.9% in 1 year. While in DLT anesthesia it is about 48.9% to 65.1% at 3 months after different surgical and approximately 20.5% to 22.8% in 1 year. Studies have shown that DLT is easier to cause postoperative cough than single lumen catheters. The main reason is that the DLT is thicker and harder, difficulty tracheal intubation, the rotation angle of the catheter when passing through the glottis is not appropriate (10), size cuff local compression, fiberoptic bronchoscope positioning and repeated suction secretions, the extubation and sucking on the trachea, bronchus, vocal cords, and throat mucosa damage (11). There is elevation of interleukin-6 (IL-6) in the early stage of inflammation following endotracheal intubation in the porcine model (12). Fleischer and Hess found that when catheter balloon pressure exceeds mucosal capillary pressure, mucosal ischemia immediately induces stress, congestion, edema, and inflammation (13). After tracheal intubation, the nasal cavity and upper respiratory tract are not wet, resulting in airway mucosal injury and accumulation of tracheal and bronchial secretions (14). Invasion of exogenous and endogenous bacteria during intubation causes infection, resulting in elevated IL-6 (15). DLT intubation with one lung ventilation and lung recruitment can cause oxidative stress and aggravate ischemia-reperfusion injury (16). Muscle remnant residual effects impair the coordination of the pharynx muscles while impairing the impairment of lung function and the protective physiologic reflex (17). The injury of throat, trachea, bronchus, bronchioles, alveoli, lung and residual muscle relaxants can easily lead to airway inflammation. Airway inflammation is an important pathological and pathological mechanism of chronic cough. The throat, trachea/bronchus, especially the carina, are sensitive cough receptors and there are a large number of cough receptors on the surface of the trachea and bronchi (18). Inflammation impairs airway epithelial cells. Cough receptors are exposed due to loss of epithelial cells and are susceptible to external stimuli and excitement. The accumulation of acidic substances and changes in airway pH during inflammation can stimulate C nerve fibers, excite the nerve center, cause airway nerve inflammation, bronchoconstriction, and aggravate postoperative cough (19).
In non-intubated thoracic surgery, spontaneous breathing anesthesia is performed under moderate sedation and analgesia (or composite regional nerve block) without endotracheal intubation or just with supraglottic artificial airway (such as laryngeal mask). These factors enable patients to avoid pressure or volume damage that may exist during unilateral pulmonary mechanical ventilation, improve pulmonary shunt, and avoid the adverse effects caused by residual muscle relaxation. In the study, the incidence of postoperative cough in the spontaneous respiratory anesthesia group is significantly lower than that in the DLT group. The main reason may be that no tracheal intubation reduces the bronchial mucosal inflammatory damage, and airway integrity is protected, and muscle relaxant residues are avoided.
The results show that in the spontaneous respiratory anesthesia group that was no endotracheal intubation, mechanical ventilation, and residual muscle relaxant drugs, the probability of coughing is approximately 27% to 36% 3 months after surgery, and approximately 2.6% to 7.9% in 1 year after surgery. While the combination of surgery and anesthesia methods increases the probability of coughing is 48.9–65.1% at 3 months after surgery, and about 20.5–22.8% in 1 year after surgery. In the lobectomy and segmentectomy with dissociating, cutting off and ligation of pulmonary artery, pulmonary artery, lymphatic vessel, and bronchus that needs with a variety of instruments, and continuously the hilar, trachea, and bronchus during the operation that damaged the lungs, trachea, and bronchus. The main receptors of the vagus nerve C-fibers are mainly distributed in the larynx, trachea, carina, and larger bronchi in the lungs, and are distributed not only in the tracheal mucosal epithelium but also in the cough effector located in the airway wall. After cough sensory stimulation, the stimulation goes along the impulse of the brain and then the vagus nerve, phrenic nerve to the ventilator, dominating respiratory muscle movement, thus producing the cough.
The results of this study shows that the rates of cough in the short and mid- to long term after operation in the two subgroups of spontaneous respiratory anesthesia are similar, indicating that the breaking capacity is basically the same between peripheral nerve block and spinal nerve block in the afferent stimulation. Epidural anesthesia can reduce the release of tumor necrosis factor (TNF-α) and IL-6 and inhibit inflammatory factors by inhibiting the neuroendocrine stress response. A series of studies have shown that thoracic epidural anesthesia can improve the postoperative pulmonary function, oxygenation, reduce postoperative traumatic stress response, reduce the release of inflammatory factors, and postoperative complications. Taiwanese scholars found in a retrospective case of 238 cases of thoracoscopic lobectomy that non-intubated thoracoscopic lobectomy using thoracic epidural (TEA) was safe and reliable (20). Intercostal nerve block can effectively block the afferent operation of noxious stimulation, reduce physiological stress and the release of inflammatory factors. In this study, thoracoscopy was used to visualize the intercostal nerve block to accurately understand the nerves and surrounding tissues. Then the puncture needle was directly and accurately placed into the target nerve, the minimum effective dose block was accurately used to reduce nerve damage and reduce the risk of local anesthetic poisoning. Scholars (21) found that the use of non-tracheal intubation with intercostal nerve block or thoracic epidural anesthesia in the safety and feasibility in the lobectomy. The results of postoperative respiratory function recovery, postoperative analgesia, and postoperative complication rate were satisfactory in the intercostal nerve block and thoracic epidural anesthesia. Intercostal nerve block can effectively reduce the release of pro-inflammatory factors, increase the release of anti-inflammatory factors, regulate cytokine balance, inhibit the body’s inflammatory response, and regulate immune function, which is conducive to postoperative rehabilitation.
The degree of trauma increases from pulmonary bullectomy, pulmonary bullectomy segmentectomy to lobectomy. Lung injury increases oxidative stress and pro-inflammatory cytokines in the lung (22). In this study, the probability of cough is approximately 50% after 3 months of bullectomy/pulmonary bullectomy in the DLT anesthesia and approximately 60% in the segmentectomy /lobectomy, indicating that larger wounds aggravate postoperative cough. After Pulmonary lobectomy, segmentectomy, wedge resection of the lungs, and bulla resection, the anatomy and physiological structure of the lungs are changed, which easily leads to a decrease in the capacity of the affected side of the lungs. The pressure in the pleural cavity is reduced and the body fills the residual cavity to restore the normal pressure of pleural cavity through compensatory mechanisms. Long-term anatomical and physiological changes lead to increased respiratory mechanics and airway sensitivity during breathing, leading to persistent cough after surgery. Intraoperative traction results in the rapid adaptation of the lungs to the receptor (RAR) and the C-fiber receptors are activated by extensive mechanical stimuli, which leads to activation of the cough receptor and leads to increasing of postoperative cough.
Under the same anesthetic method, the incidence of chronic cough after lobectomy is higher than other surgical methods, and it may be related to other factors such as lymph node clearance during surgery. In related studies, it was found that the incidence of chronic cough after radical mastectomy (especially after removal of the subcarinal or upper mediastinal lymph nodes) was high. It is considered that local cavities can be formed after the removal of lymph nodes, so that pulmonary stretch receptors of the sub-carina and the main bronchus were involved. Exposure of the sensilla to the receptors and postoperative lung respiration evoked the susceptor formed a series of conduction coughs (22). The results of this study shows that the incidence of four surgical coughs decreases to approximately 20% in 1 year after surgery, suggesting that although the degree of trauma is different, the degree of lung tissue repair at 1 year after surgery is similar.
The use of antibiotics, chest drainage tube indwelling time, and length of stay are significantly reduced in the spontaneous respiratory anesthesia group. The experimental results are consistent with Liu (23) in a randomized experiment of 354 patients undergoing video-assisted thoracoscopic lobectomy, the experimental results showed that the concentration of TNF-α levels in bronchoalveolar lavage fluid in the spontaneously breathing group was lower than of the intubation group, and antibiotic use time and fasting time are significantly shorted after surgery.
The study found that in the DLT anesthesia, day/night cough frequency and the seriousness degree of cough are heavier. VAS scores and LCQ scores are significantly higher than those in the spontaneous breathing group. This indicates that the postoperative cough in the DLT group has a great impact on the individual’s physical and mental health.
In conclusion, there is a correlation between pulmonary surgery and postoperative cough. There is higher probability of postoperative cough in patients with greater trauma, and the probability of cough is approximately 27% to 36% at 3 months after surgery and approximately 2.6% to 7.9% in 1 year after surgery. The combination of surgery and anesthesia methods increases from 48.9% to 65.1% at 3 months after surgery, and about 20.5% to 22.8% in 1 year after surgery Spontaneous respiratory anesthesia can significantly reduce the probability of cough, improve postoperative recovery and improve postoperative quality of life of patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The anesthesia protocol was reviewed and approved by the Institutional Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University. Informed consent was obtained from all enrolled patients, who signed both a “Consent to Anesthesia with spontaneous respiration” form and a “Consent to General Anesthesia with Tracheal Intubation” form.
References
- McHardy F, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia 1999;54:444-53. [Crossref] [PubMed]
- Sarna L, Evangelista L, Tashkin D, et al. Impact of respiratory symptoms and pulmonary function on quality of life of long-term survivors of non-small cell lung cancer. Chest 2004;125:439-45. [Crossref] [PubMed]
- Sawabata N, Maeda H, Takeda S, et al. Persistent Cough Following Pulmonary Resection: Observational and Empiric Study of Possible Causes. Ann Thorac Surg 2005;79:289-93. [Crossref] [PubMed]
- Long H, Lin ZC, Lin YB, et al. Quality of life after lobectomy for early stage non-small cell lung cancer--video-assisted thoracoscopic surgery versus minimal incision thoracotomy. Ai Zheng 2007;26:624-8. [PubMed]
- Brouillette G, Drolet P, Donati F. Deep extubation and insertion of laryngeal mask airway reduces coughing at emergence. Can J Anaesth 2008;55:4721391-2. [Crossref]
- Ryu JH, Yom CK, Park DJ, et al. Prospective randomized controlled trial on the use of flexible reinforced laryngeal mask airway (LMA) during total thyroidectomy: effects on postoperative laryngopharyngeal symptoms. World J Surg 2014;38:378-84. [Crossref] [PubMed]
- Dong Q, Liang L, Li Y, et al. Anesthesia with nontracheal intubation in thoracic surgery. J Thorac Dis 2012;4:126-30. [PubMed]
- Lin R, Che G. Validation of the Mandarin Chinese version of the Leicester Cough Questionnaire in non-small cell lung cancer patients after surgery. Thorac Cancer 2018;9:486-90. [Crossref] [PubMed]
- Sawabata N, Takeda S, Tokunaga T, et al. Acid regurgitation associated with persistent cough after pulmonary resection: an observational study. Cough 2006;2:9. [Crossref] [PubMed]
- Seo JH, Kwon TK, Jeon Y, et al. Comparison of techniques for double-lumen endobronchial intubation: 90° or 180° rotation during advancement through the glottis. Br J Anaesth 2013;111:812-7. [Crossref] [PubMed]
- Benjamin B. Laryngeal trauma from intubation: endoscopic evaluation and classification. Otolaryngol Head Neck Surg 1998.2013-35.
- Echternach M, Mencke T, Richter B, et al. Laryngeal alterations following endotracheal intubation and use of larynx masks. HNO 2011;59:485-98. [Crossref] [PubMed]
- Fleischer S, Hess M. Systematic investigation technique in videolaryngoscopy and stroboscopy. HNO 2003;51:160-7. [Crossref] [PubMed]
- Hanschmann H, Berger R. Quantification of videostroboscopic vocal cord findings. Laryngorhinootologie 2009;88:6. [PubMed]
- Cormack R, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984;39:1105-11. [Crossref] [PubMed]
- Misthos P, Katsaragakis S, Milingos N, et al. Postresectional pulmonary oxidative stress in lung cancer patients. The role of one-lung ventilation. Eur J Cardiothorac Surg 2005;27:379-82; discussion 82-3. [Crossref] [PubMed]
- Fuchs-Buder T, Nemes R, Schmartz D. Residual neuromuscular blockade: management and impact on postoperative pulmonary outcome. Curr Opin Anaesthesiol 2016;29:662-7. [Crossref] [PubMed]
- Widdicombe J. Airway receptors. Respir Physiol 2001;125:3-15. [Crossref] [PubMed]
- Ricciardolo FL. Mechanisms of citric acid-induced bronchoconstriction. Am J Med 2001;111:18-24. [Crossref] [PubMed]
- Hung MH, Chan KC, Liu YJ, et al. Nonintubated thoracoscopic lobectomy for lung cancer using epidural anesthesia and intercostal blockade: a retrospective cohort study of 238 cases. Medicine (Baltimore) 2015;94. [Crossref] [PubMed]
- D'Andrilli A, Ibrahim M, Ciccone AM, et al. Intrapleural intercostal nerve block associated with mini-thoracotomy improves pain control after major lung resection. Eur J Cardiothorac Surg 2006;29:790-4. [Crossref] [PubMed]
- Huang J, Luo Q, Shentu Y, et al. Prevention of refractory cough with mediastinal fat to fill the residual cavity after radical systematic mediastinal lymphadenectomy in patients with right lung cancer. Zhongguo Fei Ai Za Zhi. 2010;13:975-9. [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [Crossref] [PubMed]