Management of complications in thoracoscopic surgery
Introduction
Thoracoscopic surgery has been widely applied in many procedures in general thoracic surgery. According to the survey of Japan Society for Endoscopic Surgery, 20,357 thoracoscopic procedures were performed in 2015 while 19,125 in 2010 and 11,405 in 2005 (1). Among them, 12,610 lobectomies and 3,221 segmentectomies were performed in 2014 and 2015. Three hundred and four open conversion for bleeding were reported. This means about 2% of the major lung surgery end up with open conversion. It is important to manage complications by thoracoscopic surgery methods to avoid open conversion. This is beneficial not only for the patients but also for the surgeons.
Methods
Three port thoracoscopic surgery technique was used in all procedures in this report for the management of the complications.
Two hundred and twenty bleeding happened from pulmonary artery injury and 38 from pulmonary vein and 9 from superior vena cava which counts 88% of the bleeding from low pressure system for open conversion.
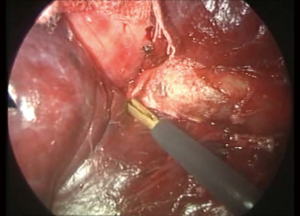
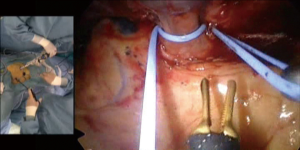
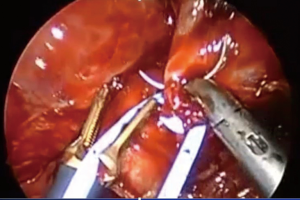
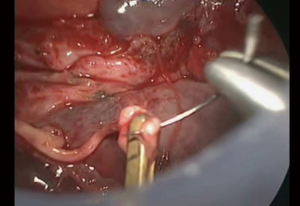
First step for control bleeding was giving compression on the bleeding point. Usually lungs nearby were used to stop bleeding then a gauze was placed into the chest cavity and took over the compression. When bleeding was not successful only by compression, fibrin sealant patch was placed (Figure 1). At least 3 minutes gentle compression with a gauze enough to stop bleeding should be maintained. Bleeding from torn small branches such as torn left A1+2c pulmonary arterial branch could be controlled with this method (Figure 2). Care must be taken when removing the gauze not to remove the fibrin sealant patch at the same time. Double loop encircling of the pulmonary artery proximal and distal part of the bleeding point with vascular slings could reduce the bleeding and that helped bleeding control (Figure 3). In one occasion, thoracoscopic pulmonary artery suture closure was done after vascular sling bleeding control (Figure 4).
Phrenic nerve could be injured incidentally or on purpose to remove malignancy. When the nerve was elongated due to the compression of the tumor, direct end-to-end anastomosis was performed. Single 6-0 absorbable monofilament suture was sufficient for anastomosis (Figure 5). When the tension free anastomosis was not possible, intercostal nerve interposition technique (Figure 6) was used (4). For the harvesting the intercostal nerve for interposition, 8th intercostal nerve was used due to our trocar placement.

Bronchus could be injured during the major lung surgery with lymph node dissection (Figure 7). Sometimes the tumor was very close and it was unable to separate the bronchus with a stapler then it became necessary to cut the bronchus with scissors and the proximal bronchial stump needed to be suture closed. When a lymph node was strongly stuck to the bronchus and it seemed to be necessary to remove the lymph node for complete lymph node dissection, the bronchus was damaged and that was also fixed with thoracoscopic suture technique (Figure 8).

Results
In our institution, open conversion to manage complications was 0.3% in consecutive 6,929 thoracoscopic surgery and 0.63% in thoracoscopic major lung resection since 2000.
In 2014 and 2015, 469 thoracoscopic major lung resections were intended to perform at the Department of Thoracic Surgery, Toranomon Hospital. Among them, there were two open conversion for the management of bleeding that count 0.4% of the procedure. Also 472 major lung resections were intended to perform in 2016 and 2017 with 2 open conversion. It was also 0.4% of the intended procedures. In 2014 to 2017, open conversion could be reduced to 0.4% of the major lung resections.
There was no procedure related mortality.
Discussion
The most important matter for the operations is safe and sufficient resection to remove the pathology. For the safe thoracoscopic management of the bleeding, it is necessary to set the criteria for open conversion. In our department, open conversion has been indicated when the blood loss exceeded 700 mL or the bleeding point was unable to identify.
It seemed to be important to acquire thoracoscopic suture technique to manage complications during thoracoscopic surgery (Figure 9). The Japan Society for Endoscopic Surgery has been running the Endoscopic Surgical Skill Qualification System and it is required to show the endoscopic suture skill.

Also, there are several techniques to manage complications in thoracoscopic surgery. It seemed to be important to include complication management in the training program for thoracoscopic surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: Not only the hospital but the society did not require the IRB for less than 10 case of report for case reports and surgical technique as well.
References
- 13th Nationwide Survey of Endocsopic Surgery in Japan. J Jpn Soc Endosc Surg 2016;21:655-810.
- Kohno T. Suture repair of the bronchial injury. Asvide 2018;5:537. Available online: http://www.asvide.com/article/view/25194
- Kohno T. Suture closure of the right main bronchial laceration in left subcarinal lymph node dissection. Asvide 2018;5:538. Available online: http://www.asvide.com/article/view/25195
- Kawashima S, Kohno T, Fujimori S, et al. Phrenic nerve reconstruction in complete video-assisted thoracic surgery. Interact Cardiovasc Thorac Surg 2015;20:54-9. [Crossref] [PubMed]
- Kohno T. ICS interposition: phrenic nerve reconstruction with intercostal nerve interposition. Asvide 2018;5:539. Available online: http://www.asvide.com/article/view/25196
- Kohno T. Thoracoscopic suture closure of the injured right atrium. Asvide 2018;5:540. Available online: http://www.asvide.com/article/view/25197
- Kohno T. Patch repair of the torn left A1+2 branch. Asvide 2018;5:541. Available online: http://www.asvide.com/article/view/25198