Role of 3D reconstruction in the evaluation of patients with lower segment oesophageal cancer
Introduction
Oesophageal cancer is one of the least studied and deadliest cancers throughout the world because of its extremely aggressive nature and poor survival rate (1). The incidence of oesophageal cancer is also high in China. Additionally, patients with oesophageal cancer are prone to early lymph node metastasis and distant metastasis, and local invasion is also commonly observed (2,3). Even after systematic treatment, the 5-year survival rate for this disease is still low (4). The Comprehensive Registry of Esophageal Cancer in Japan [2010] showed that the 5-year survival rates of patients treated using endoscopic mucosal resection, concurrent chemoradiotherapy, or oesophagectomy were 85.5%, 27.3%, and 55.5%, respectively (5).
In the treatment of oesophageal cancer, surgical treatment has always been the first choice for radical treatment (6). At present, routine preoperative evaluation of patients with oesophageal cancer includes the enhancement CT, which defines the lesion range, lesion extent and degree of external invasion (4,7). However, for the evaluation of the overall length of the lesion and its relative spatial location, the use of CT is limited.
Enhanced CT of the stomach is mainly used to assess the relationship between the gastric lymph nodes and the left gastric artery (8). The main examinations used to assess the location of the lesion are gastroscopy and upper gastrointestinal radiography. Of these methods, gastroscopy assesses lesion location mainly by measuring the distance from the central incisor to judge the segmentation of the lesion (9). However, this method is affected by individual factors, such as height and upper body length.
3D reconstruction has been used in evaluating the lungs and liver, but there is only little research on the application of 3D reconstruction for the oesophagus (10-12). The aim of this study was to evaluate the application of 3D reconstruction in the diagnosis and treatment of oesophageal cancer, which can assist in the development of diagnostic and treatment plans for oesophageal cancer and provide a better method of preoperative assessment.
Methods
Patients presented to the Department of Thoracic Surgery at the First Hospital of Jilin University from January 2014 to August 2015 were selected.
Inclusion criteria
- Pathological diagnosis of oesophageal cancer;
- Left thoracotomy with radical resection of oesophageal carcinoma;
- Having undergone enhanced chest CT and an enhanced stomach CT before surgery;
- Postoperative pathological findings were complete;
- Without preoperative chemotherapy, radiotherapy, or a combination of these treatments prior to surgery.
Exclusion criteria
- Lack of gastroscopy reports in medical records;
- Incomplete imaging data;
- Imaging data with serious artefacts and poor reconstruction results;
- Postoperative pathological findings of sarcomas;
- Postoperative pathological findings that suggested that the disease was a fundus disorder;
- Patients who have severe arrhythmia, history of thrombus or other diseases that can’t tolerate operation;
- Patients who received preoperative chemotherapy, radiotherapy, or both before.
A total of 72 patients were recruited, including 62 males and 10 females. The First Hospital of Jilin University approved the study protocol, and all the patients provided written informed consent for the procedure (number of ethnic approval: 2014122).
Experimental equipment and instruments
We used the Discovery TM 64 CT (U.S. General Company) for high-resolution (64-spiral) enhanced chest CT and enhanced stomach CT, Materialise Mimics 15.0 (Belgium Materialise Company) for three-dimensional (3D) reconstruction, and Photoshop CS4 (American Adobe Corporation) for dyeing.
Imaging data acquisition
Enhanced chest CT and enhanced stomach CT were enhanced using the Discovery TM 64 CT. The patients were positioned with their head forward in a supine position with their hands held up to their head. The scan ranged from the thoracic inlet to the umbilicus and used DICOM format image data.
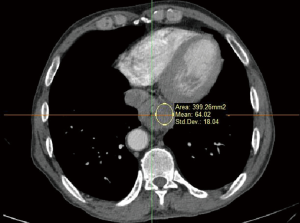
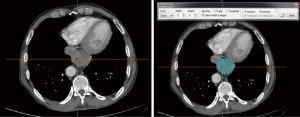
3D reconstruction
We collected patients’ information according to the inclusion and exclusion criteria. Data collection included enhanced chest CT and enhanced stomach CT DICOM files. Databases were built by Excel. We then imported files into Mimics’ 3D reconstruction software and browsed the original DICOM format two-dimensional images layer-by-layer. Using application software with tools, CT values and other specific parameters were measured from the two-dimensional images of the lesion location. The CT values for normal oesophageal tissues and diseased oesophageal tissues were measured and entered into the form.
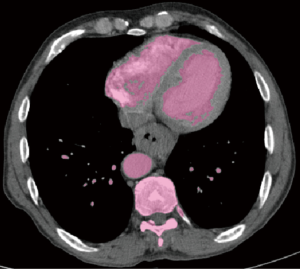
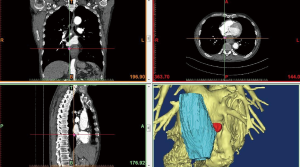
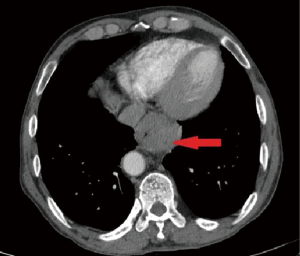
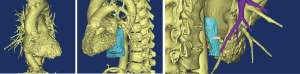
We subsequently created a blank layer and applied the surface editing software to edit and dye the location of the lesion according to the measured CT value. Then, the edited image file was created layer-by-layer to completed layer dyeing of the lesion. We then created a new blank layer and applied the surface editing software again to complete the labelling and dyeing of the adjacent tissue around the lesion. The layers of the tumour and adjacent tissues were reconstructed by surface reconstruction, and the reconstruction results could be displayed individually or in combination with display and multi-angle observation to assess the size, location and adjacent relationship of the tumour (Figures 1-6).
The length, thickness, volume and other related parameters of the tumour were measured by the software, and the results were entered into the database. The regional lymph nodes in the 7 groups and the 8 groups in the mediastinum were carefully observed by chief physicians. The lymph nodes were reconstructed, and the reconstructed results were compared with the postoperative pathological results. The positive and negative lymph nodes were labelled, the related parameters of the lymph nodes were measured using software tools, and the results were entered into the database.
Statistical analysis
IBM SPSS 19.0 was used to analyse all the data. All the data were averaged over three measurements. The t-test was used to compare the means of the two groups, and variance analysis was used among the groups, where P<0.05 indicated a significant difference.
Results
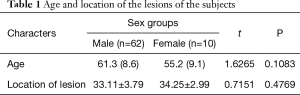
The age of the patients ranged from 45 to 85 years, and the average age was 61.3 (8.6) years. Gastroscopy was performed on all the patients. The gastroscope was able to pass through the oesophagus successfully in 48 cases but was unsuccessful in 24 cases. The location of the lesion ranged from 30 to 42 cm among the 48 cases. Detailed information is shown in Table 1 by sex groups.
Full table
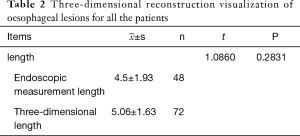
We conducted a 3D reconstruction visualization of the oesophageal lesions for all the patients and measured the lesion length by endoscopy in the 48 cases in whom the gastroscope was able to pass through the lesion successfully. The endoscopic measurement length and the 3D length were both longer than the pathological length, but there was no significant difference between the endoscopic measurement length and the 3D length (Table 2).
Full table
Table 3 presents the length, thickness and volume of the reconstructed tumours at different tumour stages. According to different pathological stages, the results of each measurement were analysed. The tumour volume, 3D length and 3D thickness were all different in the three different tumour stages.
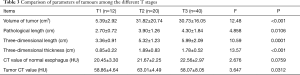
Full table
Among the 72 patients, the pathological results indicated that there were 46 patients with a positive lymph node (63.9%), and there were 12 cases where a lymph node was seen on CT images. We then conducted reconstruction for these cases. Of the remaining 26 patients with mediastinal lymph nodes that were negative on pathology, only 8 cases of oesophageal lymph nodes were observed and reconstructed. The correlation of the reconstructed results is shown in Table 3.
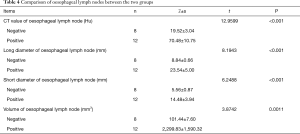
In the reconstructed data of positive lymph nodes, the length, diameter, volume, CT value and reconstruction of the lymph nodes in the negative group were significantly different compared with the positive group. Details are shown in Table 4.
Full table
Discussion
Key findings
In this study, we describe a novel 3D oesophageal reconstruction method combining both CT images and a 3D electromechanical rendering technique. 3D oesophageal reconstruction images are more intuitive and accurate than enhanced 2D CT images.
- This technique is an excellent non-invasive method for defining oesophageal position and stage.
- Increased knowledge of the location of oesophageal lesions was often used by the surgeon before surgery, and the surgical approach was modified accordingly. The considerable oesophageal 3D reconstruction would be show the location better which is beneficial to decide operational procedure before operation.
- The positive results for mediastinal lymph nodes were accurate, and they can be used for accurate assessment before surgery.
- 3D reconstruction of oesophageal cancer will improve the accuracy of traditional staging criteria for oesophageal carcinoma. In addition, this may also help to supplement information on the effects of radiotherapy and chemotherapy during the treatment period.
It has been reported that 3D-reconstruction has been applied to lung and liver, but there is little research on the use 3D reconstruction for the oesophagus (13,14). This may be due to the complex tissue construction and vessels that increase the difficulty of distinguishing the images. This study is based on two-dimensional enhanced CT images used to judge and mark the specific lesion level of oesophageal carcinoma. The reconstruction of the oesophagus in the diseased segment was performed using 3D-reconstruction. Using the same methods, oesophageal, peripheral, bronchial, and cardiovascular reconstructions were all completed.
This new method is superior to traditional gastrointestinal radiography and gastroscopy for observing the location of the diseased section of the oesophagus and for determining the surgical approach. In addition, the length and extent of the lesion are also important for the choice of treatment modality (15). The length and extent of the lesion are usually determined by gastroscopy. In this study, as a result of pathological changes, there were 24 cases that could not undergo gastroscopy, accounting for 33.3% of all the patients. For this portion of patients, only by using 2D images of the lesion could the cumulative level of the lesion’s specific length and range be estimated, and this method is not only low in accuracy but also has uncertainty for planning surgical treatment (16). The application of 3D reconstruction helps to evaluate the tissue and vessels prior to surgery, which improves the accuracy of assessment of the extent of disease. Furthermore, it is known that the malignancy of the tumours is associated not only with their length and volume but also with the degree of peripheral lymph node invasion and value of CT. In addition, 3D reconstruction of the oesophagus has a large advantage for the evaluation of the effects of chemotherapy and radiotherapy. Through 3D reconstruction, we can clearly observe changes in tumours and in the size of peripheral lymph nodes. Thus, the method used in this study is optimized for the standard of T-stage tumours. Thus the method in this study optimize for evaluating the lesion’s T stage before operation.
In this study, the visualization of oesophageal carcinoma was performed by 3D reconstruction with surface reconstruction. This method is not affected by the extent of oesophageal lesions, and it measures the length and extent of the lesion. In terms of the accuracy of the measurement, we compared the results of the gastroscopy with the results of the 3D reconstruction, using the pathological results as the standard. The results suggest that both gastroscopy and 3D reconstruction result in similar measurements. There are some differences with pathological measurements. However, the length of the 3D reconstruction was slightly larger than the actual length measured at pathology. Therefore, the therapeutic range is not affected by the range of the lesion measured by this method, and the final therapeutic effect is not affected.
It is important for rational diagnosis and treatment strategies to define the range of oesophageal carcinoma using 3D reconstruction.
Strengths and limitations
As far as we know, this study is the first report on the application of 3D oesophageal reconstruction in China. In addition, the image technology used in this study is superior to that used in previous research. However, there are still some limitations that should be mentioned. First, the sample size of this study may have been small, but it is still sufficient to describe the advantages of 3D oesophageal reconstruction compared with traditional methods. Second, all the patients were from a single centre—the First Hospital of Jilin University. Finally, a detailed point-to-point validation of fusion images was not performed.
Conclusions
The application of 3D reconstruction in oesophageal cancer is safe and effective. 3D reconstruction plays an important role in preoperative evaluation of tumours and their surrounding lymph nodes, and it can be used to evaluate the long-term efficacy of radiotherapy and chemotherapy for oesophageal cancer.
Acknowledgements
Funding: Application of Three-dimensional Reconstruction Technique in Preoperative Accurate Evaluation of Esophageal Cancer, MJR20170066, Young Scientists Research Foundation of Med Jaden; Application of 3D Simulation Technology in Diagnosis and Treatment of Thoracic Diseases, 20130604050TC, Science and Technology Department of Jilin Province.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by The First Hospital of Jilin University (No. 2014122) and written informed consent was obtained from all patients.
References
- Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol 2013;19:5598-606. [Crossref] [PubMed]
- Zhang QQ, Ni XG, He S, et al. Risk factors and survival analysis for synchronous esophageal carcinoma in patients with hypopharyngeal carcinoma. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2017;52:749-54. [PubMed]
- Chen J, Cai W, Lin Y, et al. Patterns and rates of abdominal lymphatic metastasis following esophageal carcinoma. PLoS One 2017;12. [Crossref] [PubMed]
- Yamabe Y, Kuroki Y, Ishikawa T, et al. Tumor staging of advanced esophageal cancer: combination of double-contrast esophagography and contrast-enhanced CT. AJR Am J Roentgenol 2008;191:753-7. [Crossref] [PubMed]
- Tachimori Y, Ozawa S, Numasaki H, et al. Comprehensive Registry of Esophageal Cancer in Japan, 2010. Esophagus 2017;14:189-214. [Crossref] [PubMed]
- Morita Y, Takase K, Yamada T, et al. Virtual CT thoracoscopy: preoperative simulation for thoracoscopic surgery of esophageal cancer. Abdom Imaging 2007;32:679-87. [Crossref] [PubMed]
- Holzapfel K, Rummeny EJ, Hannig C, et al. MSCT for staging and response evaluation of esophageal cancer. Radiologe 2007;47:101-9. [Crossref] [PubMed]
- Iino I, Sakaguchi T, Kikuchi H, et al. Usefulness of three-dimensional angiographic analysis of perigastric vessels before laparoscopic gastrectomy. Gastric Cancer 2013;16:355-61. [Crossref] [PubMed]
- Lewis RB, Mehrotra AK, Rodriguez P, et al. From the radiologic pathology archives: esophageal neoplasms: radiologic-pathologic correlation. Radiographics 2013;33:1083-108. [Crossref] [PubMed]
- Huang X, Yue S, Wang C, et al. Optimal three-dimensional reconstruction for lung cancer tissues. Technol Health Care 2017;25:423-34. [Crossref] [PubMed]
- Joemai RMS, Geleijns J. Assessment of structural similarity in CT using filtered backprojection and iterative reconstruction: a phantom study with 3D printed lung vessels. Br J Radiol 2017;90. [Crossref] [PubMed]
- Zhao J, Zhou XJ, Zhu CZ, et al. 3D simulation assisted resection of giant hepatic mesenchymal hamartoma in children. Comput Assist Surg (Abingdon) 2017;22:54-9. [Crossref] [PubMed]
- Shioyama Y, Jang SY, Liu HH, et al. Preserving functional lung using perfusion imaging and intensity-modulated radiation therapy for advanced-stage non-small cell lung cancer. Int J Radiat Oncol Biol Phys 2007;68:1349-58. [Crossref] [PubMed]
- Mineo TC, Schillaci O, Pompeo E, et al. Usefulness of lung perfusion scintigraphy before lung cancer resection in patients with ventilatory obstruction. Ann Thorac Surg 2006;82:1828-34. [Crossref] [PubMed]
- Krupski-Berdien G. MRI of esophagus. N staging and more.. Radiologe 2007;47:119-22. [Crossref] [PubMed]
- Kim SH, Lee JM, Han JK, et al. Three-dimensional MDCT imaging and CT esophagography for evaluation of esophageal tumors: preliminary study. Eur Radiol 2006;16:2418-26. [Crossref] [PubMed]