Pulmonary retransplantation
In the last 30 years, pulmonary transplantation has become the standard treatment for many end-stage benign lung diseases. Pulmonary transplantation has developed rapidly in the past decade. According to official data from the International Society of Heart and Lung Transplantation (ISHLT), a total of 1,934 adult pulmonary transplantations were performed worldwide in 2003, and 3,893 were performed in 2013. For patients undergoing initial pulmonary transplantation, the 5-year survival rate reported in the literature is approximately 50%, which was lower than the reported survival rates of 71% in heart transplantation, 70% in kidney transplantation, and 67% in liver transplantation. Graft failure caused by chronic rejection or bronchiolitis obliterans syndrome (BOS) is the major factor affecting long-term survival after pulmonary transplantation. Literature reports indicate that the probability of occurrence of BOS within 5 years after initial pulmonary transplantation is approximately 50%. For severe BOS, pulmonary retransplantation is the only effective means to improve survival. The first pulmonary retransplantation surgery in the world was completed in 1985, and the number of retransplantation cases has increased in recent years along with the number of initial transplantation cases. In general, the risk involved with retransplantation is greater than that of the initial transplantation, and the prognosis is also worse than that of the initial transplantation. Nevertheless, with the development of new surgical techniques and immunological drugs, the outcome of retransplantation has significantly improved in recent years. The 1-year survival rate of pulmonary retransplantation in the 1990s was approximately 47%, and data from the United Network for Organ Sharing (UNOS) database collected during 2004–2013 showed an improvement in survival to approximately 71.1%. Although this is still lower than the survival associated with initial transplantation, it was indeed a significant improvement (1,2). This study will review the current status of retransplantation and describe developments in retransplantation, the rational selection of patients, and the prognosis.
History of pulmonary retransplantation
Before the 1990s, as pulmonary transplantation was just in its infancy and all the related technologies were still immature, the number of patients undergoing pulmonary retransplantation was very small. The pulmonary retransplantation registration system was developed by Novick et al. in 1995. In 1998, this team analyzed 230 cases of pulmonary retransplantation in 47 transplantation centers, reporting a 1-year survival rate of 47%, significantly lower than the 73% observed for initial transplantation (1). A few studies on retransplantation have been conducted since then. In 2003, Brugiere et al. (3) described 15 cases of retransplantation due to BOS; 40% of the patients could not get out of bed before the retransplantation and the postoperative 1-year survival rate was 60%, which again raised expectations for the outcome of retransplantation. With the increase in the cases of initial pulmonary transplantation, retransplantation has also increased rapidly. According to a report by the organ procurement transplantation network (OPTN), pulmonary retransplantation accounted for 2.9% of all pulmonary transplantation in 2003, which increased to 5.3% in 2005. The outcomes of pulmonary retransplantation have continued to improve in recent years. In an analysis of the UNOS registration data, Kawut et al. (4) found that the outcomes of retransplantation between 2001 and 2006 were better compared to before 2001. Improvements in modern pulmonary transplantation are likely related to improvements in pulmonary preservation technology and the development of immunosuppressive drugs. The appropriate selection of cases may also have contributed to these improvements. The outcomes of surgery for BOS were significantly better than those of retransplantation for short-term graft failure and irreversible airway complications. Retransplantation for BOS is increasingly favored. Aigner et al. at the Vienna Transplantation Center (5) retrospectively analyzed 46 cases of pulmonary retransplantation, including 19 cases of BOS, 23 cases of primary graft failure and four cases of airway complications. The survival rates at 30 days, one year and five years after surgery were 89.2%, 72.5%, and 61.3%, respectively. The survival rate of the BOS group was similar to that of patients undergoing initial pulmonary transplantation. In 2006, the Hannover Transplantation Center (6) reported the outcomes of many cases of lung retransplantation at their center. Of the 614 cases of pulmonary transplantation, 54 involved retransplantation. The 5-year survival rate for pulmonary retransplantation due to BOS was 62%, essentially similar to the 63% 5-year survival rate for initial pulmonary transplantation. In 2008, Biswas et al. (7) investigated 29 cases among 419 patients with chronic graft failure undergoing retransplantation and found no significant difference between the 1- and 5-year survival rates of these patients and those of patients undergoing initial transplantation. These reports indicate that the outcomes of pulmonary retransplantation have greatly improved and that chronic graft failure is the most appropriate surgical indication for retransplantation.
Indications and contraindications of pulmonary retransplantation
Currently, the main reasons for retransplantation include early severe primary graft failure, irreversible airway complications (such as anastomosis dehiscence), and end-stage BOS. The main indications and contraindications currently considered are listed in Table 1.
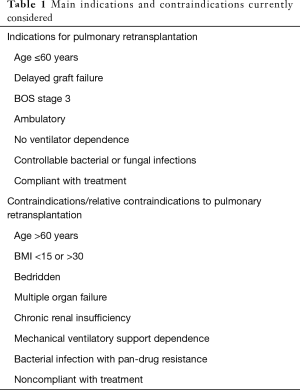
Full table
Factors associated with the prognosis of pulmonary retransplantation
There are many factors affecting the prognosis of pulmonary retransplantation. The factors that have been identified in the literature include the reason for retransplantation, the number of cases of transplantation performed each year in the institution, the interval between initial transplantation and retransplantation, the patient’s pre-transplantation functional status, the time of retransplantation, the surgical procedure for retransplantation, and the age of the patient at the time of retransplantation. (I) The reason for retransplantation. The prognosis of retransplantation due to acute graft failure and airway dehiscence is poor, whereas the prognosis of retransplantation due to end-stage BOS is better. In a study conducted by Strueber et al. (6), out of 614 cases of pulmonary transplantation, a total of 54 involved retransplantation. The authors found that the prognosis of retransplantation due to BOS was better, with a 1-year survival rate of 78% and a 5-year survival rate of 62%, which was not significantly different from the prognosis of initial pulmonary transplantation. However, for patients undergoing retransplantation due to early graft failure and anastomotic dehiscence, and patients requiring mechanical ventilation prior to surgery, the 1-year survival rate after retransplantation was approximately 50%. Thus, the reason for retransplantation is an important factor affecting the prognosis. (II) Number of cases of retransplantation. Novick et al. (1) analyzed retransplantation at 35 medical institutions and found that the 2-year survival rates for retransplantation in the institutions that had performed more than five retransplantation cases were significantly higher than those performed in institutions with fewer than five cases. (III) The interval between initial transplantation and retransplantation. Kawut et al. (4) found that patients who underwent retransplantation within 30 days of the initial transplantation had a significantly higher mortality rate than those undergoing retransplantation after 30 days or more. In a retrospective multivariate analysis of data on 604 patients who underwent lung retransplantation in 2004–2013, Thomas et al. (2) found that patients who underwent retransplantation at more than one year after initial transplantation had a significantly better prognosis than those with a retransplantation interval of less than 1 year. (IV) Preoperative functional status. Novick et al. (8) analyzed 139 cases of pulmonary retransplantation in 34 institutions and found that approximately 29% of the patients were ambulatory before surgery (walking with or without assistance for more than 50 m). The results of univariate and multivariate analyses indicated that these patients’ prognosis was better than that of the patients who could not get out of bed. (V) The time of retransplantation. In general, with the development of technology and drug research and improvements in the understanding of retransplantation, the outcomes of pulmonary retransplantation have improved over time, and they are better now than they were in the early years of this procedure. Of course, improvements in outcomes are also related to changes in the indications and patient selection for pulmonary transplantation and the increase in the proportion of patients with BOS in pulmonary retransplantation in recent years. In a study by Kawut et al. (4), the prognosis of pulmonary retransplantation surgeries performed before 2001 was significantly worse than that of retransplantation surgeries performed in 2001–2006. (VI) The surgical procedure used for retransplantation. In an analysis of 325 retransplantation patients registered in the Organ Acquisition and Transplantation Network database (OPTN), Kon et al. (9) found that the prognosis of patients who underwent double lung transplantation and contralateral lung transplantation was significantly better than that of the patients with ipsilateral lung transplantation. In a study by Thomas et al. (2), the results of multivariate analyses showed that the prognosis of patients undergoing double lung retransplantation was significantly better than that of the patients undergoing single lung retransplantation. (VII) The age of the patient at retransplantation. Hall et al. (10) analyzed the prognosis of 542 patients who underwent pulmonary transplantation, of whom 87 underwent retransplantation. The results showed that the prognosis of recipients aged 50–60 years and older was significantly worse than that of the younger patients. In addition, they found that some donor characteristics may also affect transplant recipients’ prognosis. For example, it has been reported that the prognosis of retransplantation is significantly poor when the cause of death of the donor is a cerebrovascular accident. In addition, Novick et al. (8) reported that retransplantation involving unmatched CMV status between the donor and recipient had a poor prognosis. Kawut et al. (4) reported that the prognosis of patients undergoing retransplantation with lungs from male donors was significantly worse than for patients who had female donors.
Critical issues in retransplantation
Although the outcomes of retransplantation have improved over time, there is still a certain gap in the overall surgical risk and prognosis compared with initial pulmonary transplantation, which may be related to the following factors. (I) The influence of initial transplantation surgery. Retransplantation patients may have severe pleural adhesions due to the initial transplantation surgery. Their anatomy may also deviate from the norm. After the initial operation, structures are less easily identified, and accidental injury may easily occur. Therefore, there may be an increased risk of surgical complications, such as intraoperative hemorrhage. In addition, when the anastomosis is performed, in order to maintain a good bronchial blood supply and avoid poor blood supply to the anastomosis, the original bronchial anastomosis is usually excised and the proximal segment is anastomosed to the donor bronchus. After the anastomosis is completed, the pericardium, the surrounding pleura, the intercostal muscle, or the omentum are generally wrapped around the anastomotic stoma to increase the chance of healing. (II) Long-term drug effects. The long-term use of immunosuppressants such as FK506 after initial transplantation affects renal function. Renal insufficiency itself is associated with hypertension, osteoporosis, anemia, malnutrition, and neurological disorders, which may lead to adverse events. (III) Immune problems. Retransplantation patients are in a state of chronic immunosuppression due to the long-term use of immunosuppressive agents. It is questionable whether these patients need an initial large induction dose of immunosuppressants. Large doses of immunosuppressive agents greatly increase the risk of infection after retransplantation, and infection is still the primary cause of death in retransplantation. Currently, there is no standard plan for changes in immunosuppression regimens. (IV) Criteria to assess the risk of retransplantation and choose appropriate cases. Although the risk of retransplantation is high and the prognosis is poor, it has been reported in the literature that the prognosis of some patients is equivalent to that of patients undergoing initial pulmonary transplantation (for instance, patients undergoing retransplantation due to BOS). For early post-retransplantation complications such as early graft failure and anastomosis dehiscence, postoperative ventilator support, ECMO support, and a large amount of intravenous drugs are often required. These patients are generally in very poor condition, their systemic function is altered, and the re-anastomosis is often in the edema phase, making healing more difficult and thus increasing the risk of poor surgical outcomes. Therefore, in cases of retransplantation due to early complications, assessment of surgical risk and appropriate patient selection to maximize the value of the organs represent a major challenge.
Pulmonary retransplantation experience at the Shanghai Chest Hospital
Since our hospital started performing pulmonary transplantation in 2003, four retransplantation surgeries have been performed. The indication for all the cases was BOS after initial pulmonary transplantation. All four patients underwent unilateral pulmonary transplantation. One patient had initially undergone single lung transplantation, which was followed by contralateral lung retransplantation. The remaining patients had initially undergone double lung transplantation and underwent retransplantation of a single lung. The ages of the four patients at retransplantation were 39, 44, 49, and 71 years. The intervals between the two lung transplantations were 52, 51, 101, and 78 months, respectively. Two patients had a history of intubation due to preoperative CO2 retention. No cardiopulmonary bypass was used in any of the cases. The three patients who underwent single-lung retransplantation after double-lung initial transplantation has severe adhesions in the chest cavity. However, the most difficult part of the surgery was exposure of hilar structures, especially for the pulmonary arteries, the bronchus and the pulmonary veins, which required significant care to avoid catastrophic hemorrhage. Of the four patients, two (including the patient who underwent contralateral lung retransplantation) developed anastomotic fistulas. The other two cases were discharged without any complications. In terms of postoperative management, our immunosuppression strategy was similar to that used for initial transplantation, and Simulect (Basiliximab) was used for induction. Afterwards, the triple combination of FK506, mycophenolate mofetil, and prednisone was routinely used. However, we have recently become more aggressive hormonal modulation, mainly due to the relatively high rate of anastomotic complications after retransplantation. The patients who survived the longest after retransplantation have survived for nearly four years and continue to have good outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Novick RJ, Stitt LW, Al-Kattan K, et al. Pulmonary retransplantation: predictors of graft function and survival in 230 patients. Pulmonary Retransplant Registry. Ann Thorac Surg 1998;65:227-34. [Crossref] [PubMed]
- Thomas M, Belli EV, Rawal B, et al. Survival After Lung Retransplantation in the United States in the Current Era (2004 to 2013): Better or Worse? Ann Thorac Surg 2015;100:452-7. [Crossref] [PubMed]
- Brugiere O, Thabut G, Castier Y, et al. Lung retransplantation for bronchiolitis obliterans syndrome: long-term follow-up in a series of 15 recipients. Chest 2003;123:1832-7. [Crossref] [PubMed]
- Kawut SM, Lederer DJ, Keshavjee S, et al. Outcomes after lung retransplantation in the modern era. Am J Respir Crit Care Med 2008;177:114-20. [Crossref] [PubMed]
- Aigner C, Jaksch P, Taghavi S, et al. Pulmonary retransplantation: is it worth the effort? A long-term analysis of 46 cases. J Heart Lung Transplant 2008;27:60-5. [Crossref] [PubMed]
- Strueber M, Fischer S, Gottlieb J, et al. Long-term outcome after pulmonary retransplantation. J Thorac Cardiovasc Surg 2006;132:407-12. [Crossref] [PubMed]
- Biswas Roy S, Panchanathan R, Walia R, et al. Lung Retransplantation for Chronic Rejection: A Single-Center Experience. Ann Thorac Surg 2018;105:221-7. [Crossref] [PubMed]
- Novick RJ, Schafers HJ, Stitt L, et al. Recurrence of obliterative bronchiolitis and determinants of outcome in 139 pulmonary retransplant recipients. J Thorac Cardiovasc Surg 1995;110:1402-13; discussion 13-4. [Crossref] [PubMed]
- Kon ZN, Bittle GJ, Pasrija C, et al. The Optimal Procedure for Retransplantation After Single Lung Transplantation. Ann Thorac Surg 2017;104:170-5. [Crossref] [PubMed]
- Hall DJ, Belli EV, Gregg JA, et al. Two Decades of Lung Retransplantation: A Single-Center Experience. Ann Thorac Surg 2017;103:1076-83. [Crossref] [PubMed]


