CO2 during single incisional thoracoscopic bleb resection with two-lung ventilation
Introduction
Video-assisted thoracoscopic surgery (VATS) is widely accepted for various thoracic surgeries. VATS for primary spontaneous pneumothorax is traditionally performed with one-lung ventilation (OLV) using a double-lumen endotracheal tube (DLT) or endobronchial blocker (1).
Thanks to development of surgical techniques and instruments, single-incision thoracoscopic surgery (SITS) was introduced (2-7). This surgical technique requires only one small incision (2–3 cm) and has several benefits compared to conventional three- or two-port VATS. SITS may produce less intercostal pain (5,7), decrease surgical trauma (2), and improve surgeon hand-eye coordination because of the similar situation to that of open thoracotomy (6). SITS carries several benefits, while general anesthesia with OLV has been accepted as a standard method without sufficient evidence because of the possibly limited surgical view (1,8). OLV provides the best surgical condition with a static, collapsed lung and carries various inevitable disadvantages, including ventilation/perfusion mismatch, hypoxemia, secretion retention, consolidation, edema in the operative lung (9,10), and mechanical and humoral lung injuries in the ventilated lung (11). Whether one performs bronchoscopy or not (12), establishing OLV requires more time than two-lung ventilation (TLV) with a single lumen endotracheal tube. VATS under small-tidal TLV (ST-TLV) is a proven alternative to OLV for bleb resection (13), and we reported adequate ventilator settings for ST-TLV during VATS bleb resection (14). The feasibility of CO2 insufflation with ST-TLV to ensure an appropriate surgical field was demonstrated (3). However, CO2 insufflation has potential complications including arterial hypercapnia and related cardiovascular response, CO2 embolism, and hypotension resulting from impaired venous return (15).
Thus, in this prospective randomized study, we compared surgical fields and several ventilator-associated variables between ST-TLV with or without CO2 insufflation during SITS bleb resection. We also developed a grading system for surgical field evaluation to enable an objective result.
Methods
This study was approved by the Korea University Guro Hospital Ethics Committee (MD16068-001) and informed consent was obtained from all included patients. From October 2012 to November 2014, a total of 130 patients who planned to undergo elective SITS bleb resection due to primary spontaneous pneumothorax were evaluated for eligibility. The inclusion criteria were similar to those of our previous study (14): American Society of Anesthesiologists (ASA) physical status classification I or II, age 19–64 years, complicated pneumothorax (defined as persistent air leak, hemothorax, lung re-expansion failure, bilateral pneumothorax, or tension pneumothorax), visible blebs on computed tomography, or ipsilateral recurrent episodes. Of the 130 screened patients, 88 were included in this study. The exclusion criteria were first attack without complications, suspected significant pleural adhesion on radiology, planned surgery for open thoracotomy, higher ASA classification over II, and patient refusal. Eight patients were excluded (2 with ASA classification III, 3 who refused, 3 with expected pleural adhesions), so a total of 80 patients were subjected to the study protocol and statistical analysis.
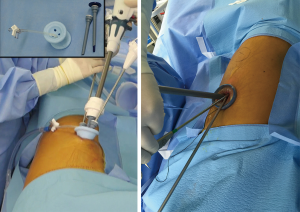
All patients underwent surgery under general anesthesia. Each patient was assigned into group C (CO2 insufflation) or group NC (no CO2 insufflation) using a block randomization method. Under standard patient monitoring (electrocardiography, oxygen saturation, noninvasive blood pressure, end-tidal CO2), general anesthesia was induced, and the trachea was intubated with a single-lumen endotracheal tube (ID 7.0 for women and ID 8.0 for men) as described in our previous trial (14). Mechanical ventilation was applied using the full tidal volume (FTV) or small tidal volume (STV) setting. The FTV was 10 mL/kg tidal volume (TV), 12 cycles/min respiration rate (RR), 1:2 inspiratory-to-expiratory (I:E) ratio without positive end expiratory pressure (PEEP), and 0.5 FiO2 with N2O. The STV was 5 mL/kg TV, 15 cycles/min RR, 1:2 I:E ratio without PEEP, and 0.5 FiO2 with N2O. After the anesthesia induction, FTV was applied first, while STV was initiated just after position changed from supine to the lateral decubitus. With the patient in the lateral decubitus position, surgery was performed with a 1.5–2.5 cm skin incision made at the 6th or 7th intercostal space where the chest tube was inserted. In group C, a special multiple-access single port (SILS™ port; Covidien, Mansfield, MA, USA) was inserted at the incision site and 6 mmHg CO2 was continuously insufflated into the thoracic cavity via the SILS channel during the operation (Figure 1). Surgery was conducted using endoscopic instruments and flexible endostaplers under 5-mm thoracoscope to resect any identified bullae or blebs. The stapler line was reinforced using polyglycolic acid sheet (Neovil, Gunze Limited Medical Division, Japan) and fibrin glue. Then CO2 flow was stopped, and a resected lung specimen was pulled out through the incision after SILS removal. Finally, a 16-Fr chest tube was inserted toward the lung apex to provide drainage. In group NC, surgery was performed through the same incision with a wound protector/retractor (Alexis® wound protector/retractor; Applied Medical, CA, USA) instead of the SILS (Figure 1). Otherwise, the surgical procedures were similar except for the CO2 insufflation.
Patient age, sex, height, and weight were collected as demographic data. Airway pressure and arterial blood gas analysis (ABGA) parameters (pH, PaO2, and PaCO2) were measured 5 minutes after FTV, STV, and CO2 insufflation. Operation time (the time from incision to wound dressing) and anesthesia recovery time (the time from the all anesthetics discontinue to transfer to post-anesthetic care unit) were recorded. Postoperative chest tube indwelling duration, length of hospital stays, complications including persistent air leakage, infection, pleural effusion, bleeding, and pneumothorax recurrence within 3 months. Postoperative nausea and vomiting was also recorded when the patients required the antiemetics.
For safety concerns, airway pressure and SpO2 were continuously observed during the operation; whenever we observed signs related to hypercapnia or hypoventilation, the study protocol was stopped, and the patient was managed according to general guidelines for OLV with an endobronchial blocker.
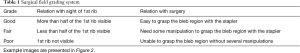
All surgical procedures were recorded as video files and each surgical field was graded later by one person who did not participate in the anesthesia or surgery. Surgical field grading was performed at the time of thoracoscope introduction into the operated side of the lung and at the time of bleb resection with the stapler (Table 1, Figure 2). All records of the surgical field grading were collected in a separated case report form containing only the case number.
Full table
The statistical analysis was performed using IBM SPSS 22.0 (PASW Statistics for Windows; SPSS, Chicago, IL, USA). According to the results of the Shapiro-Wilk test for normality, continuous variables were analyzed using Student’s t-test, while categorical variables were analyzed using the chi-square test. P values <0.05 were considered statistically significant.
Before this trial initiation, a power analysis was performed based on the retrospective pilot study. We investigated recorded video files of SITS bleb resections performed in our hospital and the same method described below was applied to the surgical field grading. The estimated effect size was 0.353 with α error of 0.05, power of 0.8, χ2 test with 2 degrees of freedom for a required sample size of 78 to detect the surgical field grading differences during bleb resection. Considering a 10% dropout rate, a total of 87 patients was required to fulfill the statistical assumptions.
Results
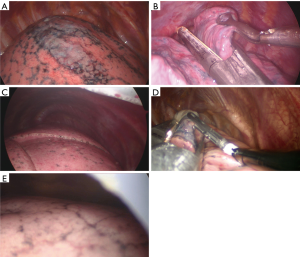
A total of 80 patients were included in the statistical analysis (40 cases in each group). There were no intergroup differences (Table 2).
Full table
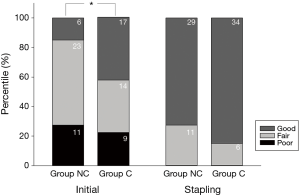
At the beginning of the surgery (the time of thoracoscope introduction), the evaluated surgical field grade was statistically different (Pearson χ2[2] =7.650, P=0.022, Cramér’s V =0.31). The most frequent incidence in group NC was fair (57.5%), while that in group C was good (42.5%). However, the surgical fields at the time of bleb resection with the stapler did not differ between groups (Pearson χ2[2] =1.867, P=0.172, Cramér’s V =0.15), while surgical fields were graded as mostly good (72.5% in group NC and 85.0% in group C; Figure 3).
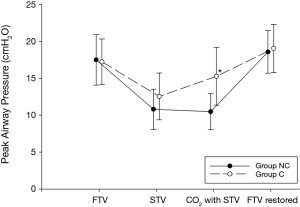
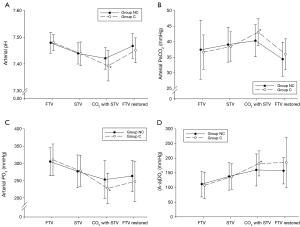
The mean operation time was longer in group C than in group NC (31.2±8.3 minutes in group NC and 36.4±10.8 minutes in group C, mean difference =5.2, 95% CI: 0.9–9.4, t[78] =2.398, P=0.019, Cohen’s d =0.59). During the CO2 insufflation, group C presented an increased mean peak airway pressure (10.5±2.4 cmH2O in group NC vs. 15.5±3.7 cmH2O in group C; mean difference =5.0, 95% CI: 3.6–6.4, t[67] =7.071, P=0.009, Cohen’s d =0.32; Figure 4), decreased pH (7.42±0.04 in group NC vs. 7.39±0.06 in group C; mean difference =0.03, 95% CI: 0.05–0.06, t[78] =2.572, P=0.012, Cohen’s d =0.58), increased pCO2 (40.4±5.1 mmHg in group NC vs. 43.1±4.4 mmHg in group C; mean difference =2.7, 95% CI: 0.6–4.9, t[78] =2.558, P=0.012, Cohen’s d =0.57), decreased pO2 (253.0±54.8 mmHg in group NC vs. 227.4±44.0 in group C; mean difference =25.6, 95% CI: 3.5–47.8, t[78] =2.305, P=0.024, Cohen’s d =0.52; Figure 5) compared to group NC. The alveolar-arterial oxygen difference [(A-a)DO2] was also progressively increased during operation. In group C, (A-a)DO2 was significantly increased during CO2 insufflation (160.0±54.6 mmHg in group NC vs. 182.2±42.8 mmHg in group C; mean difference =22.2, 95% CI: 0.4–22.2, t[78] =2.024, P=0.046, Cohen’s d =0.45; Figure 5).
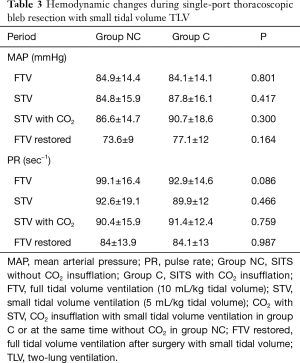
Hemodynamic changes during surgery were not statistically different between the two groups (Table 3). No patients presented signs of hypercapnia or hypoventilation.
Full table
Anesthesia recovery time was 16.1±5.2 min for group NC and 17.5±8.3 min for group C (mean difference =1.4, 95% CI: −1.7 to 4.5, t[78] =0.903, P=0.369, Cohen’s d =0.2). Postoperative chest tube indwelling duration and length of hospital stays were not statistically different (mean difference =0.3, 95% CI: −0.2 to 0.8, t[78] =1.201, P=0.234, Cohen’s d =0.3, and mean difference =0.08, 95% CI: −0.53 to 0.67, t[78] =0.248, P=0.805, Cohen’s d =0.1, respectively). Postoperative complications were observed in 12.5% for group NC and 10.0% patients for group C (Pearson’s χ2[1] =0.125, P=0.723, Cohen’s Φ =0.1). Postoperative nausea and vomiting frequencies were statistically insignificant (Pearson’s χ2[1] =0.556, P=0.456, Cohen’s Φ =0.1; Table 4).

Full table
Discussion
Our results revealed that small-incision SITS bleb resection with ST-TLV provided a similar surgical field without CO2 insufflation to that of the same surgical technique with artificial CO2 pneumothorax. Using CO2 produced a more favorable field at the beginning; at the middle of surgery, especially stapling for bleb resection (the most important procedure in this kind of surgery), the surgical field did not differ by the use or nonuse of CO2 insufflation. Moreover, operation time was slightly shorter without CO2 use than with CO2 insufflation. For iatrogenic CO2 insufflation during SITS, it is inevitable to use a special multiple-access single port, which is more expensive compared to the wound protector/retractor, 262.1 and 91.1 USD respectively in our country. CO2 insufflation also produced its inevitable consequences including increased arterial CO2 partial pressure, increased peak airway pressure, and decreased (A-a)DO2; fortunately, all of these changes during CO2 insufflation were within the physiologic range. However, these changes can be problems if the surgery lasts longer than expected or when the patient is at risk of abnormal ventilation, even from subtle changes.
Most articles on SITS bleb resection focused on the feasibility of that surgery without objective evidence (3,4,13,16). They reported the feasibility of SITS with CO2 insufflation in terms of operation time, anesthesia time, postoperative complications, hospital stay, subjective operation field evaluation and physiologic changes (3,4,13). One author reported that a feasible surgical field could be acquired using a bidirectional anchoring suture during single-port thoracoscopic surgery without CO2 (17). These results would carry biases of the subjective assessment of surgical field and of operation time, which are considerably affected by surgeon skill. Using a simplified and objective scale, we compared the surgical fields of SITS bleb resection (Table 1, Figure 2). Our grading system is simple to understand. We evaluate the surgical view using the sight of the 1st rib and anticipated stapling line of the bleb. If the operation side lung volumes were decreased enough to leave the space for thoracoscopic instrument movements, the surgical fields near the cupola would expose the significant part of the 1st rib. If not, the lung will increase its volume during inspiration, resulting in a limited view of the 1st rib. Before stapling, blebs should be lifted using grasping forceps and an imaginary stapling line should be decided. To perform these procedure, lung tissues around the bleb should be collapsed. If the operated lung re-expands at every inspiration cycle, the next stapling procedure would be impossible. Therefore, we considered the need for some manipulation to grasp the bleb region with the stapler concurrently with exposure of the 1st rib. Under these simple considerations, our grading system guarantees objectivity in the surgical field evaluation and enables comparison between SITS with and without CO2 insufflation.
Using our grading system, surgical fields during SITS bleb resection were not significantly different at the time of bleb resection despite the initial grade being much higher in the group without CO2. However, the mean operation time was 5 minutes longer in the group with CO2. SILS has its own bulky structure compared to the wound protector, it requires more skillful insertion technique through small incision. Also, introduction and manipulation of endoscopic instruments through SILS could take time and limited compared to the wound protector. Due to limited maneuverability through SILS, some endoscopic forceps with a joint at the distal part of it (articulating instruments) provide to enhance maneuverability. However, wound protector has superior aspects compared to SILS because all kinds of conventional endoscopic instruments could be used through one single incision which are more familiar to the most surgeons. That is, SITS bleb resection without CO2 insufflation is a simplified feasible procedure that less takes time (Figure 6).

Although an iatrogenic CO2 pneumothorax could provide a superior surgical field from the start of the operation, it carries various adverse aspects. It could deteriorate the pH and PaCO2 in patients with decreased lung function, older age, or a smoking history (19). In several reports, CO2 insufflation did not produce hypercapnia in the operation of relatively short duration (20,21). However, the more evidences about adverse response to CO2 insufflation were reported including hemodynamic suppression and oxygenation deterioration even a low intrapleural pressure (22-24). In our study, hemodynamic parameters were maintained without deterioration. The patients included in this study were mostly young adults with a mean age in their late twenties and no lung disease except pneumothorax. Surgery usually finished within 30 minutes. A young and healthy lung and short operation time could be major factors for preventing hemodynamic deterioration. However, most changes in ABGA were in the physiologic range—including lowered pH, increased PaCO2, decreased PO2, and increased (A-a)DO2—creating the possibility of physiologic derangement when the surgery continues over a considerable amount of time or patients are vulnerable (elderly, with underlying lung disease, smoking status).
There are some limitations to our study. First, in our study population, no patients had an underlying lung disease, which could be a cause of increased residual volume. If residual volume or alveolar closing volume of the lung increased, this diseased lung would not tend to be collapsed by atmospheric pressure. The effectiveness of SITS without CO2 insufflation should be evaluated in the patient with a diseased lung. Second, long-term follow-up results were not considered in our study. Considering the ipsilateral recurrence of primary spontaneous pneumothorax, age, and pleurodesis is important (25), despite insufficient evidence, it is difficult to consider that SITS without CO2 insufflation produces more recurrence than other surgical types. Other factors including pain score, and patient satisfaction were not evaluated in our study. Still, arguments about postoperative pain persist (26,27), several advantages have been suggested (28), and further studies are needed to elucidate these points. Third, the grading tool developed and applied in this study, was not confirmed any external validation. Despite we considered every possible circumstance, it may not be reflecting or capturing any perceived advantages or disadvantages of applied ventilation methods.
In conclusion, SITS without CO2 insufflation provides a sufficient surgical field compared to CO2 insufflation for bleb resection. At the beginning of surgery, the surgical field without CO2 was unfavorable, but it was not considerably different during bleb resection. Instead, the operation time was shorter than surgery with CO2 insufflation. During CO2 insufflation, ABGA values and oxygen diffusion capacity changed but remained in the physiologic range. However, these changes could advance into the pathologic range in patients with certain risk factors.
Acknowledgements
Funding: This work was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI17C0654).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Korea University Guro Hospital Ethics Committee (MD16068-001) and informed consent was obtained from all included patients.
References
- Hatz RA, Kaps MF, Meimarakis G, et al. Long-term results after video-assisted thoracoscopic surgery for first-time and recurrent spontaneous pneumothorax. Ann Thorac Surg 2000;70:253-7. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Han KN, Kim HK, Lee HJ, et al. Single-port thoracoscopic surgery for pneumothorax under two-lung ventilation with carbon dioxide insufflation. J Thorac Dis 2016;8:1080-6. [Crossref] [PubMed]
- Kara M, Alzafer S, Okur E, et al. The use of single incision thoracoscopic surgery in diagnostic and therapeutic thoracic surgical procedures. Acta Chirurgica Belgica 2013;113:25-9. [Crossref] [PubMed]
- Liu CY, Lin CS, Shih CH, et al. Single-port video-assisted thoracoscopic surgery for lung cancer. J Thorac Dis 2014;6:14-21. [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
- Ciriaco P, Muriana P, Bandiera A, et al. Video-assisted thoracoscopic treatment of primary spontaneous pneumothorax in older children and adolescents. Pediatr Pulmonol 2016;51:713-6. [Crossref] [PubMed]
- Cohen E. Physiology of the lateral position and one-lung ventilation. Chest Surg Clin N Am 1997;7:753-71. [PubMed]
- Dunn PF. Physiology of the lateral decubitus position and one-lung ventilation. Int Anesthesiol Clin 2000;38:25-53. [Crossref] [PubMed]
- Lohser J, Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and collapsed lung. Survey Anesthesiol 2016;60:98-9. [Crossref]
- Amin N, Tarwade P, Shetmahajan M, et al. A randomized trial to assess the utility of preintubation adult fiberoptic bronchoscope assessment in patients for thoracic surgery requiring one-lung ventilation. Ann Card Anaesth 2016;19:251-5. [Crossref] [PubMed]
- Kim H, Kim HK, Choi YH, et al. Thoracoscopic bleb resection using two-lung ventilation anesthesia with low tidal volume for primary spontaneous pneumothorax. Ann Thorac Surg 2009;87:880-5. [Crossref] [PubMed]
- Lee DK, Kim HK, Lee K, et al. Optimal respiratory rate for low-tidal volume and two-lung ventilation in thoracoscopic bleb resection. J Cardiothorac Vasc Anesth 2015;29:972-6. [Crossref] [PubMed]
- Suarez-Pierre A, Terasaki Y, Magruder JT, et al. Complications of CO2 insufflation during endoscopic vein harvesting. J Card Surg 2017;32:783-9. [Crossref] [PubMed]
- Song IH, Lee SY, Lee SJ. Can single-incision thoracoscopic surgery using a wound protector be used as a first-line approach for the surgical treatment of primary spontaneous pneumothorax? A comparison with three-port video-assisted thoracoscopic surgery. Gen Thorac Cardiovasc Surg 2015;63:284-9. [Crossref] [PubMed]
- Son BS, Kim DH, Lee SK, et al. Small single-incision thoracoscopic surgery using an anchoring suture in patients with primary spontaneous pneumothorax: a safe and feasible procedure. Ann Thorac Surg 2015;100:1224-9. [Crossref] [PubMed]
- Lee DK, Kim H, Kim HK, et al. Comparison of differences between SITS with and without CO gas insufflation. Asvide 2018;5:709. Available online: http://www.asvide.com/article/view/26627
- Tran DT, Badner NH, Nicolaou G, et al. Arterial pCO2 changes during thoracoscopic surgery with CO2 insufflation and one lung ventilation. HSR Proc Intensive Care Cardiovasc Anesth 2010;2:191-7. [PubMed]
- Sancheti MS, Dewan BP, Pickens A, et al. Thoracoscopy without lung isolation utilizing single lumen endotracheal tube intubation and carbon dioxide insufflation. Ann Thorac Surg 2013;96:439-44. [Crossref] [PubMed]
- Wong RY, Fung ST, Jawan B, et al. Use of a single lumen endotracheal tube and continuous CO2 insufflation in transthoracic endoscopic sympathectomy. Acta Anaesthesiol Sin 1995;33:21-6. [PubMed]
- Brock H, Rieger R, Gabriel C, et al. Haemodynamic changes during thoracoscopic surgery the effects of one-lung ventilation compared with carbon dioxide insufflation. Anaesthesia 2000;55:10-6. [Crossref] [PubMed]
- Ohtsuka T, Imanaka K, Endoh M, et al. Hemodynamic effects of carbon dioxide insufflation under single-lung ventilation during thoracoscopy. Ann Thorac Surg 1999;68:29-32. [Crossref] [PubMed]
- Polis I, Gasthuys F, Gielen I, et al. The effects of intrathoracic pressure during continuous two-lung ventilation for thoracoscopy on the cardiorespiratory parameters in sevoflurane anaesthetized dogs. J Vet Med A Physiol Pathol Clin Med 2002;49:113-20. [Crossref] [PubMed]
- Huang H, Ji H, Tian H. Risk factors for recurrence of primary spontaneous pneumothorax after thoracoscopic surgery. Biosci Trends 2015;9:193-7. [Crossref] [PubMed]
- Akter F, Routledge T, Toufektzian L, et al. In minor and major thoracic procedures is uniport superior to multiport video-assisted thoracoscopic surgery? Interact Cardiovasc Thorac Surg 2015;20:550-5. [Crossref] [PubMed]
- Young R, McElnay P, Leslie R, et al. Is uniport thoracoscopic surgery less painful than multiple port approaches? Interact Cardiovasc Thorac Surg 2015;20:409-14. [Crossref] [PubMed]
- Yang Y, Dong J, Huang Y. Single-incision versus conventional three-port video-assisted surgery in the treatment of pneumothorax: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 2016;23:722-8. [Crossref] [PubMed]


