Esophageal cancer patients’ information management: cross-cultural differences between Dutch and Italian patients in perceived quality of provided oncological information
Introduction
Esophageal cancer (EC) is the eight most common cancer worldwide with more than 450,000 new cases every year with the highest incidence in Asia and Africa (1,2). The prognosis remains generally poor, with a 5-year survival rate decreasing from 50% for localized tumors to 4% for metastatic disease (3). Surgical resection is the most valuable treatment but many advances have occurred during the last 20 years especially with neoadjuvant therapies (3). The best clinical approach to EC therefore is a multidisciplinary approach (involving surgeons, oncologists, radiotherapists, endoscopists and radiologists) in order to plan a patient tailored therapy (4). On the other hand, EC remains a relatively rare disease in the western world and, in Western Europe a family doctor will face no more than ten ECs in his/her career. Therefore, patients diagnosed with EC will encounter many physicians that will provide different levels of information about EC and its treatment options with an impact on expectations, illness perception and, in the end, quality of life that can vary from one patient to another even in similar circumstances (5).
Information perception about the disease and its prognosis is an important step of the patients’ active involvement in the curative path increasing the abilities to cope with the illness (6,7). Dein and colleagues showed evidence how cultural differences affect the illness perception (8) and many studies have investigated how cross-cultural differences can affect health related quality of life (HRQOL) (9,10). Most studies investigated perceived receipt of information in Northern Europe (5,11,12) whereas little is known about the situation in Southern Europe, but it is suspected that the approach can be very different. In fact, until recently, in Italy the doctor could conceal both diagnosis and prognosis to seriously ill patients out of beneficence (13) as part of a “paternalistic” model traditionally more common in Southern Europe (14). In this model bad news could be partially or totally hidden in order to protect the patient. On the other hand, the “autonomy” model prefers caregivers to be outright and clear providing complete information (13) and is more common in the United States and Northern Europe (15). This study was aimed to investigate how patients affected by EC can perceive the information provided by caregivers in two different European cultural context, one in the north (The Netherlands) and the other in the south (Italy) of Europe.
Material and methods
Study design
This is an observational prospective study aimed to investigate cultural differences in patients’ perception about provided information in patients with potentially curable EC in two tertiary referral centers in Italy and The Netherlands. This study was approved by the local Ethical Committees of the Veneto Institute of Oncology (IOV-IRCCS) in Padova, Italy (Reference Number: 2014/83) and the Academic Medical Center in Amsterdam, The Netherlands (Reference Number: W14_217 # 14.17.0263). All the Italian patients signed a written consent; the Institutional Review Board of the Academic Medical Center in Amsterdam granted a waiver of written consent for Dutch patients.
Statistics
The sample size was calculated setting a standardized effect size at 0.50 [clinically significant difference for the European Organization for Research and Treatment of Cancer (EORTC) questionnaire is conventionally set at 10 and the mean standard deviation (SD) is around 20], the possibility of type I error (alpha) at 0.05 and the possibility of type II error (beta) at 0.20. Consequently, the minimal sample size for each group was 63 patients but we incremented it of 10% to adjust for gender so the final minimal sample size was 69 patients for each group.
Patients
All the patients presenting with EC at the outpatient clinic of the Veneto Institute of Oncology and the Academic Medical Center from October 2014 to November 2015 were asked to fill in the questionnaires. Patients were enrolled if they had a diagnosis of EC with a tumor localized in the gastroesophageal junction (GE junction) or the distal esophagus (Siewert I or II). Exclusion criteria were: patients who were not able to fill in the questionnaire independently or who had more than one malignancy or a Siewert class III tumor.
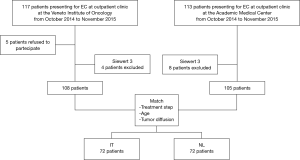
During the study period, 230 patients were asked to fill in the questionnaire: 113 of whom were Dutch and 117 were Italian. In this group, 12 patients had a Siewert III tumor (8 Dutch and 4 Italian) and were therefore excluded. Moreover, in the Italian group, 5 patients refused the enrollment. Patient matching was performed on the following criteria: treatment step (diagnosis vs. during neoadjuvant therapy), age, tumor diffusion (localized vs. metastatic) and the final sample size was 72 patients per group. The enrollment flow chart is shown in Figure 1.
Data collection
Patients were asked to participate in the study while waiting for the multidisciplinary visit at first consultation or while waiting for the medical/radiation oncologist during neoadjuvant therapy. The questionnaires were administered and filled in after the visit; moreover, a preformatted sheet was used to collect clinical and demographic records. Since patients were enrolled at their first or second visit in a tertiary referral center, some clinical information about disease stage or curability might be incomplete or incorrect. However, we still decided to use these data because this was the information available at the time of the visit and was reported to the patients by the clinicians: the answers given to the questionnaire reflected what the patient could perceive at the moment of questionnaire collection.
Questionnaires
The Italian and Dutch versions of the EORTC QLQ-INFO25 were used to evaluate the information received by EC patients. This 25-items questionnaire includes: four information provision subscales (about disease, medical tests, treatment and other care services), two items on perceived receipt of information about other areas (different places of care, things you can do to help yourself to get well), two items on the perceived receipt of hard copy information (written and electronic), two items on the wish to receive more or less information and two items on satisfaction and usefulness of the information disclosed (16). We chose not to consider the item about receipt of electronic information (i.e., CD/video) because is not usually provided at this moment of care in our context.
The Italian and Dutch versions of EORTC, QLQ-C30 were used to evaluate specific aspects of quality of life. The QLQ-C30 is a 30-items questionnaire for assessing the generic quality of life of cancer patients (17). The selected aspects of quality of life were C30 global quality of life and the five functioning scales. All scores are linearly transformed to a scale of 0 to 100 according to the guidelines of the EORTC. Data on patient’s characteristics and disease status were retrieved from local medical records.
Healthcare context
The Veneto Institute of Oncology and the Academic Medical Center are tertiary referral centers that get referrals for EC patients from all over Italy and The Netherlands, respectively. Most patients are directly referred by the medical oncologist or gastroenterologist of the referring hospitals or from the family doctor whereas a minority of patients are referred to the outpatient clinic for multidisciplinary oncological consultation about treatment by the endoscopist that made the diagnosis at the referral center. Every patient is discussed in a weekly multidisciplinary oncology meeting (including a dedicated upper GI surgeon, a medical oncologist, a radiation oncologist, a pathologist and a nuclear medicine radiologist) in which a definitive treatment plan is designed.
Statistical analysis
Continuous data were expressed as mean and SD or median and interquartile range (IQR). Patient’s characteristics were compared between the two centers using Fisher test (categorical data) and Mann-Whitney test (continuous data). Linear regression models were used to compare INFO25 and C30 scales between the two centers at different treatment steps, adjusting for gender. A P value less than 0.05 was considered statistically significant. Statistical analysis was performed using SAS 9.1 software (SAS Institute Inc., Cary, NC, USA).
Results
Participants
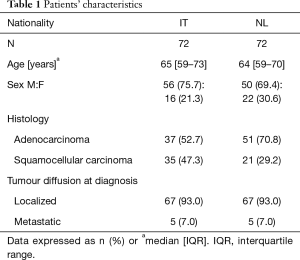
One hundred and forty-four patients presenting for EC at outpatient clinic at the Veneto Institute of Oncology in Italy (72 patients) and the Academic Medical Center in The Netherlands (72 patients) were included in the study. Forty-eight patients were included at diagnosis and 96 patients during neoadjuvant therapy. Most patients (94%) had a diagnosis of localized EC. Patients’ characteristics are shown in Table 1.
Full table
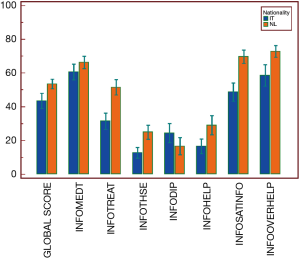
Patients’ perceived receipt of information
At diagnosis, Dutch patients reported better information than Italian patients about: treatments (51.6±25.9 vs. 31.5±25.9, P<0.001), other services (24.9±24.4 vs. 12.7±18.3, P=0.01), and things that patients can do to help themselves (29.2±32.5 vs. 16.6±24.3, P=0.02), when adjusted for gender. Moreover, Dutch patients reported higher satisfaction with information received (69.8±22.9 vs. 48.8±29.3, P<0.001) and with written information (96.9±17.4 vs. 43.3±50.4, P<0.001), and a better global score (53.5±15.4 vs. 43.5±22.6, P=0.03) than Italian patients, adjusting for gender (Figure 2).
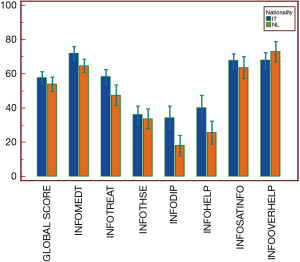
During neoadjuvant therapy, Italian patients were more satisfied than Dutch patients with information about disease (62.1±23.9 vs. 45.1±21.0, P=0.01) while Dutch patients were more satisfied with written information (78.3±42.1 vs. 43.3±50.4, P=0.01), adjusting for gender (Figure 3).
Association between perceived receipt of information and quality of life
At diagnosis, the global quality of life (QL2) of the Italian patients showed no correlation with any scale of the INFO25 questionnaire. On the contrary, in Dutch patient QL2 and emotional function scale (EF) significantly correlated with the perceived information about the disease (rho =0.547 vs. rho =0.360, respectively), medical tests (rho =0.372 vs. rho =0.405, respectively), treatments (rho =0.427 and rho =0.528, respectively) and other services (rho =0.553 and rho =0.472, respectively). Moreover, in Dutch patients, QL2 correlated with the global score of perceived information (rho =0.456). P values and details about association between perceived receipt of information and quality of life are shown in Table 2.
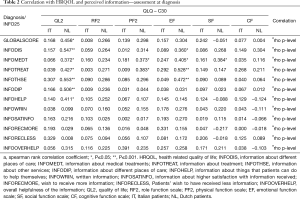
Full table
During neoadjuvant therapies, Italian patients reported a correlation between the INFO25 Global Score and QL2 (rho =0.483), role function scale (RF2) (rho =0.410), physical function scale (PF2) (rho =0.401) and EF (rho =0.568). The perceived information about medical treatments (INFOMEDT) of the Italian patients was correlated with their RF2 (rho = 0.382), PF2 (rho =0.425), EF (rho =0.392), SF (rho =0.420) and their perceived information about treatment (INFOTREAT) and other services (INFOTHSE) were correlated with PF2 (rho =0.347) and EF (rho =0.451) respectively. Details about association between perceived receipt of information and quality of life are shown in Table 3.
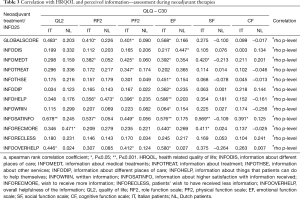
Full table
Discussion
In this study, we aimed to evaluate how cross-cultural differences among Northern and Southern Europe can affect the perception of the information provided by caregivers in EC patients. To our knowledge this is the first study investigating this field in patients affected by EC.
Our findings revealed that Dutch patients have a higher satisfaction at diagnosis with the information received and a better perception of the information about treatments, other services and in how they can help themselves. Moreover, they were more satisfied about the written support they received at diagnosis and during neoadjuvant treatment. Arraras et al. (18) reported that patients from Northern and Central Europe usually receive more written information than patients from Southern Europe. Therefore, this precise and accurate way of communication of cancer information is thus common and expected by Dutch patients that confirmed their satisfaction with written information.
On the other hand, the Italian patients revealed higher level of satisfaction with information about the disease only in a later time, during the neoadjuvant therapy. The INFO25 validation study (16) found that patients from South Europe usually prefer a more oral-based communication style. A study by Mauri et al., suggested a cross-cultural uniformity among Italian cancer patients who appreciate a direct physician-patient relationship with the possibility to ask questions and to be reassured (13). In fact, during the neoadjuvant treatment, patients have more opportunities to ask for more information that she/he did not ask or did not dare to ask at diagnosis. During their disease course, EC patients will encounter different specialists that can meet their needing in receiving more information about their disease; this could explain higher satisfaction with information about the disease reported by the Italian patients during neoadjuvant treatment.
Our results indicated that perceived information can affect EC patients’ HRQOL. In Dutch patients we observed a direct correlation at diagnosis between global quality of life and the global score of perceived information and, between emotional function with the perceived information about the disease, medical tests, treatments and other services. These findings are similar to those of Husson et al. (6) in patients affected by lymphoma who reported better HRQOL associated with higher level of information perceived at baseline (<6 months from diagnosis). Curiously enough, at diagnosis, Italian patients did not associate the satisfaction with provided information with their quality of life; this might be due to lower expectation about information of their disease (13). These data suggest that, at diagnosis, while Dutch patients in some way use the provided information to ameliorate their quality of life Italian patients do not. At diagnosis, an effective communication should aim to increase the capability to cope the new disease situation (19). Efforts to reach this aim should be attempted in the Italian setting.
On the contrary, during neoadjuvant therapy, QL2 correlated with the perceived information in the Italian group. In this group, INFO25 Global Score was correlated with global quality of life and emotional function. Since the definition of quality of life include “patient satisfaction with levels of functioning and control of the disease” (20), at this stage Italian patients probably feel that information help them to better control what is happening. In fact, improving the level of perceived information on the disease and on treatments could help to improve quality of life in a delicate moment such as during neoadjuvant therapy where the length of cure and its side effects might undermine patient’s emotional function.
The information providing by caregivers recognizes two models in use in Europe: the “autonomy” and the “paternalistic” model. The “autonomy” model (15), more in use in Northern Europe, accepts patients as collaborative partners in making major medical decisions and therefore prefers physicians to be clear, easy to perceive and providing a high level of both written and oral information. In Southern Europe it is more prevalent the “paternalistic” model (14,21) in which caregivers usually withhold, in whole or in part, the truth in order to obtain a beneficial effect on the patients, with the purpose to help them to live with less anxiety and preserving their hope. In our study, the higher level of perceived information with better quality of life in Dutch patients at diagnosis seem to fit well in the “autonomy” model, matching with good results the patients’ needing at the beginning of the treatment path. On the reverse, during neoadjuvant therapy Dutch patients tend to be more insecure than Italian in their perception of information provided. We found the opposite situation in the Italian group, according to the “paternalistic” model that reported lower level of perceived information at diagnosis. On the contrary, this level tends to grow and to correlate with HRQOL during neoadjuvant therapy. The autonomy model (more clear in communication) and the paternalistic model (more protective) (14) seem to be the two sides of the same coin: both cover the need in information during a step of the treatment, both leave empty spaces that sooner or later will require more information. A previous study investigated patients’ preferences for medical decision making to compare later the results with the physician's perception of these preferences and demonstrated that usually physicians were more likely to predict that patients would have preferred a less shared approach than they in fact did (6). Further investigation are required to plan a new approach in information providing that could better meet the patients’ needing at any phase of the therapeutic process.
The main limit of this study is the heterogeneity of the enrolled patients; due to this our regression models were adjusted for gender but a more homogeneous sample with a more even representation of gender could help in determining differences between males and females. A second limit is the low rate of patients presented with metastatic disease; the perceived information and the needing in receiving more information may vary between potentially curative and metastatic disease (22). Finally, this study was conducted in only one center per country. Even if both the centers involved in this study are among the largest referral centers of their respective nations and usually receive patients from all over the respective nation, the perception of information can vary from one hospital to another in the same country, especially if they are located in geographically distant areas.
Conclusions
In conclusion, the present study shows cross-cultural differences between Italian and Dutch patients in the perception of information at baseline and during neoadjuvant therapy, reflecting the autonomy model (more clear in communication) and the paternalistic model (more protective) used respectively in Northern and Southern Europe. The level of perceived information can affect quality of life of patients; tailoring communication and information providing can improve the way of patients’ coping with illness.
Acknowledgements
The study was supported by Current Research Fund from Italian Ministry of Health to Carlo Castoro and by a grant from Berlucchi Foundation (Brescia, Italy) to Carlo Castoro.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the local Ethical Committees of the Veneto Institute of Oncology (IOV-IRCCS) in Padova, Italy (Reference Number: 2014/83) and the Academic Medical Center in Amsterdam, The Netherlands (Reference Number: W14_217 # 14.17.0263). All the Italian patients signed a written consent; the Institutional Review Board of the Academic Medical Center in Amsterdam granted a waiver of written consent for Dutch patients.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2013. Bethesda, MD: National Cancer Institute, 2016. Available online: http://seer.cancer.gov/csr/1975_2013/
- Shapiro J, van Lanschot JJB, Hulshof MCCM, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol 2015;16:1090-8. [Crossref] [PubMed]
- Cools-Lartigue J, Spicer J, Ferri LE. Current status of management of malignant disease: current management of esophageal cancer. J Gastrointest Surg 2015;19:964-72. [Crossref] [PubMed]
- Jenkins V, Fallowfield L, Saul J. Information needs of patients with cancer: results from a large study in UK cancer centres. Br J Cancer 2001;84:48-51. [Crossref] [PubMed]
- Husson O, Oerlemans S, Mols F, et al. Satisfaction with information provision is associated with baseline but not with follow-up quality of life among lymphoma patients: Results from the PROFILES registry. Acta Oncol 2014;53:917-26. [Crossref] [PubMed]
- Faller H, Koch U, Brähler E, et al. Satisfaction with information and unmet information needs in men and women with cancer. J Cancer Surviv 2016;10:62-70. [Crossref] [PubMed]
- Dein S. Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncol 2004;5:119-24. [Crossref] [PubMed]
- Kaptein AA, Yamaoka K, Snoei L, et al. Illness perceptions and quality of life in Japanese and Dutch women with breast cancer. J Psychosoc Oncol 2013;31:83-102. [Crossref] [PubMed]
- van der Kloot WA, Uchida Y, Inoue K, et al. The effects of illness beliefs and chemotherapy impact on quality of life in Japanese and Dutch patients with breast or lung cancer. Chin Clin Oncol 2016;5:3. [PubMed]
- McNair AGK, MacKichan F, Donovan JL, et al. What surgeons tell patients and what patients want to know before major cancer surgery: a qualitative study. BMC Cancer 2016;16:258. [Crossref] [PubMed]
- Thrumurthy SG, Morris JJ, Mughal MM, et al. Discrete-choice preference comparison between patients and doctors for the surgical management of oesophagogastric cancer. Br J Surg 2011;98:1124-31; discussion 1132. [Crossref] [PubMed]
- Mauri E, Vegni E, Lozza E, et al. An exploratory study on the Italian patients' preferences regarding how they would like to be told about their cancer. Support Care Cancer 2009;17:1523-30. [Crossref] [PubMed]
- Costantini M, Morasso G, Montella M, et al. Diagnosis and prognosis disclosure among cancer patients. Results from an Italian mortality follow-back survey. Ann Oncol 2006;17:853-9. [Crossref] [PubMed]
- Whitney SN, McCullough LB. Physicians' silent decisions: because patient autonomy does not always come first. Am J Bioeth 2007;7:33-8. [Crossref] [PubMed]
- Arraras JI, Greimel E, Sezer O, et al. An international validation study of the EORTC QLQ-INFO25 questionnaire: an instrument to assess the information given to cancer patients. Eur J Cancer 2010;46:2726-38. [Crossref] [PubMed]
- Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365-76. [Crossref] [PubMed]
- Arraras JI, Greimel E, Chie WC, et al. Cross-cultural differences in information disclosure evaluated through the EORTC questionnaires. Psychooncology 2013;22:268-75. [PubMed]
- Bruera E, Sweeney C, Calder K, et al. Patient preferences versus physician perceptions of treatment decisions in cancer care. J Clin Oncol 2001;19:2883-5. [Crossref] [PubMed]
- Gotay CC, Korn EL, McCabe MS, et al. Quality-of-life assessment in cancer treatment protocols: research issues in protocol development. J Natl Cancer Inst 1992;84:575-9. [Crossref] [PubMed]
- Levenstein S, Li Z, Almer S, et al. Cross-cultural variation in disease-related concerns among patients with inflammatory bowel disease. Am J Gastroenterol 2001;96:1822-30. [Crossref] [PubMed]
- Pinto E, Cavallin F, Saadeh LM, et al. Potential curability and perception of received information in esophageal cancer patients. Support Care Cancer 2018;26:1807-14. [Crossref] [PubMed]


