Double-barreled bronchoplasty for a carcinoid tumor with a rare variation of displaced bronchus
Introduction
Bronchoplasty is a procedure that is often performed to preserve the lung parenchyma. We report the case of double-barreled bronchoplasty performed for a carcinoid tumor with a rare variation of displaced bronchus.
Case presentation
The patient was a 69-year-old woman who previously visited a clinic with a chief complaint of bloody sputum. Bronchoscopy performed at the clinic suggested the presence of a tumor in the left bronchus, and the patient was referred to our hospital. Chest computed tomography (CT) (Figure 1) revealed the presence of a 21-mm mass along the left main and lower lobe bronchi and the tumor was protruding into the branching point of the upper segmental bronchi (Figure 1A). There was partial atelectasis of the lower lobe. The lingular segmental bronchus below the upper segmental bronchus was displaced as it branched with the lower lobe bronchus (LLB), and the left pulmonary artery was located ventral to the left main bronchus (LMB) without passing over it. The left pulmonary vein had a single stem, and V1+2a had a peculiar variation in which it ascended along the dorsal side of the bronchus after branching from the lower pulmonary vein (Figure 1B).
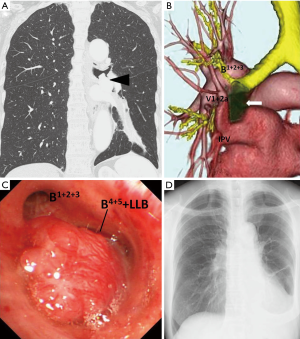
Bronchoscopy revealed the presence of a smooth and highly vascularized tumor in the LMB. Although the upper segmental bronchus could be identified, the lingular and lower lobe bronchi could not be identified (Figure 1C). However, the biopsy of the tumor was not performed at the previous clinic due to bleeding, the patient refused to undergo bronchoscopy at our hospital again. Therefore, we decided to perform lower lobectomy and bronchoplasty.
The surgery was performed through anterior axillary thoracotomy at the 4th intercostal space. The upper and lower lobes had poorly lobulated margins, whereas a distinct aberrant fissure was noted between the upper and lingular divisions. The V1+2a that ascended from the lower pulmonary vein was taped for preservation, and the lower pulmonary vein and A6–10 were stapled. The tissue surrounding the bronchi was dissected in order to identify the lingular segmental bronchus. A stiff tumor was identified along the LLB up to the branching point of the upper segmental bronchus. Therefore, the LMB was cut at the proximal of the tumor (Figure 2A), and the lingular and upper segmental bronchi were also cut. We resected left lower lobe and part of the LMB. A diagnosis of carcinoid tumor was made based on the pathological examination performed during the surgery. Tumor cells were not identified in the resected samples of the upper, lingular, and main bronchi. Since there were no metastases in the surrounding lymph nodes (stations 10–13), we proceeded to perform bronchoplasty. After the upper and lingular segmental bronchi were anastomosed by interrupted suture with 4-0 polydioxanone (Ethicon, Somerville, NJ), the LMB and upper-lingular segmental bronchi were anastomosed with a continuous suture with 4-0 polydioxanone (Figure 2B). The absence of any leakage was confirmed before ending the surgery. The tumor was 20 mm × 15 mm in size and was determined to be a typical carcinoid (TC). The postoperative course was favorable. X-ray and CT examinations performed 3 months after the surgery demonstrated that the upper and lingular segments were well-aerated (Figure 1D).

Discussion
Carcinoids comprise one of the neuroendocrine tumors (NET) of the lung and are rare, accounting for approximately 1% to 2% of all primary lung tumors (1). Carcinoids are categorized as typical or atypical, based on the presence of mitosis and necrosis. TC, which was identified in the present case, often occurs in a central location and is generally associated with a good prognostic outcome. When possible, bronchoplasty is performed for patients with central TCs without metastasis to the lymph nodes in order to preserve the lung parenchyma (2,3). In this scenario, pathological diagnosis should be performed during the surgery to confirm that the resected tissues from the central and peripheral locations are negative for tumor cells.
The patient in this case had displaced bronchi; in particular, the upper segmental bronchus alone branched from the LMB, and the lingular segmental and LLB branched below. Displacement of the bronchus in the lingular segment of the left lung, such as seen in this case, is quite rare and has been reported by only a few case reports. The tumor was seen to arise from the LLB, protruded to the branching of the upper segmental bronchus, and almost blocked the opening of the lingular segmental bronchus. Therefore, we performed double-barreled bronchoplasty by continuous suturing of the upper and lingular segmental bronchi to the main bronchus, using 4-0 polydioxanone (Ethicon, Somerville, NJ). Recent studies demonstrated the effectiveness of endoscopic continuous suturing of the bronchus (4). At our institution, we typically chose to perform continuous suturing during bronchoplasty procedures, as reported previously (5). As demonstrated in the present case, continuous suturing was safe, effective, and can be performed easily and rapidly without tangling of the suture.
Conclusions
Continuous suturing with absorbable suture was a safe and effective surgical technique during double-barreled bronchoplasty for a carcinoid tumor with a very rare complication of a displaced bronchus.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- McMullan DM, Wood DE. Pulmonary carcinoid tumors. Semin Thorac Cardiovasc Surg 2003;15:289-300. [Crossref] [PubMed]
- Drożdż K, Chabowski M, Chachaj A, et al. Two cases of the bronchial carcinoid tumors successfully treated with the parenchymal-sparing bronchoplastic resections. J Thorac Dis 2017;9:E669-73. [Crossref] [PubMed]
- Terzi A, Lonardoni A, Feil B, et al. Bronchoplastic procedures for central carcinoid tumors: clinical experience. Eur J Cardiothorac Surg 2004;26:1196-9. [Crossref] [PubMed]
- Ohata K, Zhang J, Ito S, et al. Thoracoscopic bronchoplasty using continuous sutures in complete monitor view. Ann Thorac Surg 2014;98:1132-3. [Crossref] [PubMed]
- Matsuura N, Yokota N, Go T, et al. Bronchoplastic operation using a continuous anastomosis for mucous gland adenoma. Ann Thorac Surg 2011;92:2272-4. [Crossref] [PubMed]


