The role of initial radiologic and clinical manifestations in predicting the prognosis for pneumonia caused by H1N1 influenza virus
Introduction
The novel swine-origin influenza (H1N1) virus (S-OIV) generally known as the “swine flu” was first identified in Mexico in April 2009 (1). In 11 January 2009, the World Health Organization (WHO) announced the novel influenza virus (H1N1) global pandemic documented in more than 70 countries. The first series of patients were diagnosed in North America and the disease rapidly spread towards a pandemic (1-3). Similar to the seasonal influenza virus, the virus is spread through hand contact, respiratory tract and aerosol-generating procedures (4). The spectrum of the pandemic influenza A (H1N1) virus infection ranges between non-febrile mild upper respiratory tract disease to severe and even fatal pneumonia. Generally, the condition is often characterized by benign, self-limiting respiratory symptoms; the disease is similar to the other frequently observed viral infections of the respiratory tract and seasonal influenza that does not cause a more serious disease (5-8).
The aim of the present study is to evaluate the radiological and clinical findings of the patients with H1N1 during the novel swine-origin influenza A (H1N1) virus (S-OIV) pandemic. The radiologic aspects and variable co-existing clinical conditions were quested in terms of being indicators for increased morbidity.
Material and methods
Patients who presented with flu symptoms to our institution in the city of Van in the Eastern Anatolian region of Turkey between September-December 2009 and had to be hospitalized were retrospectively evaluated. Patients who were treated on an outpatient basis and those who did not undergo diagnostic tests for H1N1 although they presented with mild flu symptoms were excluded from the study. Thirty-nine patients with the diagnosis of H1N1 infection confirmed by fluorescent antigen-antibody testing and polymerase chain reaction (PCR) tests were included in the study. Radiography and thoracic computed tomography (CT) examinations were performed; the demographic characteristics, symptoms, laboratory findings and radiological features of all the patients were evaluated. This study was approved by the Institutional Ethics Committee, and informed consents were obtained from all patients.
The CT imaging was carried out using a two cross-sectional CT (SOMATOM Spirit Siemens, Erlangen, Germany) device and at a cross-sectional thickness of 10 mm, at a 130 kV dose and between 50-130 mAs. The images were assessed on the workstation, using the Nova PACS viewer program and a 2.560×2.048 pixel monitor. The CT images’ interpretations of all cases were performed by a single radiologist with at least 5 years of thoracic imaging experience.
The hospitalized patients were divided in two groups as those who needed intensive care unit (ICU) administration and those who were required brief hospitalization without advanced mechanical ventilation; ICU management was decided to be necessary for patients defined as the existence of either one of two major, or two of three minor criteria. While the major criteria include need for mechanical ventilation and shock requiring vasopressors; the minor criteria were respiratory rate > or =30 min–1, PaO2-to-FiO2 ratio < or =250, multilobar infiltrates, confusion or delirium, blood urea nitrogen (BUN) > or =20 mg/dL, leukopenia (WBC count <4,000 cells/mm3), thrombocytopenia (platelet count <100,000 cells/mm3), hypothermia (core temperature <36 °C), hypotension requiring aggressive fluid resuscitation criteria for ICU administration were stated to be the requirement of the invasive or non-invasive mechanical ventilation support. In both groups, the radiological features of pulmonary involvement such as extent (>3 lobes or less); location (peripheral or central); and pattern (ground glass opacity-GGO, consolidation, peribronchial thickening, or embolism) were respectively assessed as prognostic index. The pre-existing medical conditions such as obesity, chronic obstructive pulmonary disease (COPD), coronary artery disease and malignancies with or without immunocompromised conditions; moreover the patients’ age were considered respectively as if they have significance affect to the prognostic process. The follow-up results of the patients, particularly of the ICU administered cases, were evaluated.
The statistical analysis was performed with the help of the SSPS statistical software (v.16) and independent samples t-test and Pearson’s Chi-square test were employed. The logistic regression test was used to provide multivariable analysis of the co-existing risk factors and their combinations in terms of significance for the prognostic process. Statistical significance was based on a P value below 0.05.
Results
The mean age was calculated as 53.9±14 years (range, 19-99 years) among the patients, 21 (53.8%) were male and 18 (46.2%) were female. The mean age of the patients who were admitted to ICU was 58.3±14, while the mean age of those followed up on the ward was 52.7±20 years.
When the patients were classified according to their body mass index (BMI), 35 patients (89.7%) were found to be obese (BMI of 30 or greater, 2 were morbidly obese). The independent distribution of risk factors among patients was; coronary artery disease was present in seven patients (17.9%, three patients were with previous coronary by-pass surgery), COPD was present in 8 patients (20.5%), and malignancy was present in three patients (7.7%, two patients had esophageal and gastric cancer respectively; one patient had lymphoma). In terms of the combinations of risk factors that were co-existed with H1N1 pneumonia; the distribution among included patients was summarized in Table 1.
Full table
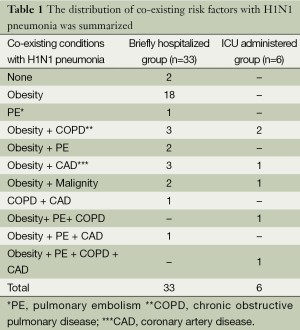
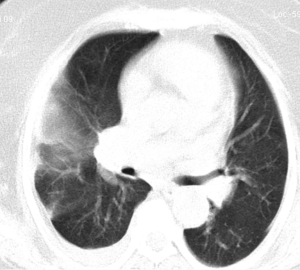
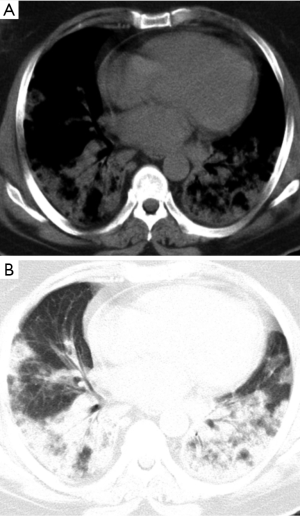
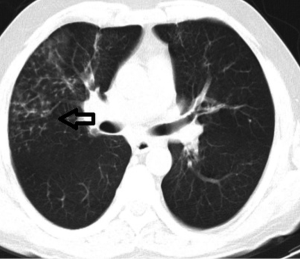
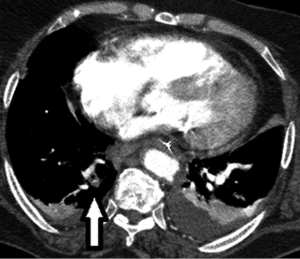
Thoracic CT examinations revealed that; unilateral pulmonary involvement was observed in 6 patients (15%), while bilateral pulmonary involvement was detected in 33 patients (85%). Only peripheral pulmonary involvement was observed in 14 patients (35.9%), while only central pulmonary involvement was observed in 2 patients (5.1%), and the combination of central and peripheral pulmonary involvement was observed in 23 patients (59%). The involvement according to the lobes was as follows: upper right pulmonary lobe, 20 (51.3%); middle right pulmonary lobe, 29 (74.4%); lower right pulmonary lobe, 28 (71.8%); upper left pulmonary lobe, 19 (48.7%); lingula of the left lung, 24 (61.5%); and lower left pulmonary lobe, 26 (66.7%). The numeric distribution of the pulmonary patterns was as follows: ground glass in 38 patients (97.4%) (Figure 1); consolidation in 24 patients (61.5%) (Figure 2), peribronchial thickening in 33 patients (84.6%), tree-in-bud sign in 18 patients (46.2%) (Figure 3), nodule in 18 patients (46.2%), pleural fluid in 3 patients (7.7%) (Figure 4), mediastinal lymphadenopathy in 12 patients (30.8%), atelectasis in 21 patients (53.8%), and pulmonary embolism in 6 patients (15.4%). Embolic occlusions were limited to sub-segmental range (Figure 4).
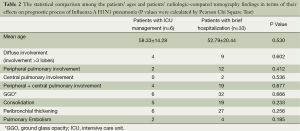
Six patients were admitted to ICU and thirty-three patients who did not require mechanical ventilation were followed up on the ward. The statistical assessment revealed a significant relationship between the co-existence of solely COPD (P=0.008, Odds ratio: 27) or COPD by malignity (Odds ratio: 13) and increased morbidity rate in the patients with H1N1 pneumonia; besides, no statistically significant correlation was observed between the incidence of necessity of ICU administration and the other investigated parameters including patients’ ages, the radiologic features of pulmonary involvement such as extent, location or patterns. The summary of statistical assessment among prearranged patient groups according to CT manifestations was demonstrated in Table 2. The co-existing situations such as obesity, coronary artery disease and pulmonary embolism were also considered. Even the combinations of the co-existing factors among patients were included in statistical analysis; no significance by them was revealed that can affect the prognostic process. In the follow-up period; while thirty-three briefly hospitalized patients were discharged within the consequent 24 hours, six patients who were administered in ICU had a mean ICU-stay-length of 12.67 days ±5.32 (range, 7-21 days) and were discharged without any permanent sequelae. No mortality was occurred.
Full table
Discussion
The well described etiologic factor of seasonal influenza that occurs as acute respiratory disease mostly in winter season is an RNA virus from the orthomyxovirus family termed as the “influenza”. In humans, the disease is frequently caused by the type A and type B viruses (9). Novel H1N1 influenza viruses are found in North America and Eurasia (1,10). In some cases, the infection in the upper respiratory tract may rapidly progress towards a fatal pulmonary disease. Hospitalization and even mechanical ventilation may be essential in these patients. Thoracic CT plays an important role in characterising the lesions and establishing the extent of the involvement, predicting the prognosis, planning the treatment and following the patient up (11). In the patients when the PCR is negative as the laboratory marker; radiological findings can influence the definite diagnosis and avoid any delays in the treatment protocol (9). According to our experiences, it could not be possible for each patient with suspected symptoms to confirm the H1N1 infection by developed laboratory tests; especially in hospitals located at cities with low socio-economic status. The increased patient number during pandemic periods could be another explanation of this unfortunate situation. Therefore, the predomination about the knowledge of the radiologic findings of the disease has an important role for practical diagnosis to maintain the appropriate medical approach promptly.
In a previous study conducted for this purpose in Mexico, the clinical and epidemiologic characteristics of 18 hospitalized patients due to the diagnosis of S-OIV were described (1). In this study, it has been claimed that the S-OIV infection may lead to severe medical conditions (12 of the 18 patients needed mechanical ventilation) and even death (7 of 18 patients). Also, in contrast to seasonal influenza, the swine flu affected young and middle-aged patients (between 13 and 47 years; 90% of cases were <52 years). The mean age of our cases was 53.9±14, which is higher than such previous study. The mean age of the patients with the requirement of ICU administration was 58.3 years in our study. This evidence may be related to the 76 excluded patients who were treated on outpatient basis without further hospitalization. Among the hospitalized patients who needed ICU administration, only one patient was 32 years old.
In a study reported by Li et al. that was conducted on 106 patients (11), the median age was found as 31.7±15.7. The characteristic imaging findings were ground glass opacities (74.5%), consolidations (72.6%), nodular opacities (3.7%), and the reticular opacities (1.6%). These findings had shown similarity with previously reported study by Agarwal et al. (12). In our study, there were 38 cases (97.4%) of ground glass, 24 cases (61.5%) of consolidation, 18 cases (46.2%) of nodules, 33 cases of (84.6%) peribronchial thickening, and 18 cases (46.2%) with the tree-in-bud sign. We observed that, the percentage of nodules and tree-in-bud sign were higher. Again, Li et al. declared higher percentages of diffuse pulmonary involvement in patients requiring advanced mechanical ventilation (63.3%), when compared with patients lack serious conditions of the disease (19.3%). Our study was also resulted with similar ratios; diffuse pulmonary involvement rates were 66.6% and 43.4% among ICU administered patients and non-ICU patients; respectively. However, the incidences of central, peripheral or both central and peripheral pulmonary involvements among two groups of our study (were 33% and 39%, 0% and 2%, 66% and 57% of 6 critically ill and 33 briefly hospitalized patients; respectively) had shown disparities when compared with the report by Li et al. (central involvements were in 63% and 4%, peripheral involvements were in 100% and 8%, and both central and subpleural involvement were in 86% and 29% among 30 critically ill and 76 briefly hospitalized patients; respectively).
From the aspect of the involvement of the lobes by H1N1 influenza pneumonia, the previous study by Li et al. had pointed the upper zone in 45%, middle zone in 83% and the lower zone in 96% of patients (11). In our study, involvement in the upper lobes was observed in 51% (upper right lobe: 51%, upper left lobe: 48.7%), involvement in the middle lobes was 81.2% (middle right: 74.4%, left lingula: 71.8%), and involvement in the lower lobes was 89.7% (lower right: 71%, lower left: 66.7%). Consequently, the involvement in the middle and lower lobes were stated with higher incidences in both studies.
Federal advisory committee on Immunization Practices (ACIP) of the United States’ Centers for Disease Control and Prevention (CDC) announced the obese and pregnant patients as the emergency risk groups for severe H1N1 infection (13). Another study including ten patients with novel influenza A (H1N1) virus infection and ARDS was pointed out the increased rates for severe complications, particularly in extremely obese patients (14). Although there was a higher prevalence of obesity in hospitalized patients, no statistically significant difference was observed by our study regarding the poor prognosis due to obesity. The number of hospitalized patients due to H1N1 infection was 39 in our study and interestingly; 35 of them were obese (2 were morbid obese) which can deduce that; in obese patients, H1N1 infection has a higher prevalence for the requirement of hospitalization but no statistical difference between the ratios for brief hospitalization and most advance therapies such as ICU administration and mechanical ventilation was determined.
Pulmonary embolism (PE) has not been reported to be a frequently observed complication of influenza infection (14,15). Among the patients clinically under the suspicion of PE, van Wissen et al. have found lower rates of PE evidences (1%) in the patients with influenza A infection (16), Thus, the authors have concluded that the influenza infection was not associated with an increased risk of acute pulmonary embolism. In the study originated from Mexico where the S-OIV (H1N1) was verified in the laboratory, similar result as no higher incidence of PE in H1N1 infected patients was reported (1). In our study, embolisms within segmental branches of pulmonary artery were observed in 6 patients (5.6%). Ohrui et al. reported of similar findings that were concluded as pulmonary micro-thromboembolism in two cases (17); thus knowing such particular complication is important for the radiologists to diagnose the pulmonary micro-embolic events when investigating the contrast enhanced thoracic CT images.
In our study, coexisting of H1N1 influenza pneumonia with COPD had an unfavourable prognosis; 4 of 6 patients (66.6%) with the necessity of ICU administration were also suffering from COPD while only 4 of 33 briefly hospitalized patients (12.1%) were with COPD and influenza infection coexistence and the statistical difference between groups was significant (P=0.008). According to our knowledge, this correlation of unfavourable prognostic process of H1N1 influenza pneumonia with accompanying COPD (Odds ratio: 27) or COPD and malignity (Odds ratio: 13) has not previously been reported; and should be confirmed by further studies. We also investigated the prognostic role of coronary artery disease coexistence with H1N1 influenza infection but no relation was determined.
There are a few studies investigated the prognosis of H1N1 infection in patients, especially in children, with co-existing malignant circumstances. Tran et al. reported the common interruption of cancer treatment by pH1N1 infection among children with cancer and stem cell transplant recipients (18) and Shah et al. declared that the prevention of severe complications of influenza virus can be possible by initiation of antiviral therapy promptly in children with cancer (19). Increased morbidity and mortality in immunocompromised patients with solid tumors was documented by Chemaly et al. and immediate antiviral therapy was also suggested to decrease the complication rates (20). Moderate or severe parenchymal involvement mostly without association of bronchiolitis was reported as an indicator of severe viral infection in neutropenic cancer patients (21). In our study; three patients with pre-diagnosed malignancy including the esophageal and gastric cancer in two cases and lymphoma in one case had shown no statistically significant difference when compared with the other patients in terms of prognosis. Only 32-year-old male with co-exiting lymphoma had to be managed in ICU. The explanation of this dilemma when compared with previous studies could be; two patients with esophageal and gastric cancers were in their remission period when referred with influenza infection and no abnormalities in complete blood count including the rough immunity parameters were noticed; besides, slight immunocompromised situation was present in case with lymphoma. However; in our study, the malign situations when combined with COPD had shown statistically significant effect on impoverishing the prognostic process (with an odds ratio of 13). Because of previous studies were mostly included the pediatric population; projected future studies including higher number of H1N1 infected adult patients with coexisting malignancies are necessary to clarify the effects of immunocompromised situations to the prognosis of entity.
The observed radiological findings such as ground glass opacity, consolidation, nodular lesions, tree-in-bud sign, and peribronchial distribution were considered to be non-specific to influenza pneumonia. The radiological differential diagnosis must be based on cryptogenic organizing pneumonia (COP) and chronic eosinophilic pneumonia (CEP) or other viral, fungal and bacterial infections. The radiologic imaging results may be contributory to the laboratory tests especially in cases with reminiscent clinical symptoms and anamnesis of doubtful contamination (22). Additionally, the sudden onset of the H1N1 infection symptoms should be respected as an important factor when distinguishing from other diseases. However, unusual imaging findings such as pleural effusion, lymphadenopathy and lobar consolidation besides the clinical and laboratory results may help in eliciting the accurate diagnosis (23). The patterns and distribution of the ground glass opacity, consolidations and peribronchovascular or subpleural involvements were found to be highly correlated with H1N1 infection by Aviram et al. (24); but we revealed that none of these radiologic features can be considered in estimating the prognosis.
Our study had certain limitations such as the total patient number was limited. We also did not verify S-OIV among the patients who were treated in an outpatient setting. Since we excluded these patients from the study, the demographic and radiological statistics of the patients could be affected by selection bias. No additional comparison of the severity of the disease among ICU administered patients was performed that can be provided by evident predictive scoring systems such as Acute Physiology, Age and Chronic Health Evaluation (I-IV) (APACHI) or Sequential Organ Failure Assessment (SOFA).
Conclusions
Radiologic manifestations and clinical parameters such as age, obesity, co-existence of coronary artery disease or malignancy (with normal immunological parameters in general) does not affect the prognosis of patients with H1N1 influenza pneumonia; besides, the clinicians should be on the alert of unfavourable and rapid progression when considering patients of H1N1 infection with co-existence of solely COPD or COPD by malignity.
Acknowledgements
Funding: This work was not supported by and funds nor grand.
Disclosure: The authors declare no conflict of interest.
References
- Perez-Padilla R, de la Rosa-Zamboni D, Ponce de Leon S, et al. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med 2009;361:680-9. [PubMed]
- Domínguez-Cherit G, Lapinsky SE, Macias AE, et al. Critically Ill patients with 2009 influenza A(H1N1) in Mexico. JAMA 2009;302:1880-7. [PubMed]
- Echevarría-Zuno S, Mejía-Aranguré JM, Mar-Obeso AJ, et al. Infection and death from influenza A H1N1 virus in Mexico: a retrospective analysis. Lancet 2009;374:2072-9. [PubMed]
- Writing Committee of the WHO Consultation on Clinical Aspects of Pandemic (H1N1) 2009 Influenza, Bautista E, Chotpitayasunondh T, et al. Clinical aspects of pandemic 2009 influenza A (H1N1) virus infection. N Engl J Med 2010;362:1708-19. [PubMed]
- Plessa E, Diakakis P, Gardelis J, et al. Clinical features, risk factors, and complications among pediatric patients with pandemic influenza A (H1N1). Clin Pediatr (Phila) 2010;49:777-81. [PubMed]
- Komiya N, Gu Y, Kamiya H, et al. Clinical features of cases of influenza A (H1N1)v in Osaka prefecture, Japan, May 2009. Euro Surveill 2009;14:19272. [PubMed]
- Park SI, Kim MJ, Hwang HY, et al. Clinical characteristics of children with 2009 pandemic influenza A (H1N1) admitted in a single institution. Korean J Pediatr 2010;53:886-91. [PubMed]
- Ong AK, Chen MI, Lin L, et al. Improving the clinical diagnosis of influenza--a comparative analysis of new influenza A (H1N1) cases. PLoS One 2009;4:e8453. [PubMed]
- García-García J, Ramos C. Influenza, an existing public health problem. Salud Publica Mex 2006;48:244-67. [PubMed]
- Novel Swine-Origin Influenza A. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med 2009;360:2605-15. [PubMed]
- Li P, Su DJ, Zhang JF, et al. Pneumonia in novel swine-origin influenza A (H1N1) virus infection: high-resolution CT findings. Eur J Radiol 2011;80:e146-52. [PubMed]
- Agarwal PP, Cinti S, Kazerooni EA. Chest radiographic and CT findings in novel swine-origin influenza A (H1N1) virus (S-OIV) infection. AJR Am J Roentgenol 2009;193:1488-93. [PubMed]
- To KK, Wong SS, Li IW, et al. Concurrent comparison of epidemiology, clinical presentation and outcome between adult patients suffering from the pandemic influenza A (H1N1) 2009 virus and the seasonal influenza A virus infection. Postgrad Med J 2010;86:515-21. [PubMed]
- Centers for Disease Control and Prevention (CDC). Intensive-care patients with severe novel influenza A (H1N1) virus infection - Michigan, June 2009. MMWR Morb Mortal Wkly Rep 2009;58:749-52. [PubMed]
- Schultz MJ, Haitsma JJ, Zhang H, et al. Pulmonary coagulopathy as a new target in therapeutic studies of acute lung injury or pneumonia--a review. Crit Care Med 2006;34:871-7. [PubMed]
- van Wissen M, Keller TT, Ronkes B, et al. Influenza infection and risk of acute pulmonary embolism. Thromb J 2007;5:16. [PubMed]
- Ohrui T, Takahashi H, Ebihara S, et al. Influenza A virus infection and pulmonary microthromboembolism. Tohoku J Exp Med 2000;192:81-6. [PubMed]
- Tran D, Science M, Dix D, Portwine C, et al. Pandemic (H1N1) 2009 influenza in Canadian pediatric cancer and hematopoietic stem cell transplant patients. Influenza Other Respir Viruses 2012;6:e105-13. [PubMed]
- Shah DP, El Taoum KK, Shah JN, et al. Characteristics and outcomes of pandemic 2009/H1N1 versus seasonal influenza in children with cancer. Pediatr Infect Dis J 2012;31:373-8. [PubMed]
- Chemaly RF, Vigil KJ, Saad M, et al. A multicenter study of pandemic influenza A (H1N1) infection in patients with solid tumors in 3 countries: early therapy improves outcomes. Cancer 2012;118:4627-33. [PubMed]
- Rodrigues RS, Marchiori E, Bozza FA, et al. Chest computed tomography findings in severe influenza pneumonia occurring in neutropenic cancer patients. Clinics (Sao Paulo) 2012;67:313-8. [PubMed]
- Punpanich W, Chotpitayasunondh T. A review on the clinical spectrum and natural history of human influenza. Int J Infect Dis 2012;16:e714-23. [PubMed]
- Guo HH, Sweeney RT, Regula D, et al. Best cases from the AFIP: fatal 2009 influenza A (H1N1) infection, complicated by acute respiratory distress syndrome and pulmonary interstitial emphysema. Radiographics 2010;30:327-33. [PubMed]
- Aviram G, Bar-Shai A, Sosna J, et al. H1N1 influenza: initial chest radiographic findings in helping predict patient outcome. Radiology 2010;255:252-9. [PubMed]


