Extent of lymph node dissection: common hepatic artery lymph node dissection can be omitted for esophageal squamous cell carcinoma
Introduction
The outcomes for patients with esophageal cancer (EC) remain suboptimal and the incidence of EC has been increasing in recent years. To improve the outcomes of EC, multidisciplinary treatment has been developed and the survival rates have been improving, however, they are still far from satisfactory (1,2). One reason is its high frequency of lymph node (LN) metastasis. In addition, lymphatic metastasis of EC does not follow a standard pattern (3,4). The latest version of the UICC/AJCC TNM classification (7th edition) emphasizes the importance of LN metastasis for prognosis. However, the Japanese Classification of EC (10th edition) has not incorporated the number of LN metastases into the N factor for its staging system (5,6). Given its frequency and extent of LN metastasis, controlling LN metastasis is a rational therapeutic strategy, and an extended LN dissection may be logical in selected patients. But recent arguments have supported a reduction of unnecessary LN dissection in esophagectomy, which may be associated with increased operative time and postoperative complication (7). Here, we aimed to evaluate the effectiveness of common hepatic artery LN dissection in surgery for thoracic esophageal squamous cell carcinoma.
Methods
Patients
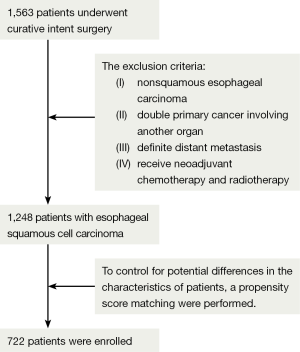
Between 2005 and 2012, 1,563 patients underwent curative intent surgery for EC at the Fudan University Shanghai Cancer Center. The records of all patients with esophageal squamous cell carcinoma were reviewed for the present study. Of these patients, 1,248 patients with esophageal squamous cell carcinoma were enrolled in this study, 682 patients were underwent esophagectomy with common hepatic artery LN dissection and 566 patients were underwent esophagectomy without common hepatic artery LN dissection. The exclusion criteria were as follows: (I) nonsquamous esophageal carcinoma; (II) double primary cancer involving another organ; (III) definite distant metastasis; and (IV) receive neoadjuvant chemotherapy and radiotherapy. All patients were staged according to the TNM classification of the 7th edition of the American Joint Committee for cancer staging manuals (8). The institutional review board of Fudan University Shanghai Cancer Center approved the database of esophageal carcinoma used for the present study.
Preoperative evaluation
Preoperative evaluation at Fudan Universtiy Cancer Center included chest and abdomen computed tomography (CT), barium esophagography, electronic gastroscopy, cervical and abdomen ultrasound, and endoscopic ultrasound (EUS). Through preoperative evaluation, patients with tumors that were confined to the mucosa without nodal metastasis were referred to the endoscopic intervention department for endoscopic mucosal resection (EMR). However, for tumors that were invading the submucosa or for which adequate resection margins were not achieved, EMR was performed at our institution. If a patient had already undergone endoscopy at another hospital, pathology consultation was performed at our insititution. If adequate resection margins were not achieved at another hospital, endoscopy was performed a second time. Integrated positron emission tomography and CT (PET-CT) has not been routinely performed to evaluate nodal metastasis and distant extrathoracic metastasis because of the high price that people cannot afford it. On the basis of the results from those examinations, the patients who were medically suitable, with stage T1-T3 tumors without distant metastases would undergo Surgery.
Surgical approach and lymphadenectomy
Patients was either Ivor Lewis, transhiatal esophagectomy or tri-incisional esophagectomy according to their bodies situation and tumor location, however, the choice of surgical approach also depend on surgeon preference. Middle and lower mediastinal nodes and upper abdominal nodes were routinely removed through a left thoracotomy, however, through a right thoracotomy (Ivor-Lewis procedures), usually the total mediastinal lymphadenectomy was performed. And cervical lymphadenectomy was performed through cervical incision when lymphatic involvement in the neck was indicated by CT scan or ultrasonography.
In our present study, the cervical LNs included the LNs in the supraclavicular and cervical paraesophageal regions. The upper mediastinal nodes included the upper paraesophageal LNs and recurrent laryngeal nerve LNs. The middle mediastinal nodes included the subcarinal, middle paraesophageal, and bilateral hilar LNs. The lower mediastinal nodes included the lower paraesophageal, and diaphragmatic LNs. The upper abdominal nodes included the paracardial LNs, lesser curvature LNs, left gastric artery LNs, common hepatic artery LNs, splenic artery LNs, and celiac artery LNs.
Statistical analysis
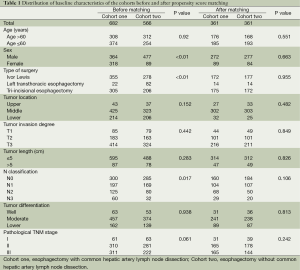
Descriptive statistics were used to compare variables between the unmatched groups, using the χ2 test for categorical variables. Logistic regression analysis was conducted to evaluate the effects of clinical factors. To control for potential differences in the characteristics of patients treated with common hepatic artery LN dissection or without common hepatic artery LN dissection, propensity score methods were used. By using logistic regression model, which included variables such as age, sex, type of surgery, tumor location, tumor invasion degree, tumor length, pathological N stage, tumor differentiation and pathological TNM stage, propensity scores were computed as the conditional probability of receiving either esophagectomy with common hepatic artery LN dissection or esophagectomy without common hepatic artery LN dissection. Using the nearest neighbor match algorithm, we created propensity score-matched pairs without replacement (a 1:1 match). And the caliper definition was set 0.02. The paired patients were extracted from the database. Using this method, 361 of 682 patients who underwent esophagectomy with common hepatic artery LN dissection were matched with 361 of 566 patients who underwent esophagectomy without common hepatic artery LN dissection with similar propensity scores (Table 1). A P value of <0.05 was considered statistically significant. All statistical analyses were performed with SPSS package (version 19.0).
Full table
Results
Patients characteristics
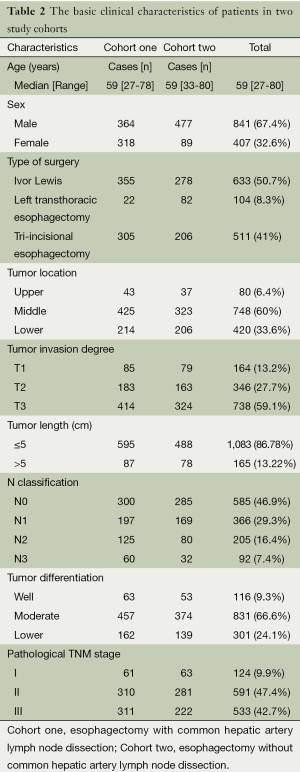
A total of 1,563 EC patients who underwent esophagectomy were enrolled onto the research at the Fudan University Cancer Center from May 2005 to December 2012. The results of the procedure are summarized in Figure 1. The enrolled study patients were divided into two cohorts: patients (n=682) who underwent esophagectomy with common hepatic artery LN dissection and patients (n=566) who underwent esophagectomy without common hepatic artery LN dissection. In the first cohort, 364 patients (53.37%) were male and 318 female (46.63%); in the second cohort, 477 patients (84.27%) were male and 89 female (15.73%), all the patients were stage I to III. The baseline characteristics of 1,563 patients are summarized in Table 2. Matching based on propensity scores produced 361 patients in each cohort, and the paired cohorts were well balanced (Table 1).
Full table
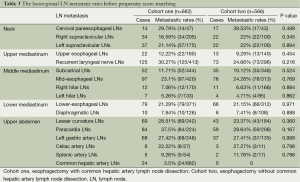
Lymph node metastasis (LNMs) before propensity score-matching
A total of 18,277 LNs were dissected (27 LNs per patient), the LN metastatic rate was 55.87%. Of all the LNMs, the paracardial LNs were the most frequently involved (37.5%), followed by recurrent laryngeal nerve LNs (30.27%) in cohort one. Whatever, only 24 patients had common hepatic artery LN metastasis, with the metastatic rate of 3.5% in cohort one (Table 3). Compared with other LNMs, the metastatic rate of common hepatic artery LN is the lowest. In addition, all the common hepatic artery LN metastasis was accompanied with locoregional metastasis.
Full table
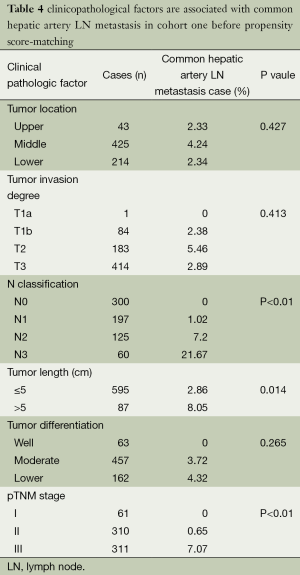
Risk factors for common hepatic LNMs
In our study, the relationship between metastatic rates of common hepatic artery LN and clinicopathological factors were also analyzed (Table 4). Logistic regression analysis identified that tumor length (P=0.014), N classification (P<0.01) and pathological TNM stage (P<0.01) correlated with the occurrence of common hepatic artery LNMs. The common hepatic artery LN metastatic rates of patients with diameter of tumor under or equal 5 cm and 5 cm were 2.86% and 8.05%, with significant difference (P=0.014). The common hepatic artery LN metastatic rates of patients in N0, N1, N2 and N3 stage were 0%, 1.02%, 7.2% and 21.67%, with significant difference (P<0.01). The common hepatic artery LN metastatic rates of patients with stage I, II, III were 0%, 0.65% and 7.07%, significant difference was found (P<0.01).
Full table
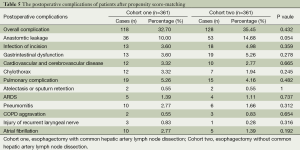
Postoperative complications after propensity score-matching
After propensity score-matching, the postoperative complications were analyzed in Table 5. The percentage of overall complications were 118 patients (32.70%) in cohort one and 128 patients (35.45%) in cohort two (Table 5): including anastomotic leakage, infection of incison, gastrointestinal dysfunction, cardiovascular and cerebrovascular disease, chylothorax, pulmonary complication, injury of recurrent laryngeal nerve and atrial fibrillation, no significant difference was found (P=0.432). The overall incidence of anastomotic leakage in the cohort one was lower than that in the cohort two, although this difference was not statistically significant (P=0.054).
Full table
Discussion
In EC, the overall 5-year survival rate after surgical resection is between 70% and 92% for patients without nodal involvement, but only 18-47% for patients with LN metastasis (9-11). However, aggressive radical LN dissection may increase postoperative morbidity and mortality. The latest version of the UICC/AJCC TNM classification (7th edition) emphasizes the importance of LN metastasis for prognosis (12). Therefore, the extent of adequate LN dissection has again become a matter of debate recently (13,14). LN dissection in EC is an old topic, but still requiring discussions.
Chen and colleauges suggested that abdominal LN metastasis is not rare and is associated with poor survival (15). Abdominal LN dissection is a standard surgical procedure in thoracic EC, Shim et al. showed that for suitable people after preoperative evaluation, common hepatic artery LN dissection may be safely omitted (16).
In our retrospective study, the metastatic rate of celiac axis node involvement in thoracic EC is 22.2%. Seto et al. suggested that celiac axis nodes should be reclassified as regional LNs before the proposal of the new staging system (17). However, common hepatic artery LNs are located more distantly from the esophagus, and the metastatic rate of common hepatic artery LN was less frequent metastasis compared with celiac axis LNs and left gastric artery LNs (18), only 3.5% in our study and the left gastric artery LN metastatic rate is 27.42%. Furthermore, the celiac axis LNs can be dissected together with the left gastric artery LNs during gastric graft preparation. While the dissection of common hepatic artery node requires exposure of an additional surgical plane near the cisterna chyli and can result in complications such as chylous ascites (19,20). However, no case of chylous ascites was experienced in our institute among curative thoracic EC surgeries.
Among the 682 patients with esophageal thoracic squamous cell carcinoma, a total of 18,277 LNs were dissected, 24 had common hepatic artery LN metastasis, and the metastatic rate is the lowest compared with others (Table 3). Logistic regression analysis identified that tumor diameter (P=0.014), N classification (P<0.01) and pathological TNM stage (P<0.01) correlated with the occurrence of common hepatic artery LNMs. Rice et al. suggested that the depth of tumor invasion was associated with LNMs (21), but no significance difference was found between the tumor invasion and common hepatic artery LN metastasis in our study. For stage T1 tumors, common hepatic artery LN metastasis occurred in 2 (2.38%) of 84 patients with tumor infiltrating the submucosa (stage T1b), only one patient with tumor limited to the mucosa (stage T1a) was found, and no common hepatic artery LN metastasis was occurred (Table 4). When it comes to the tumor diameter, more studies are required. In our study, no common hepatic artery LN metastasis was found at stage I, while 2 patients and 22 patients was found at stage II and stage III. What about the postoperative complications between the cohorts? To control for potential differences in the characteristics of patients treated with common hepatic artery LN dissection or without common hepatic artery LN dissection, propensity score methods were used to compare the postoperative complications between the cohorts. The overall incidence of anastomotic leakage in the cohort one was lower than that in the cohort two, however, this difference was not statistically significant (P=0.054).
A number of limitations apply to the present study and interpretations should be made with caution. Firstly, this is a retrospective study at our institute; therefore, selection bias was unavoidable. However, propensity score-matching gives the present study the power to represent; Secondly, there were some variability in the experience and skill of individual surgeons.
In conclusion, the metastatic rate of common hepatic artery LN is low. Common hepatic artery LN may be safely omitted in esophagectomy for thoracic esophageal squamous cell carcinoma at stage I. Though LN dissection is an old topic, curtail unnecessary LN dissection is still the most important issues to be resolved for EC, and further accumulation of data and prospective studies are warranted in the future.
Acknowledgements
This work was supported by the grant from the Shanghai Rising-Star Program (11QH1400600), National Natural Science Foundation of China (81272608) and National Natural Science Foundation of China (81102044).
Disclosure: The authors declare no conflict of interest.
References
- Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin 2010;60:277-300. [PubMed]
- Kayani B, Zacharakis E, Ahmed K, et al. Lymph node metastases and prognosis in oesophageal carcinoma--a systematic review. Eur J Surg Oncol 2011;37:747-53. [PubMed]
- Nishihira T, Sayama J, Ueda H, et al. Lymph flow and lymph node metastasis in esophageal cancer. Surg Today 1995;25:307-17. [PubMed]
- Sannohe Y, Hiratsuka R, Doki K. Lymph node metastases in cancer of the thoracic esophagus. Am J Surg 1981;141:216-8. [PubMed]
- Takubo K, Makuuchi H, Fujita H, et al. Japanese Classification of Esophageal Cancer, tenth edition: part I. Esophagus 2009;6:1-25.
- Japan Esophageal Sociaty. Japanese classification of esophageal cancer, tenth edition: parts II and III. Esophagus 2009;6:71-94.
- Shim YM, Park JS, Lee M, et al. Can common hepatic artery lymph node dissection be safely omitted in surgery for clinical T1N0 thoracic esophageal squamous cell carcinoma? Dis Esophagus 2013;26:272-5. [PubMed]
- Edge S, Byrd DR, Compton CC, et al. American Joint Committee on Cancer (AJCC) cancer staging manual. 7th ed. Chicago, III: Springer, 2010.
- Lerut TE, de Leyn P, Coosemans W, et al. Advanced esophageal carcinoma. World J Surg 1994;18:379-87. [PubMed]
- Jauch KW, Bacha EA, Denecke H, et al. Esophageal carcinoma: prognostic features and comparison between blunt transhiatal dissection and transthoracic resection. Eur J Surg Oncol 1992;18:553-62. [PubMed]
- Waterman TA, Hagen JA, Peters JH, et al. The prognostic importance of immunohistochemically detected node metastases in resected esophageal adenocarcinoma. Ann Thorac Surg 2004;78:1161-9; discussion 1161-9. [PubMed]
- Rice TW, Blackstone EH, Rusch VW. 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol 2010;17:1721-4.
- Zhang HL, Chen LQ, Liu RL, et al. The number of lymph node metastases influences survival and International Union Against Cancer tumor-node-metastasis classification for esophageal squamous cell carcinoma. Dis Esophagus 2010;23:53-8. [PubMed]
- Li H, Yang S, Xiang J, et al. The number of lymph node metastases influences survival and International Union Against Cancer tumor-node-metastasis classification for esophageal squamous cell carcinoma: does lymph node yield matter? Dis Esophagus 2011;24:108. [PubMed]
- Chen G, Wang Z, Liu XY, et al. Abdominal lymph node metastasis in patients with mid thoracic esophageal squamous cell carcinoma. World J Surg 2009;33:278-83. [PubMed]
- Shim YM, Park JS, Lee M, et al. Can common hepatic artery lymph node dissection be safely omitted in surgery for clinical T1N0 thoracic esophageal squamous cell carcinoma? Dis Esophagus 2013;26:272-5. [PubMed]
- Seto Y, Fukuda T, Yamada K, et al. Celiac lymph nodes: distant or regional for thoracic esophageal carcinoma? Dis Esophagus 2008;21:704-7. [PubMed]
- Akiyama H, Tsurumaru M, Kawamura T, et al. Principles of surgical treatment for carcinoma of the esophagus: analysis of lymph node involvement. Ann Surg 1981;194:438-46. [PubMed]
- Yau KK, Siu WT, Li MK. Chylous ascites in a patient with esophageal carcinoma. Clin Gastroenterol Hepatol 2005;3:A33. [PubMed]
- Lamb PJ, Dresner SM, Robinson S, et al. Chylous ascites complicating esophagectomy. Dis Esophagus 2001;14:67-9. [PubMed]
- Rice TW. Superficial oesophageal carcinoma: is there a need for three-field lymphadenectomy? Lancet 1999;354:792-4. [PubMed]