Elastic stable chest repair and its hybrid variants in 86 patients with pectus excavatum
Introduction
Congenital chest wall deformities have been fascinating doctors since the 16th century (1). Pectus excavatum (PE), a funnel-shaped impression of the anterior chest wall, causes functional limitations in addition to an atypical cosmetic appearance with potentially serious psychological consequences (2,3). When these physical manifestations persist despite athletic training and physiotherapeutic exercise, surgical correction is often recommended (4). This operation is traditionally performed through open surgical access to the sternum, severing the deformed ribs, and lifting the sternum with sutures or metallic implants (5,6).
A paradigm shift was introduced by Nuss’s innovative surgical technique in 1998. This “Minimally Invasive Reconstruction of Pectus Excavatum” (MIRPE) involves retrosternally introducing a steel bar through a minimal skin incision in young patients, and pushing the deformed anterior chest wall forward without cartilage and bone incisions (7). Its success relies on the growth-directing effect of the bar and usually requires 3 to 5 years of bar-stay in order to finally obtain a fully remodeled chest wall. Although this method is currently used in most patients, there are some complex deformities that are more effectively managed by an open correction surgical procedure.
There are considerable differences between the different correction procedures in terms of the mobilization, reduction, and stabilization of the chest wall.
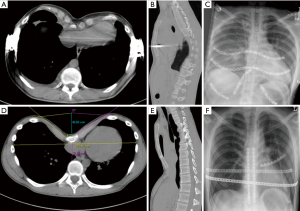
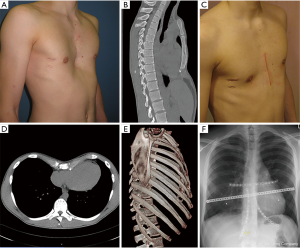
The closed mobilization of the chest wall by internal pressure in the context of the MIRPE is expediently applied in the growth phase or as long as the chest wall is elastic enough but has a higher complication rate in fully formed adults (8-10). As elasticity decreases with age and also with the degree of asymmetry of the deformity, open surgical procedures allow more precise mobilization and reduction of the chest wall. Today, cartilage-saving resection techniques relieve the deformity at the crests of the ribs and the sternum and also allow an en bloc repositioning of the mobilized chest wall (6,11). Subsequently the restoring forces are lower in contrast to MIRPE and thus the fixation of the correction result can be done with various implants in a low-profile design until its consolidation (12). Particularly precise fixation allows for the use of locked plate systems with a low-profile design towards the preservation of the functional elasticity of the thoracic wall (Figures 1,2). Elastic stable chest repair (ESCR) can also be applied to the most complex deformities, even those with strong asymmetry and to recurrent deformities, which may result in instability of the ribs, sternum, and their connections after open resecting procedures (Figures 3,4). ESCR combines sternum and rib osteosynthesis with the correction of chest wall deformities (13,14).
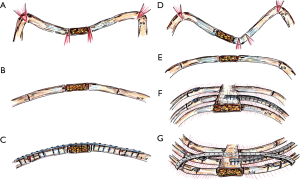
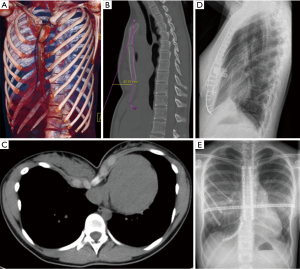
The challenges of correction and stabilization arise when treating particularly broad-based deformities and those with pronounced asymmetry, accompanied by helical torsion of the sternum and adjacent ridge valleys (15) (Figures 2D,E,F,3). To manage these adequately, we have seen in clinical practice the use of hybrid methods indicated. Osteotomy and chondrotomy corrections to sternum and ribs are stabilized by using traditional transsternal metal bars and supplemental locked plates and possibly intramedullary titanium splints.
The aim of this study was to compare stabilization in open funnel chest correction by plate osteosynthesis with stabilization in hybrid methods. The primary endpoint of the analysis was the measurable correction result, and secondary complications were also compared.
Methods
Study design
All PE patients who received an open correction or revision of relapse using either ESCR (Group A) or a hybrid technique (Group B) from January 2011 to November 2015 were included in this retrospective study.
Children under the age of 16 and patients with a history of septic wound healing (n=3) or a history of malignant disease (n=1) were excluded from this study.
Operation (OP) method
Patients underwent open surgery under general anesthesia in a supine position. All of the procedures in each group were performed by the same two senior surgeons. To reach the deformed areas, a median skin incision was made in male patients and a transversal, submammary incision in female patients. Pre-operative computed tomography (CT) planning was performed to determine the length of cut for the necessary osteotomies and chondrotomies of the sternum and the ribs. This was then carried out intra-operatively after planning until the anterior chest wall remained tension-free at the desired anatomical and physiological level. Chest drains were bilaterally inserted and the chest wall was then stabilized by metallic implants.
Transsternal titanium bars (10 mm × 300 mm, Lettenbauer, Erlangen, Germany), low-profile titanium plates of various lengths, and intramedullary rib-splints were used (MatrixRib™, TiAl, 1.5 mm, 2.9 mm self-tapping screws, DePuySynthes, Oberdorf, Switzerland).
In Group A, only locked plates were used including at least one long transverse plate from rib to sternum to rib. These plates provided a positive repositioning of the anterior chest wall as they bridged all osteochondrotomies. Optionally, further plate osteosyntheses were applied to the sternum and rib correction zones.
In Group B, combinations of materials were used with at least one transverse metal bar. Sternal osteotomies were stabilized by longitudinal plates and rib corrections either by plates or with intramedullary splints at the bony part of the ribs.
The wound closure was performed in both groups following an institutional standard procedure under stratified soft tissue reconstruction with reinsertion of the mobilized pectoral musculature, subcutaneous, and intracutaneous sutures.
Follow-up examination
All patients underwent a follow-up examination at 6, 12 weeks, and 1 year after surgery.
Patients were interviewed about their satisfaction and the functional outcome. The soft tissue was examined after the scars possible problems due to palpable or interfering implants. Furthermore, thoracic breathing under unchallenged and forced respiratory cycles was clinically assessed for physiology.
X-ray thorax examination and, in justified cases, CT of the thorax were performed at these follow-up visits.
The results were measured clinically and with imaging to compare the pre- and post-operative findings using the Haller index (HI) (16). The bony structures were evaluated in the area of the osteochondrotomies for signs of bone consolidation and possible remodeling.
The material position of the implants was thoroughly examined and their condition described. Explicit searches were made for dislocations, especially after intrathoracic intervention and for material failure.
The occurrence of secondary complications was also thoroughly investigated and recorded.
Theory and calculation
Since both of the procedures address all of the deformities and stabilized them properly there should not be any significant difference in their outcome parameters. However, it remains exciting if there were differences their possible complications. The data were interpreted using EXCEL (Microsoft® Excel®2016, Santa Rosa, California, USA) and SPSS (Version 21, IBM, Armonk, New York, USA).
Results
The collective
Eighty-six patients with PE met the inclusion criteria. Of these, 38 patients were treated by ESCR (Group A) and 48 patients by the hybrid technique (Group B).
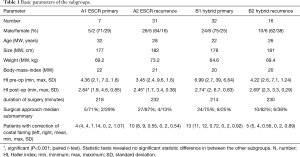
The average age was 23.7 years (12.4–63.5; SD=11.1) in primary operations (n=39, 10 female) and in recurrence corrections (n=47, 11 female) 27.1 year (14.8–49.8; SD=8.8) (Table 1).
Full table
Pain was the indication for a revision procedure in 38 patients (81.0%), 24 of which had nonunion (63.2%).
The number of previous surgeries ranged from one to nine (one OP 62%, two OP 25%, three OP 4%) and averaged 6.2 years (SD 5.2). In 17 patients (36.2%), MIRPE was their initial procedure, in 30 an open procedure (63.8%), of which 10 included transsternal bars (21.3%).
Implants
In Group A, an average of 3.3 plates was used. Group B required an average of 1.1 transsternal bars and an additional 1.9 plates (30 patients) and 2.6 intramedullary splints (15 patients). A detailed overview is shown in Table 2.
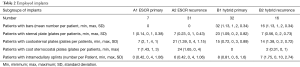
Full table
The implant distribution between groups was also different with respect to primary surgery and recurrence correction. For primary correction, bar implantation was required in 30 patients (77%) and in 16 (34%) for relapse. All patients received plates. In primary correction, 36 plates were used longitudinally in 24 patients (61.5%) and 16 plates in 14 patients with recurrent deformities (29.8%). Ten patients each had costosternal single (25.6%) and bilateral plates (25.6%), and two patients required three or four costo-sternal plates (recurrence: 74.5%). A costo-sterno-costal fixation was recorded in seven patients (18%) supplied with two or three plates (recurrence: 55.3%).
Ribs at the lower costal margin were corrected in 16 patients (41.0%) with 31 plates [recurrence: 15 (31.9%)/26], additional ribs in 14 patients (35.9%) with 23 plates [recurrence: 4 (8.5%)/6] (Table 2).
Operation time
Surgical time was 214 minutes (135–290 min, SD=39) for primary surgery and considerably longer for recurrence procedures (231 min, 135–418 min, SD=61). There was no significant difference between Groups A and B (Table 1).
Correction results
The patients showed remarkable cosmetic improvement in follow-up studies with nearly all displaying no evidence of residual deformity and a healthy mean HI (2.56 primarily/2.54 recurrence) (Table 1); 38.4% of patients requested material removal (64.1% primary, 17.0% recurrence) as part of another operation.
Physiology
Physiological examination of the chest wall revealed healthy respiratory mechanics with a harmonious extension of the anterior chest wall in 34 of 38 cases in Group A, and 41 of 48 cases in Group B. For the remaining 12.8% of patients, respiration was mildly limited but did not lead to patient complaints.
Since only full-grown patients were included in this investigation, there was no development of a growth disorder or acquired Jeune syndrome. Also, rigidity was not observed in any of the cases.
Implant position
The X-ray follow-up examinations at 6, 12 weeks, and 1 year in all cases showed veritable material positions without changes to the post-operative X-ray control and without any dislocation. In 5 of 38 cases in Group A, plate osteosynthesis had a near-center rupture in the plate, whereas in Group B, no such cases were observed. However, a loss of the repositioning of the chest wall was detected in one patient from Group B who had grown again at the age of 17, likely causing the material failure. The remaining patients showed no loss in correction.
Remodeling
Examination of the osteo- and chondrotomies in X-ray thorax examinations showed, in particular, as far as bony assessments are possible, a veritable consolidation with callus formation from the time of admission 6 weeks postoperatively. In the further course was here a remodeling of the ribs to a normal level to observe. In eight cases, CT examination was required because patients either suffered an accident or still experienced slight abnormal sensations on the anterior chest wall. In all cases, CT examination confirmed the true material position and a true bony consolidation with remarkable remodeling of the ribs corrected by wedge osteotomy. Even challenging cases of PE recurrence with unstable anterior chest walls showed a veritable material situation and signs of bony consolidation of the pseudarthrosis. These were managed with the combination of raising the chest wall and stabilizing the pseudarthroses, which were refreshed and augmented with cancellous bone.
External cardiac massage
Two of the 86 patients (Group A2) had to be mechanically reanimated immediately following the operation, as they suffered a sudden cardiac arrest due to pre-existing conditions. In both cases, the patients survived the event without any neurological consequences or loss of correction of the newly mobilized anterior chest wall. The first patient showed an intact material layer without any relaxation signs but experienced a rib fracture on the margin of two rib plates that was treated conservatively. Since these fractures showed minor dislocations and were directly sub-mammary, no cosmetic disadvantage resulted and the remaining course was uncomplicated.
The second patient also suffered from a PE recurrence and was treated by means of three transversal costo-sterno-costal plates and a special tricosto-sterno-tricostal plate in the xiphoid area. Again, the resuscitation proceeded successfully. Only the lower edge of the sternum broke out of the plate. The plate could be sufficiently reaffixed to the sternum during a minor follow up procedure and the bone grafts were left in situ. The follow-up examinations consistently indicated proper consolidation, a very good correction result, and very good physiological function of the anterior chest wall with high patient satisfaction.
Discussion
Overall, ESCR and its hybrid methods are highly safe and effective for chest wall correction. Major surgery-related complications with organ injuries, which are rarely described in MIRPE, did not occur (17).
These surgical techniques also proved successful in terms of patient acceptance and restoring the physiological parameters of unaffected chest wall mobility.
Only a few patients reported a foreign body sensation, indicating that low-profile titanium plates with 1.5 mm material thickness produce excellent results. In contrast, sternum-supporting metal bars are often palpable through the skin and soft tissue and can cause friction in the tissue due to movements between the bar, ribs, and musculature; this can cause sudden pain, hematomas, fluid retention, and chronic inflammation (10).
Plates fixed anatomically to the ribs showed appropriate material integration during follow-up examinations and material removals. Thus, the titanium plates very easily became well-integrated into the bone, likely due to the high primary stability of the titanium material (18).
From a biomechanical perspective, a spanning plate osteosynthesis of the entire anterior chest wall can be seen as an internal plate fixator. Individual segments of the ribs, which are unstable by incision or did not consolidate after previous operations, are assembled in an overall alignment and at the same time held in place at the anatomical level. Thus, the elevation and the stabilization are achieved in one step (14). The plate is not able to slide over the ribs due to its defined length and lateral fixation and conversely, the ribs underneath cannot move away from the plate. In this study, the sternal fixation was accomplished with three to four screws, so that the sternum was fitted as a capstone with optimal anatomical configuration in the anterior chest wall. In the context of continuous respiratory activity, micro-movements in the area of the osteo- and chondrotomies occur as compressions in the fracture gap so that healing of a biological fracture is obtained by means of elastic plate osteosynthesis. In principle, this is similar to the internal plate fixator, a locked plate similar to that used on long bones, which utilizes the principle of vibrating plate osteosynthesis in complex fractures such as comminuted ones (19,20).
For the first time, we were able to monitor these extensively studied and described phenomena in the anterior chest wall under critical observation of the ESCR.
Another benefit of this approach is the prevention of recurrence as the plate is laterally fixed to the ribs and therefore, for physical reasons, no impression in the central area can take place. This property is also of crucial importance for cardiopulmonary resuscitation during the rarely necessary, but extremely vital, external thoracic wall compression (21-23). Chest compression may not be possible when using the rigid steel bar essential to the Nuss procedure (24). For all other bars with elastic, lateral fixation, compression is possible whilst the underlying incisions of the ribs are reinforced adequately.
Fortunately, both patients recovered quickly and without complication from their cardiac arrests, however, the necessary, complete intensive care monitoring during the postoperative course must be considered.
It is reasonable on the basis of these case studies that ESCR enables successful resuscitation with impressive physiological performance of the chest wall in this stressful situation. However, very few accounts of resuscitation in patients after open chest wall correction have yet to be reported in the literature (21,24).
The investigation on material failure showed a spontaneous plate fracture in some cases, including one after considerable external trauma caused by an accident; this case was therefore considered separately. The remaining material fractures can be attributed to material fatigue as a part of the permanent respiratory effort. Interestingly, however, these four chest walls both showed very good remodeling and optimal sternum positioning. Thus, from a biomechanical point of view, complete bone healing is associated with strong cartilage and bone stability, which differ in vibrational behavior from that of the elastic vibration that the rather rigid metal implant material undergoes in everyday life.
Thus, a break is expected after cyclic loading of the material. However, in all cases, this was completely sequence-free and also symptom-free, and was only noticed in the X-ray routine examinations. Subsequent material removal was easily achieved. The exploration of the ribs after removal of the plate showed complete stability and a matured remodeling so that the correction incisions of the cartilage and bone could no longer be reproduced.
In reference to the material, bending tests carried out in a biomechanical laboratory during the development phase of the panels confirmed the feasibility of cyclic loading over the range of about 100 million bending cycles. When extrapolated, the average service life of the plates was calculated to be around three months (25).
In most cases, however, the plate has become an integral part of the anterior chest wall and displays virtually no relative movement and therefore a tiring material break is relatively rare. It is necessary to explore changes to the material structure (e.g., material thicknesses or different materials) however, the orthopedics and traumatology fields collectively tout the tremendous advantages of titanium alloys for implants due to their low weight, high elasticity, and deformation moments, and the excellent biological integration of materials as discussed above (26).
The hybrid procedure also showed excellent results with high safety in this study. In principle, there is the aforementioned risk of dislocation of a metal bar but this was not observed. It is crucial in our experience to use the longest bars possible, which cross at least two ribs on each side to prevent sliding into the chest cavity. In addition, the stabilization of anterolateral rib osteotomies by intramedullary splints has proven to be very effective. The bar is unable to break through the stabilized rib and their healing and remodeling are superbly supported in the desired position.
Another positive aspect of the hybrid method is that virtually all deformities can be treated successfully. These include the highly asymmetric funnel chest with significant sternum torsion and frequent, parasternal, deep rib valleys, as well as very broad base forms, which are no longer sufficiently straddled by a long plate. Since the material load also increases with increasing plate length and asymmetry, the hybrid method reduces the risk of the aforementioned material fatigue.
However, for correction, preservation, and stabilization of pronounced rib valleys, the plates are of particular use for the correction of costal flaring, as they ensure precise rib alignment and thereby facilitate proper remodeling. The present analyses establish that there are no major differences compared to pure ESCR with regard to surgery time, correction results, and secondary complications.
It is again discussed here that any form of bar implantation produces pressure on the anterior chest wall during retrosternal application (MIRPE) or in the transsternal application in open procedures. In this case, the bar is subject to considerable elastic deformation and the multi-fragmentary bilateral unstable chest wall is supported only by a non-anatomically placed implant. An osteosynthesis of the osteo- and chondrotomies is omitted in addition to the anatomical support at the corresponding rib level. However, this is made possible by the use of a long, locked titanium plate that ensures the appropriate anatomical structure of the anterior chest wall, as described in ESCR (14). Finally, the physiological parameters of the anterior chest wall are well-preserved. Correspondingly, remaining restorative forces could also be effectively transmitted internally by the dome from the central sternum to the paramedian and lateral rib sections by the plate fixator. Based on architectural principles, this elastic tension represents a key function of the ESCR and thus forms the fundamental element of a freshly corrected, destabilized chest wall after open correction procedures. ESCR thus results in an optimal physiological form and function in the immediate postoperative time.
Impressively, the present study reveals that a bar support can very well stabilize even challenging, complex deformities when combined with direct osteosynthesis procedures, as has been described in the context of revisions to the MIRPE (9). Plates are applied locally to deformed key points of the anterior chest wall toward providing modular correction. Important examples include the sternum, local rib deformities, and strong impressions of serial ribs or deformed lower costal arches. In the correction of recurrences, this indication extends to the stabilization of former osteo- and chondrotomies from healing disorders (i.e., pseudarthrosis) (13).
Conclusions
In summary, ESCR and its hybrid variants represent highly effective methods for correcting simple and complex anterior chest wall deformities and their recurrence.
Acknowledgements
None.
Footnote
Conflicts of Interest: S Schulz-Drost is a member of the AO Thoracic Expert Group (THEG) and has a consultant agreement with DePuySynthes. The other authors have no conflicts of interest to declare.
Ethical Statement: Ethical Committee of the faculty of medicine of the FAU Erlangen-Nuremberg confirm that an approval of the ethics committee was not necessary in this retrospective study. No experiments on humans had been done.
References
- Brochhausen C, Turial S, Müller FK, et al. Pectus excavatum: history, hypotheses and treatment options. Interact Cardiovasc Thorac Surg 2012;14:801-6. [Crossref] [PubMed]
- Krille S, Müller A, Steinmann C, et al. Self- and social perception of physical appearance in chest wall deformity. Body Image 2012;9:246-52. [Crossref] [PubMed]
- Ewert F, Syed J, Kern S, et al. Symptoms in pectus deformities: A scoring system for subjective physical complaints. Thorac Cardiovasc Surg 2017;65:43-9. [Crossref] [PubMed]
- Kelly RE Jr, Cash TF, Shamberger RC, et al. Surgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: multicenter study. Pediatrics 2008;122:1218-22. [Crossref] [PubMed]
- Ravitch MM. The operative treatment of pectus excavatum. Ann Surg 1949;129:429-44. [Crossref] [PubMed]
- Gall FP, Hegemann G, Kollermann MW, et al. Surgical treatment of funnel chest. Dis Chest 1967;52:10-4. [Crossref] [PubMed]
- Hebra A, Swoveland B, Egbert M, et al. Outcome analysis of minimally invasive repair of pectus excavatum: review of 251 cases. J Pediatr Surg 2000;35:252-7. [Crossref] [PubMed]
- Nuss D, Obermeyer RJ, Kelly RE Jr. Pectus excavatum from a pediatric surgeon's perspective. Ann Cardiothorac Surg 2016;5:493-500. [Crossref] [PubMed]
- Ashfaq A, Beamer S, Ewais MM, et al. Revision of failed prior Nuss in adult patients with pectus excavatum. Ann Thorac Surg 2018;105:371-8. [Crossref] [PubMed]
- Choi S, Park HJ. Complications after pectus excavatum repair using pectus bars in adolescents and adults: risk comparisons between age and technique groups. Interact Cardiovasc Thorac Surg 2017;25:606-12. [Crossref] [PubMed]
- Fonkalsrud EW. Open repair of pectus excavatum with minimal cartilage resection. Ann Surg 2004;240:231-5. [Crossref] [PubMed]
- Weber PG, Hümmer HP. The new Erlangen Technique of funnel chest correction – minimalization of a well working procedure. Zentralbl Chir 2006;131:493-8. [Crossref] [PubMed]
- Schulz-Drost S, Syed J, Besendörfer M, et al. Sternocostal dislocation following open correction of pectus excavatum – “stairway phenomenon”: complication management by means of sternocostal locking titanium plate osteosynthesis. Thorac Cardiovasc Surg 2014;62:245-52. [PubMed]
- Schulz-Drost S, Syed J, Besendörfer M, et al. Elastic stable chest repair as a means of stabilizing the anterior chest wall in recurrent pectus excavatum with sternocostal pseudarthrosis: An innovative fixation device. Thorac Cardiovasc Surg 2015;63:419-26. [PubMed]
- Coelho Mde S, Silva RF, Bergonse Neto N, et al. Pectus excavatum surgery: sternochondroplasty versus Nuss procedure. Ann Thorac Surg 2009;88:1773-9. [Crossref] [PubMed]
- Ewert F, Syed J, Wagner S, et al. Does an external chest wall measurement correlate with a CT-based measurement in patients with chest wall deformities? J Pediatr Surg 2017;52:1583-90. [Crossref] [PubMed]
- Hebra A, Kelly RE, Ferro MM, et al. Life-threatening complications and mortality of minimally invasive pectus surgery. J Pediatr Surg 2018;53:728-32. [Crossref] [PubMed]
- Carlsson L, Röstlund T, Albrektsson B, et al. Osseointegration of titanium implants. Acta Orthop Scand 1986;57:285-9. [Crossref] [PubMed]
- Stoffel K, Dieter U, Stachowiak G, et al. Biomechanical testing of the LCP - how can stability in locked internal fixators be controlled? Injury 2003;34 Suppl 2:B11-9. [Crossref] [PubMed]
- Wagner M. General principles for the clinical use of the LCP. Injury 2003;34 Suppl 2:B31-42. [Crossref] [PubMed]
- Grupp S, Fürst V, Buder T, et al. Comparative studies of different types of osteosynthesis on the human corpse preparation in bilateral antero-lateral flail chest. Injury 2017;48:2709-16. [Crossref] [PubMed]
- Firstenberg MS, Crestanello J. Durability of sternal plating after respiratory arrest requiring chest compressions. Ann Thorac Surg 2011;91:988-9. [Crossref] [PubMed]
- McKay DR, Fawzy HF, McKay KM, et al. Are chest compressions safe for the patient reconstructed with sternal plates? Evaluating the safety of cardiopulmonary resuscitation using a human cadaveric model. J Cardiothorac Surg 2010;5:64. [Crossref] [PubMed]
- Zoeller GK, Zallen GS, Glick PL. Cardiopulmonary resuscitation in patients with a Nuss bar --a case report and review of the literature. J Pediatr Surg 2005;40:1788-91. [Crossref] [PubMed]
- MatrixRIB. Stable Fixation of normal and osteoporotic ribs. Technique guide. West Chester, PA: DePuySynthes CMF, 2013.
- Uhthoff HK, Bardos DI, Liskova-Kiar M. The advantages of titanium alloy over stainless steel plates for the internal fixation of fractures. An experimental study in dogs. J Bone Joint Surg Br 1981;63-B:427-84. [Crossref] [PubMed]


