
Recurrence of pectus excavatum following the Nuss procedure
Introduction
Pectus excavatum (PE) is the most common congenital chest wall disorder and is characterized by anterior chest wall depression (1-3). The Nuss procedure (NP) has been established as standard surgical techniques to repair PE (2,4-6). The NP corrects PE by the placement of metal bars in the retrosternum to lift the depressed chest wall (2,7). The duration of bar placement is usually about two to three years according to the patients’ status (8). Recent studies have reported better outcomes after the NP than following the Ravitch procedure (5,6). However, despite the outstanding outcomes of the NP, the recurrence of PE—in other words, chest wall depression after the completion of repair—is one of the most important issues in PE (5,9). Many previous studies have reported that depression of the anterior chest wall after bar removal (BR) can occur and we occasionally observe a considerable chest wall depression after the completion of treatment (7,8,10,11). Especially, due to the recurrence of PE that may happen, there is an ongoing debate regarding the optimal age for the NP (1,2,12). However, because the recurrence of PE is multifactorial and there are few studies on it, little about the recurrence of PE is known (4,12,13). In addition, there is no established definition of the recurrence of PE after the completion of treatment (12). In this sense, the present study aimed (I) to evaluate the characteristics of chest wall depression during treatment and (II) to present the definition of recurrence of PE, investigate the risk factors for recurrence, and predict the recurrence at one year after BR.
Methods
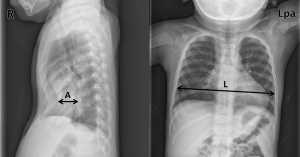
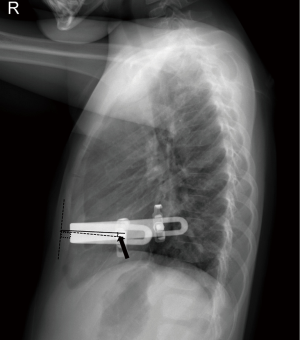
All consecutive patients who underwent BR for PE in a single institution from March 2012 to June 2017 were retrospectively assessed in the present study. The NP was performed in the routine manners of our previous studies (1,7). The inclusion criteria for subjects in the present study were no major complications such as bleeding, a requirement for reoperation, no other combined congenital anomalies or diseases, and no previous surgery for other diseases in the thorax. Simple chest radiographs and three-dimensional chest computed tomography (CT) scans without enhancement were taken in all patients. Simple chest radiographs (posteroanterior and both lateral views) were also routinely taken every day during hospitalization and at every follow-up appointment (all of which were outpatient in nature). Chest CT scans were routinely taken twice for preoperative evaluations before the NP and for the postoperative evaluation of complications and operative results (once on the day before and once on the third day after surgery). The severity of PE is presented as a radiographical Haller index (RHI) in the present study (14). RHI is calculated by the ratio of the transverse diameter to the anteroposterior (AP) diameter at the point of the deepest chest wall depression (14) (Figure 1). The transverse and AP diameters were measured and collected in a double-blind manner by the authors so as to present the degree of chest wall depression. Patients with a ≥3.5 RHI value, which simultaneously increased to more than the value of RHI before BR, were considered as demonstrating recurrence in the present study. Age at the time of the NP, sex, RHI value, pectus morphology type, degree of bar migration, number of bars used, and duration of bar placement were assumed to be the parameters that affect the chest wall depression after BR (3,4). As such, we collected and analyzed data on these clinical parameters during treatment of PE. In our patient cohort, one to two pectus bars were used to correct PE. BR was usually conducted two to three years after the NP, according to patients’ age and condition (8). In order to investigate the chest wall changes after BR, we performed (I) a comparison of the Haller index values calculated with chest radiographs versus CT in order to validate RHI for describing chest wall changes, (II) analyses of characteristics of the chest wall changes after BR, and (III) analyses of the risk factors of the recurrence after BR. In addition, all postoperative chest wall changes were analyzed find out the difference according to the age at the time of the NP; specifically, the subjects were divided into two groups according to whether they were either <10 years old (early group; EG) or ≥10 years old (late group, LG) at the time of the NP.
Statistical analysis
Comparisons between each group were analyzed using the Student’s t-test or the paired t-test. To investigate the relationship between two quantitative continuous variables, Pearson correlation analysis was conducted. The chi-squared statistic was used for investigating relationships between categorical variables. Repeat measures analysis of variance test was performed to analyze the changes of chest wall depression after BR. Multivariate analysis using the logistic regression model (backward, stepwise approach) was performed to determine independent risk factors of the recurrence after BR. Receiver operating characteristic (ROC) analysis was used for prediction for the recurrence of PE using significant variables in the logistic regression model. The results were analyzed using the Statistical Package of Social Sciences version 22.0 software (IBM Corp, NY, USA), with a level of significance of 0.05.
Ethical approval
This study was approved by the institutional review board of Uijeongbu St. Mary Hospital (UC18RESI0091). Written informed consent was obtained from the study subjects prior to their participation. The authors declare no interest to the present study.
Results
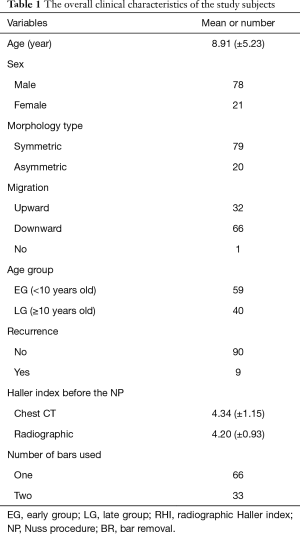
Ninety-nine patients were included into the present study. The mean age of the study participants was 8.91 (±5.23) years at the age of the NP and the mean duration of bar placement was 28.4 (±5.04) months. Seventy-eight males and 21 females were included. The pectus type was 79 symmetric and 20 asymmetric cases. The mean observation period after BR was 16.47 (±3.74) months. The mean Haller index value using chest CT and radiography before the NP were 4.34 (±1.15) and 4.20 (±0.93), respectively, while the mean RHI immediate before BR and one year after BR were 2.57 (±0.40) and 2.92 (±0.44), respectively. Recurrence occurred in nine of the 99 cases. The overall clinical characteristics of the study subjects are presented in Table 1.
Full table
Comparison of Haller index values calculated with chest radiographs versus CT
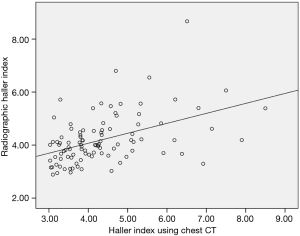
The calculation of the Haller index value using chest CT is standard for describing the severity of PE (15). However, because chest CT is not routinely performed during treatment and follow-ups, we used RHI instead of the Haller index using chest CT. In order to validate RHI for describing the severity of PE, we compared the Haller index values calculated with chest radiographs versus CT. The mean Haller index values using chest CT and radiography immediate before the NP were 4.34 (±1.15) and 4.20 (±0.93), respectively. There was no significant difference in the Haller index values between chest CT and simple radiography (P=0.201), and there was a significant correlation between Haller index using chest CT and simple radiographic data (P<0.001). Therefore, we decided to use RHI for describing the chest wall changes, like as was done in previous studies (Figure 2) (13,15,16).
Chest wall changes immediately after the NP
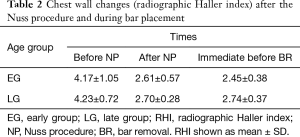
Chest wall changes immediately after the NP were analyzed according to the aforementioned age groups. Irrespective of these age groups, there was a significant decrease in RHI values (both P<0.001). In addition, there were no significant differences in RHI values between the EG and LG cohorts before the NP and immediate after the NP (P=0.775, P=0.356, respectively) (Table 2).
Full table
Chest wall changes during bar placement
Chest wall changes between after the NP and before BR (during bar placement) were analyzed according to the age groups. In the EG, there was a significant decrease in RHI (P=0.040). However, in the LG, there was an increase in RHI, albeit without a significance (P=0.330) (Table 2). This finding showed that in the EG, the chest wall depression presented by RHI was improved during bar placement, while, in spite of bar placement, the chest wall depression in the LG seemed to progress without statistical significance.
Degree of bar migration
The occurrence of bar migration during bar placement was analyzed according to the age groups. Degree of bar migration was defined as a change of the angle between the sternum and the pectus bar during bar placement (Figure 3) (17). We found one case with no migration, 66 cases with downward migration, and 32 cases with upward migration. Lateral migration was not found in the present study. Additionally, there was no difference in the direction of migration according to the age groups (P=0.228). Bar displacement (severe migration) was defined as bar migration of more than 20° in the present study. Bar displacements were more frequent in the EG than in the LG (11 cases in the EG versus three cases in the LG; P=0.149), which was assumed to be due to fewer bar placements in the EG (P<0.001).
Analyses of characteristics of the chest wall changes after BR
Chest wall changes after BR
To analyze characteristics of the chest wall changes after BR, we measured the AP and lateral diameter and RHI changes after BR at the subsequent time points (i.e., immediate, one month, six months, one year after BR) according to the age groups. In the EG, there was a decrease in AP at all subsequent time points (all P<0.001); an increase in lateral diameter (P=0.941, P<0.001, P<0.001, and P<0.001); and an increase in RHI values at all subsequent time points (all, P<0.001) in comparison with those before BR (Table 3). In the LG, there was a decrease in AP at all subsequent time points (all P<0.001); an increase in lateral diameter except immediately after BR (P=0.416, P<0.001, P<0.001, P<0.001); and an increase in RHI values at all subsequent time points (all P<0.001) in comparison with those before BR (Table 3). RHI values in the LG were significantly higher than those in the EG throughout the period after the NP (P=0.019). In comparison with those at six months after BR, AP diameter, suggesting directly the degrees of the chest wall depression, was significantly restored at one year after BR only in the EG (P=0.011). These findings suggest that the chest wall depression progressed for the first six months after BR. However, the chest wall depression did not progress at one year after BR (Figure 4).
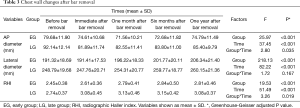
Full table

Recurrence of PE
Our previous studies showed that the early correction of PE is more desirable than late correction in some aspects (1,18,19). However, although we prefer the early correction of PE, there was no definite consensus regarding an appropriate age for the NP due to the recurrence that may occur. In the present study, we analyzed the recurrence of PE according to the age groups. Recurrence occurred in nine cases at one year after BR (four cases in the EG and five cases in the LG). The recurrence rate was higher in the LG than in the EG (P= 0.479).
Analysis of risk factors of the recurrence of PE one year after BR
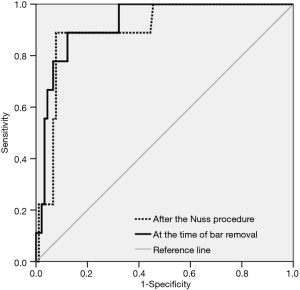
In order to investigate the independent risk factors of the recurrence of PE one year after BR, multivariate analysis was carried out using the logistic regression test. Recurrence at one year after BR was defined as an event. Age at the time of the NP, sex, RHI values before and after the NP, morphological type, number of bars used, degree of bar migration, and duration of bar placement were included as covariates for the multivariate analysis of the recurrence. Accordingly, only RHI value after the NP was identified as an independent risk factor of the recurrence, irrespectively of the age groups. The results of the multivariate analysis of risk factors are shown in Table 4. ROC study showed that RHI value after the NP had a significant predictable cutoff value for the recurrence [cutoff value of RHI: 2.91, sensitivity: 88.9%, specificity: 90.00%, P<0.001, area: 0.899, 95% confidence interval (CI): 0.806−0.993] (Figure 5). In addition, RHI at the time of BR also had a significant diagnostic cutoff value for the recurrence of PE (cutoff value of RHI: 2.88, sensitivity: 88.9%, specificity: 87.8%, P<0.001, area: 0.925, 95% CI: 0.854−0.996) (Figure 5).

Full table
Discussion
Despite the excellent results of the NP achieved in the repair of PE, chest wall depression after BR remains an issue to overcome (5,9). To date, because many previous studies have reported the occurrence of chest wall depression after BR, no consensus on the optimal age for the NP has been reached (1,2). Little about the characteristics of chest wall depression after BR is known (5,9). In addition, it remains unclear as to whether pediatric and adult patients both present the same chest wall change patterns after BR. Chest wall depression is multifactorial and spatial (4). Because no methods or tools are clinically available to fully describe the chest wall depression, it is difficult to clearly explain the chest wall depression after BR (4,9,13,20). To prevent chest wall depression and to obtain persistent corrective results after BR, it is necessary to determine the details of the techniques of the NP, such as size, number, shape, and location of pectus bars (3,4,7,21). We have suggested the optimal details of the NP according to morphologic types in previous studies (1,7). In the present study, we investigated the characteristics of chest wall depression and the risk factors for recurrence after BR using RHI.
Like in previous research, the present study showed the occurrence of chest wall depression after BR (5,9). The chest wall depression progressed for the first six months after BR. However, it was not aggravated at the time of one year after BR. This finding indicated that patients should be followed up with to check up the recurrence of PE for the period of one year after BR. The chest wall changes that occurred during bar placement showed different patterns according to the age groups. RHI value in the EG significantly decreased, while RHI value in the LG increased without significance during bar in placement. In addition, because the RHI value before BR was significantly higher in LG than in the EG, the corrective effect of the repair in the EG was higher than in the LG. The chest wall depression after BR was also different according to the age groups. It was not aggravated at one year after BR irrespective of the age group. However, in comparison with at six months after BR, AP diameter, suggesting directly the degrees of the chest wall depression, was significantly restored at one year after BR only in the EG. In addition, RHI values at one year after BR was significantly higher in the LG than in the EG. These findings showed that early correction of PE seems to be better than late correction with respect to obtaining corrective results (17). To analyze the risk factors for the recurrence of PE, multivariate analysis was carried out. We assumed that the recurrence after BR might be associated with age at the time of the NP, sex, RHI values before and after the NP, morphological type, the number of bars used, degree of bar migration, and duration of bar placement (9). The analysis revealed that only RHI value after the NP was identified as an independent risk factor of the recurrence, irrespectively of the age groups. These findings suggest that sufficient elevation of depressed chest wall is essential to prevent recurrence of PE. ROC analysis also showed that sufficient elevation is essential to prevent the recurrence of PE. Enough duration of bar placement is known to be an important factor in the recurrence (8). However, because all bar placements were maintained over two years in the present study, which is known as enough duration to prevent the recurrence of PE, the duration of bar placement was considered not to be associated with the recurrence. The direction of bar migration was not different according to age group and bar migration was not associated with the recurrence of PE after BR. However, more frequent bar displacement in the EG was found, which was assumed to be due not to age at the time of the NP, but rather the number of bars used. These findings suggest that if sufficient elevation by the pectus bar is obtained, even severe bar migration (displacement) can be clinically acceptable.
On the basis of the above findings, it can be stated that only sufficient chest wall elevation by the NP is associated with the recurrence of PE. In addition, early correction of PE seems to be better than late correction with respect to obtaining corrective results.
Previously, our research has showed that the early correction of PE is more desirable than late correction in some aspects (1,13,20,21). Although we prefer an early correction of PE, there was no definite consensus regarding the decision of an appropriate age for the NP due to the recurrence (2,12). The optimal age for the NP remains under debate (2,12). However, our findings suggest that early correction of PE can provide better corrective results because of the existence of a more pliable chest wall, which can be easily and sufficiently elevated by the NP. If we can sufficiently elevate the depressed chest wall, the age at the time of the NP is not important in the context of the recurrence of PE. Surgeons should know the risk factor for the recurrence of PE and be aware that sufficient elevation of the depressed chest wall should be ensured during the NP when deciding upon treatment in PE.
The present study has several limitations. First, it was a small sample size, a retrospective in nature and has selection bias, especially toward the early correction of PE. The retrospective nature of the present study might affect the results. In addition, because the definition of the recurrence of PE may be somewhat arbitrary, our results might have been influenced. Second, some measurement errors might exist due to using simple radiography and due to position, respiration, and other unknown factors. Because it is difficult to fully describe the chest wall depression, the present study presented only the change of the deepest point of the chest wall depression. Third, because the observation period was relatively short, it is unclear whether the recurrence of PE would eventually occur in larger numbers. Further long-term studies are necessary.
Conclusions
The present study shows the characteristics of chest wall depression and the risk factor of the recurrence of PE after BR. The effect of the NP is different according to the patient age at the time of the procedure. Early correction of PE can provide better corrective results because of the existence of a more pliable chest wall, which can be easily and sufficiently elevated by the NP. Sufficient elevation of the depressed chest wall should be ensured during the NP to prevent the recurrence of PE. Additional long-term and prospective research efforts about the recurrence of PE are necessary to validate these findings.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the institutional review board of Uijeongbu St. Mary Hospital (UC18RESI0091). Written informed consent was obtained from the study subjects prior to their participation.
References
- Park HJ, Kim JJ, Park JK, et al. Effects of Nuss procedure on thoracic scoliosis in patients with pectus excavatum. J Thorac Dis 2017;9:3810-6. [Crossref] [PubMed]
- Nuss D, Obermeyer RJ, Kelly RE Jr. Pectus excavatum from a pediatric surgeon's perspective. Ann Cardiothorac Surg 2016;5:493-500. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr. Indications and technique of Nuss procedure for pectus excavatum. Thorac Surg Clin 2010;20:583-97. [Crossref] [PubMed]
- Matsuo N, Matsumoto K, Taura Y, et al. Initial experience with a 3D printed model for preoperative simulation of the Nuss procedure for pectus excavatum. J Thorac Dis 2018;10:E120-4. [Crossref] [PubMed]
- Tikka T, Kalkat MS, Bishay E, et al. A 20-year review of pectus surgery: an analysis of factors predictive of recurrence and outcomes. Interact Cardiovasc Thorac Surg 2016;23:908-13. [Crossref] [PubMed]
- Kocher GJ, Gstrein N, Jaroszewski DE, et al. Nuss procedure for repair of pectus excavatum after failed Ravitch procedure in adults: indications and caveats. J Thorac Dis 2016;8:1981-5. [Crossref] [PubMed]
- Park HJ, Jeong JY, Jo WM, et al. Minimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approach. J Thorac Cardiovasc Surg 2010;139:379-86. [Crossref] [PubMed]
- Chang PY, Zeng Q, Wong KS, et al. Chest Wall Constriction after the Nuss Procedure Identified from Chest Radiograph and Multislice Computed Tomography Shortly after Removal of the Bar. Thorac Cardiovasc Surg 2016;64:70-7. [PubMed]
- Gomes-Fonseca J, Vilaca JL, Henriques-Coelho T, et al. A new methodology for assessment of pectus excavatum correction after bar removal in Nuss procedure: Preliminary study. J Pediatr Surg 2017;52:1089-97. [Crossref] [PubMed]
- Kilda A, Lukosevicius S, Barauskas V, et al. Radiological changes after Nuss operation for pectus excavatum. Medicina (Kaunas) 2009;45:699-705. [Crossref] [PubMed]
- Chang PY, Chang CH, Lai JY, et al. Analysis of changes to the anterior chest wall after the Nuss procedure-an objective measurement of pectus excavatum. J Pediatr Surg 2009;44:2291-5. [Crossref] [PubMed]
- Ishimaru T, Kitano Y, Uchida H, et al. Growth spurt-related recurrence after Nuss procedure. J Pediatr Surg 2009;44:E13-6. [Crossref] [PubMed]
- Chang PY, Zeng Q, Wong KS, et al. A Cross-Sectional Study of Chest Wall Development in Patients with Pectus Excavatum. Thorac Cardiovasc Surg 2015;63:433-6. [Crossref] [PubMed]
- Wu TH, Huang TW, Hsu HH, et al. Usefulness of chest images for the assessment of pectus excavatum before and after a Nuss repair in adults. Eur J Cardiothorac Surg 2013;43:283-7. [Crossref] [PubMed]
- Poston PM, McHugh MA, Rossi NO, et al. The case for using the correction index obtained from chest radiography for evaluation of pectus excavatum. J Pediatr Surg 2015;50:1940-4. [Crossref] [PubMed]
- Sarwar ZU, DeFlorio R, O'Connor SC. Pectus excavatum: current imaging techniques and opportunities for dose reduction. Semin Ultrasound CT MR 2014;35:374-81. [Crossref] [PubMed]
- Binkovitz LE, Zendejas B, Moir CR, et al. Nuss bar migrations: occurrence and classification. Pediatr Radiol 2016;46:1797-803. [Crossref] [PubMed]
- Park HJ, Kim JJ, Park JK, et al. A cross-sectional study for the development of growth of patients with pectus excavatum. Eur J Cardiothorac Surg 2016;50:1102-9. [Crossref] [PubMed]
- Park HJ, Sung SW, Park JK, et al. How early can we repair pectus excavatum: the earlier the better? Eur J Cardiothorac Surg 2012;42:667-72. [Crossref] [PubMed]
- Ewert F, Syed J, Wagner S, et al. Does an external chest wall measurement correlate with a CT-based measurement in patients with chest wall deformities? J Pediatr Surg 2017;52:1583-90. [Crossref] [PubMed]
- Lai JY, Wang CJ, Chang PY. The measurement and designation of the pectus bar by computed tomography. J Pediatr Surg 2009;44:2287-90. [Crossref] [PubMed]


