
Diaphragm and transdiaphragmatic injuries
Introduction
A traumatic diaphragmatic rupture (TDR) can develop in cases of thoracoabdominal injuries and in a very high percent of cases it is associated with other organs injuries. In some cases TDR itself can cause life-threatening complications, but generally the outcome of the injury with TDR depends on the severity of the lesions and complications of the associated organs injury. Hospital mortality is 15% after blunt injuries and 4% after penetrating lesions (1). In case of a significant TDR, diagnosis is simple, although in most cases correct diagnosis is often delayed. When TDR is a part of a polytrauma, the management of the patient must be done according to ATLS (Advanced Trauma Life Support) protocol (2) and treatment can be done in the primary survey, however most typically carried out during the secondary survey.
Incidence
TDR was found in 0.4% of all trauma patients (3) and in 1.9% among blunt trauma cases (4). Eighty percent of TDRs were found on the left side and 20% on the right side among trauma patients (3). It is bilateral in around 3% of the cases (5). Incidence of TDR among penetrating trauma cases is 20–59% with gunshot and 15–32% with stab wounds (6). Autopsy studies suggest an equal incidence of diaphragmatic lacerations on the left and right side, but left-sided lesions are more commonly verified clinically (7). One theory explaining these results could be that the left hemidiaphragm is weaker during embryological development, and it is likely that the protecting effect of the liver on the right side also plays an important role (8,9). There has currently been a slight change in aetiology, since the causes of TDR are more frequently due to penetrating trauma (63%) than blunt injuries (37%) (9). The aetiology of TDR can be as follows: decelerating motor vehicle accidents, falling from great heights and crushing injuries to the lower chest and upper abdomen which are the most frequent causes of blunt diaphragmatic injuries. Stab and gunshot wounds are the most common causes in cases of penetrating diaphragmatic injuries (10-12). There have been reported cases of iatrogenic injuries of the diaphragm either during thoracic or abdominal procedures or secondary to thoracocentesis and radiofrequency ablation (13). Spontaneous rupture during pregnancy and unexplained spontaneous rupture are also reported (10,14).
Pathophysiology
There is a positive gradient of 7–20 watercentimeter between intraperitoneal and intrapleural pressure (15) which may increase ten folds during severe abdominal trauma (16). This positive pressure gradient can exceed 100 watercentimeter during maximum respiratory effort and can result in transdiaphragmatic herniation of the abdominal viscera through the defect (17). Due to the continuous movement of the diaphragm, its injuries cannot heal spontaneously (9,11,12), and the size of TDR usually increases with time, which leads to herniation of the abdominal viscera through the defect (18,19).
The Organ Injury Scaling Committee of the American Association for the Surgery of Trauma proposed a classification system for diaphragmatic injury: Grade I Contusion; Grade II Laceration <2 cm; Grade III Laceration 2–10 cm; Grade IV Laceration >10 cm with tissue loss <25 cm2; Grade V Laceration with tissue loss >25 cm2 (20). In a study, the incidences of the different injuries were found as follows: acute diaphragmatic herniation (30.4%); tears (47.8%); and contusions (21.7%) (2).
Clinical presentation
TDR can be divided into three phases: acute, latent, and obstructive. The acute phase extends from the initial trauma until recovery from the primary injuries. During the latent phase, which can range from days up to 10 years, the hernia is gradually developing, with clinical symptoms of visceral obstruction or ischaemia presenting in the obstructive phase (21).
During the acute phase abdominal-, chest pain, and cardio-respiratory dysfunctions are typically present. During the latent phase clinical symptoms of the herniation will be found, such as upper gastrointestinal complaints; pain in the left upper quadrant or in the chest; dyspnoea/orthopnoea; decreased breathing sounds. In the obstructive phase, previously mentioned symptoms progress, and the signs of peritonitis can develop.
Diagnosis
The diagnosis of traumatic diaphragmatic injury is not always easily made. Special imaging procedures may be used, but they are time-consuming and may provide an additional risk for polytrauma patients by causing a delay in adequate management. In the primary survey, chest radiography is currently the most valuable simple test, although it is diagnostic or suggestive of a diaphragmatic rupture in only 25–70% of cases (22,23). Signs on chest radiography, e.g., irregularity of the diaphragmatic outline, elevated diaphragm, mediastinal shift without pulmonary or intrapleural cause and compression atelectasis of the lower lobe, might suggest a diaphragmatic rupture (24,25). Additionally, a radiopaque nasogastric tube or simple gastrointestinal studies might also be helpful in revealing a defect or a visceral herniation. Repeated chest radiography during hospitalisation, and after discharge, are necessary in order to detect a slowly increasing herniation (26).
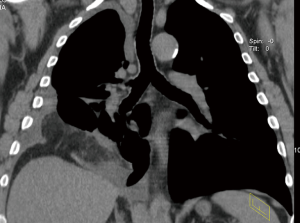
Computed tomography (CT) is the second choice imaging technique, although the axially oriented diaphragm is not always well demonstrated on conventional CT. In a single-layer spiral CT study, the sensitivity for left- and right-sided diaphragmatic injuries was 78% and 50% (27), but with a multidetector CT (MDCT) specificity was 100% and 83% for left and right-sided ruptures, respectively (28) (Figure 1). Currently in polytrauma and trauma cases, including patients with thoracoabdominal trauma, a whole body MDCT is performed (29,30).
Magnetic resonance imaging (MRI) can play an important role in the diagnosis of latent TDR, but helical CT remains the recommended examination in traumatic patients in the diagnosis of TDR (31). In patients with acute herniation, MRI has a very limited use, due to the fact that it is not always available in the acute setting and with numerous trauma patients possessing metal prostheses not compatible with MRI (6).
Contrast studies may be helpful in cases of suspected intrathoracic herniation, whilst a diagnostic pneumoperitoneum or an intraperitoneal injection of technetium are not used nowadays (22,25). There appear to be too many false negative results to depend on a diagnostic peritoneal lavage to identify diaphragmatic damage after blunt trauma, with a false-negative rates up to 25% (7,32). The method is replaced by the more reliable bedside focused assessment sonography for trauma (FAST) (9,26).
When there is a high degree of suspicion, only direct visualisation by laparoscopy or thoracoscopy may exclude/confirm the existence of a diaphragmatic defect. In patients with thoracoabdominal trauma who do not have any abdominal injury and do not require laparotomy, video-assisted thoracic surgery (VATS) is an excellent tool for the diagnosis and treatment of diaphragmatic injury. VATS can be used to manage TDR, remove clots and properly carry out chest drainage, although it cannot be performed in haemodynamically unstable patients and it also requires general anaesthesia and one-lung ventilation, also (33). In case of thoracoabdominal stab wounds or tangential gunshot wounds, when the patient is haemodynamically stable, and there is no sign of peritonitis or diffuse abdominal tenderness, and the patient is in a non-operative method management, a laparoscopy can be indicated to verify a diaphragmatic rupture (34). Another study suggests that if the hemodynamically stable left thoracoabdominal stab wound patients without signs of peritonitis is managed with a non-operative method, 48 hours after admission a diagnostic laparoscopy may be performed to check the diaphragm. In 22% of these patients (15/68) a left diaphragmatic injury was found (35).
Surgical management
About 10% of blunt and 15% to 30% of penetrating chest injuries require operative intervention. Due to the fact that associated injuries determine the choice of treatment, management of these patients is performed according to the rules of ATLS: managements in the primary survey (life-threatening injuries) and the secondary survey (potentially life-threatening injuries) (2). During the primary survey A (airway), B (breathing), C (circulation) D (disability) and E (environment and exposure) are managed.
Management of the acute phase
In case a resuscitative thoracotomy or laparotomy is indicated during the primary survey, the diaphragmatic rupture (if found) could be reconstructed after the treatment of life-threatening injuries. The most frequent therapeutic maneuvers that can be performed during a resuscitative thoracotomy are as follows: removal of pericardial blood causing tamponade, direct control of exsanguinating intrathoracic hemorrhage, open cardiac massage, cross-clamping of the descending aorta to slow blood loss below the diaphragm and increase perfusion to the brain and heart (2). If the primary survey can be managed without resuscitative thoracotomy or laparotomy and it is completed and the patient is stable, the second survey can be performed. TDR is mainly diagnosed and operated during the secondary survey.
In the acute period, approach is determined by the site of the life-threatening injuries. According to a recent study, if the site of the penetrating wound was located in the abdomen, the rate of intraabdominal organ injury was 83%, and in case the penetrating wound was in the thoracoabdominal area of the chest, abdominal organ injury was 55%. According to these results, the authors performed an explorative laparotomy for all patient with penetrating thoracoabdominal injuries, and the most frequent indication for thoracotomy was haemodynamic instability caused by injury to the heart or great vessels (9).
As reported in a different paper, the approach depended on the haemodynamic stability of the patients, and the preference and skills of the surgeon: there is no superiority of one cavity approach over the other in haemodynamically stable patients, but the associated injuries may require a specific approach. Their approaches were as follows: laparotomy (94%) and thoracotomy (6%) (5). In blunt diaphragmatic injuries, the causes of death were found as follows: head injury (25.0%) intra-abdominal bleeding (23.3%), pelvic hemorrhage (18.3%), and the most frequently associated injuries found were as follows: liver (64%), spleen (53%), small bowel and the mesentery (46%), rib fracture (76%) and pulmonary contusion (63%) (4).
During the daily surgical routine, in cases of acute TDR, a laparotomy provides the best mode of diaphragmatic repair, however a transthoracic approach is favoured in cases of delayed TDR (36). In case an exploratory laparotomy a meticulous inspection of both hemidiaphragms is mandatory (37).
In case, any sign of an injury (bleeding, perforation) is verified in the other cavity (abdomen or chest vice versa) during the exploration (laparotomy or thoracotomy) through the diaphragmatic rupture, the rupture of the diaphragm can be enlarged, thus allowing us to explore and manage the injury through a transdiaphragmatic method (Figure 2). If transdiaphragmatic management is impossible, open or minimally invasive exploration of the other cavity (thoracotomy/thoracoscopy or laparotomy/laparoscopy) is necessary.

When dealing with acute diaphragmatic injury there are two rules that should be respected “reduction of the herniated organs into the abdomen;” watertight closure of the diaphragm after the insertion of a chest tube into the hemithorax. The herniated viscera are reduced to the abdominal cavity by gentle traction. Careful passage of a small nasogastric tube placed alongside the herniated organs avoids gastric overdistention. In case of abdominal organ perforation, thorough irrigation of the haemothorax is necessary to prevent the development of thoracic empyema (9,22,25,26).
A simple and small rupture up to 5–6 cm can usually be reconstructed with No. 0 or 1 monofilament non-absorbable or absorbable interrupted sutures (1), while for larger defects, interrupted figure-of-eight or horizontal mattress sutures are required (38). Some authors advocate a two-layer closure for defects >2 cm. The inner layer is an interlocking horizontal mattress that everts the edges of the diaphragm which is reinforced with a running 3-0 non-absorbable suture (38). Sometimes, it is also useful to secure the diaphragm to the ribs. The use of a prosthetic mesh is rarely needed, but it may be occasionally indicated in patients with large defects (10,11,19,38).
If an abdominal injury has been ruled out, either diagnostic laparoscopy or VATS can be used to identify and manage an injury to the diaphragm. Video-assisted thoracoscopy is performed by intubating the patient in lateral decubitus position with a double-lumen endotracheal tube to permit single lung ventilation and facilitate visualisation (33).
Chronic traumatic diaphragmatic hernia
Elective repair of a chronic traumatic diaphragmatic hernia is obligatory, but in cases of visceral obstruction, strangulation or incarceration urgent surgery is needed (25).
Transthoracic, transabdominal or sometimes thoracoabdominal and more recently minimally invasive thoracoscopic approaches are also used for the repair of a chronic diaphragmatic hernia (10,37,39), but the approach largely depends on the experience of the surgeon (25).
Transthoracic approach through the sixth or seventh intercostal space allows freeing the adhesions between the viscera, chest wall and lung, along with decortication, if needed. For right-sided lesions, a transthoracic approach is obligatory since the position of the liver renders the transabdominal repair of the right hemidiaphragm difficult or even impossible (9,37). Thoracoscopy can be successful in elective cases (36,40), however, this approach has some limitations such as the decortication of the lung and/or the obstruction or strangulation of the intrathoracic viscera into the chest. Sometimes enlargement of the defect is also required to allow reduction of the herniated viscera. Once the reduction is carried out, the diaphragm is repaired using the same techniques as described in patients with an acute injury.
In contrast to acute injuries, different meshes might be used in chronic traumatic hernias in order to perform a tension-free repair (25,36,41).
In acute cases the recurrence of the repaired TDR is rare. Early diagnosis and treatment of TDR leads to a better prognosis; which—in the latent phase—depends on the presence of bowel ischaemia, necrosis and sepsis, which can be fairly high (10,22,37).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ties JS, Peschman JR, Moreno A, et al. Evolution in the management of traumatic diaphragmatic injuries: A multicenter review. J Trauma Acute Care Surg 2014;76:1024-8. [Crossref] [PubMed]
- Advanced Trauma Life Support (ATLS) 9th Edition. Student Course Manual American College of Surgeons. Chicago IL, Thoracic Trauma Chapter 4, 2012:94-112.
- Lim BL, Teo LT, Chiu MT, et al. Traumatic diaphragmatic injuries: a retrospective review of a 12-year experience at a tertiary trauma centre. Singapore Med J 2017;58:595-600. [Crossref] [PubMed]
- Chughtai T, Ali S, Sharkey P, et al. Update on managing diaphragmatic rupture in blunt trauma: a review of 208 consecutive cases. Can J Surg 2009;52:177-81. [PubMed]
- Zarour AM, El-Menyar A, Al-Thani H, et al. Presentations and outcomes in patients with traumatic diaphragmatic injury: A 15-year experience. J Trauma Acute Care Surg 2013;74:1392-8. [Crossref] [PubMed]
- Ahmed N, Jones D. Video-assisted thoracic surgery: state of the art in trauma care. Injury 2004;35:479-89. [Crossref] [PubMed]
- Feliciano DV, Cruse PA, Mattox KL, et al. Delayed diagnosis of injuries to the diaphragm after penetrating wounds. J Trauma 1988;28:1135-44. [Crossref] [PubMed]
- Andrus CH, Morton JH. Rupture of the diaphragm after blunt trauma. Am J Surg 1970;119:686-93. [Crossref] [PubMed]
- Hanna WC, Ferri LE, Fata P, et al. The current status of traumatic diaphragmatic injury: lessons learned from 105 patients over 13 years. Ann Thorac Surg 2008;85:1044-8. [Crossref] [PubMed]
- Shah R, Sabanathan S, Mearns AJ, et al. Traumatic rupture of diaphragm. Ann Thorac Surg 1995;60:1444-9. [Crossref] [PubMed]
- Rosati C. Acute traumatic injury of the diaphragm. Chest Surg Clin N Am 1998;8:371-9. [PubMed]
- Mansour KA. Trauma to the diaphragm. Chest Surg Clin N Am 1997;7:373-83. [PubMed]
- Koda M, Ueki M, Maeda N, et al. Diaphragmatic perforation and hernia after hepatic radiofrequency ablation. AJR Am J Roentgenol 2003;180:1561-2. [Crossref] [PubMed]
- Carter BN, Giuseffi J, Felson B. Traumatic diaphragmatic hernia. Am J Roentgenol Radium Ther 1951;65:56-72. [PubMed]
- Waldhausen JA, Kilman JW, Helman CH, et al. The diagnosis and management of traumatic diaphragmatic injuries of the diaphragm including the use of marlex prostheses. J Trauma 1966;6:332-43. [Crossref] [PubMed]
- de la Rocha AG, Creel RJ, Mulligan GW, et al. Diaphragmatic rupture due to blunt abdominal trauma. Surg Gynecol Obstet 1982;154:175-80. [PubMed]
- Waldschmidt ML, Laws HL. Injuries of the diaphragm. J Trauma 1980;20:587-92. [PubMed]
- Kearney PA, Rouhana SW, Burney RE. Blunt rupture of the diaphragm mechanism, diagnosis and treatment. Ann Emerg Med 1989;18:1326-30. [Crossref] [PubMed]
- Wilson RF, Bender J. Diaphragmatic injuries. In: Wilson RF, Walt Al. editors. Management of trauma: pitfalls and practice. 2nd ed. Baltimore: Lippincott-Williams & Wilkins, 1996:432-48.
- Moore EE, Malangoni MA, Cogbill TH, et al. Organ injury scaling. IV: Thoracicvascular, lung, cardiac, and diaphragm J Trauma 1994;36:299-300. [Crossref] [PubMed]
- Grimes OF. Traumatic injuries of the diaphragm. Diaphragmatic hernia. Am J Surg 1974;128:175-81. [Crossref] [PubMed]
- Payne JH Jr, Yellin AE. Traumatic diaphragmatic hernia. Arch Surg 1982;117:18-24. [Crossref] [PubMed]
- Gelman R, Mirvis SE, Gens D. Diaphragmatic rupture due to blunt trauma sensitivity of plain chest radiographs. AJR Am J Roentgenol 1991;156:51-7. [Crossref] [PubMed]
- Hood RM. Traumatic diaphragmatic hernia. Ann Thorac Surg 1971;12:311-24. [Crossref] [PubMed]
- Blitz M, Louie MB. Chronic traumatic diaphragmatic hernia. Thorac Surg Clin 2009;19:491-500. [Crossref] [PubMed]
- Hanna WC, Ferri LE. Acute traumatic diaphragmatic injury. Thorac Surg Clin 2009;19:485-9. [Crossref] [PubMed]
- Killeen KL, Mirvis SE, Shanmuganathan K. Helical CT of diaphragmatic rupture caused by blunt trauma. AJR Am J Roentgenol 1999;173:1611-6. [Crossref] [PubMed]
- Bergin D., Ennis R, Keogh C., et al. The “Dependent Viscera” Sign in CT Diagnosis of Blunt Traumatic Diaphragmatic Rupture. AJR Am J Roentgenol 2001;177:1137-40. [Crossref] [PubMed]
- Scaglione M, Pinto A, Pedrosa I, et al. Multi-detector row computed tomography and blunt chest trauma. Eur J Radiol 2008;65:377-88. [Crossref] [PubMed]
- Eichler K, Marzi I, Wyen H, et al. Multidetector computed tomography (MDCT): simple CT protocol for trauma patient. Clin Imaging 2015;39:110-5. [Crossref] [PubMed]
- Barbiera F, Nicastro N, Finazzo M, et al. The role of MRI in traumatic rupture of the diaphragm. Our experience in three cases and review of the literature. Radiol Med 2003;105:188-94. [PubMed]
- Freeman T, Fischer RP. The inadequacy of peritoneal lavage in diagnosing acute diaphragmatic rupture. J Trauma 1976;16:538-42. [Crossref] [PubMed]
- Freeman RK, Al-Dossari G, Hutcheson KA, et al. Indications for using video-assisted thoracoscopic surgery to diagnose diaphragmatic injuries after penetrating chest trauma. Ann Thorac Surg 2001;72:342-7. [Crossref] [PubMed]
- Como JJ, Bokhari F, Chiu WC, et al. Management Guidelines for Selective Nonoperative Management of Penetrating Abdominal Trauma. J Trauma 2010;68:721-33. [Crossref] [PubMed]
- Yücel M, Özpek A, Kerem H, et al. Importance of diagnostic laparoscopy in the assessment of the diaphragm after left thoracoabdominal stab wound: A prospective cohort study. Ulus Travma Acil Cerrahi Derg 2017;23:107-11. [PubMed]
- Scharff JR, Naunheim KS. Traumatic diaphragmatic injuries. Thorac Surg Clin 2007;17:81-5. [Crossref] [PubMed]
- Athanassiadi K, Kalavrouziotis GM, Athanassiou M, et al. Blunt diaphragmatic rupture. Eur J Cardiothorac Surg 1999;15:469-74. [Crossref] [PubMed]
- Athanassiadi K. Chapter 105: Diaphragmatic Trauma. ESTS textbook of Thoracic Surgery (Volume 2). Cracow: Medycyna Praktyczna, 2015:945-50.
- Haciibrahimoglu G, Solak O, Olcmen A, et al. Management of traumatic diaphragmatic rupture. Surg Today 2004;34:111-4. [Crossref] [PubMed]
- Cetindag IB, Neideen T, Hazelrigg SR. Video-assisted thoracic surgical applications in thoracic trauma. Thorac Surg Clin 2007;17:73-9. [Crossref] [PubMed]
- Furak J. Chapter 68.2: Diaphragmatic Reconstruction. Textbook of Thoracic Surgery (Volume 2). Cracow: Medycyna Praktyczna, 2015:217-21.


