
Oscillating between prone ventilation and ECMO?
Meade et al. (1) have performed an interesting individual patient data meta-analysis to identify subgroups of patients with acute respiratory distress syndrome (ARDS) who had differential outcomes from high frequency oscillatory ventilation (HFOV). This analysis is relevant given the significant differences in trial designs amongst the six studies included in the analysis and possible heterogeneity in treatment effect of HFOV.
The authors report an increased harm from HFOV in patients with mild to moderate ARDS, especially when compared with patients who received lowest tidal volumes (Vt <6.3 mL/kg predicated body weight) on conventional ventilation. There was an increased risk of barotrauma with HFOV. Interestingly, they report a potential survival benefit in patients with a partial pressure of oxygen to fraction of inspired oxygen ratio (PaO2:FiO2) <100 mmHg (OR =0.83 in PaO2:FiO2 <100 mm of Hg group and OR =0.68 in PaO2:FiO2 <64 group). These findings along with the results of the recently published Extracorporeal membrane oxygenation to Rescue Lung Injury in Severe ARDS (EOLIA) trial (2) may reopen the debate for role of HFOV as a rescue therapy for refractory hypoxemia whilst on low Vt, pressure limited lung protective ventilation.
To date, protective ventilation with low Vt (3), early pharmacologic paralysis (4) and early prone ventilation (5) remain the key evidence-based interventions that are shown to improve survival in ARDS. Although low Vt ventilation is recommended for all comers with ARDS, the effects of early prone ventilation and neuromuscular paralysis were tested in patients with moderate ARDS (PaO2:FiO2 <150 mmHg). These measures are now integral to ARDS management and must be, of course, complimented with good general supportive intensive care including a conservative fluid strategy (6).
When patients with ARDS continue to worsen with refractory hypoxia despite management with evidence-based strategies mention above, extracorporeal membrane oxygenation (ECMO) is being increasingly applied (7). Given the lack of conclusive evidence for ECMO and based on the findings from Meade et al. (1), does HFOV move back into contention in this subgroup of patients with refractory hypoxemia especially when there is no access to ECMO? It must be pointed out though that this potential benefit of HFOV in setting of refractory hypoxia hasn’t been replicated in a randomised trial setting. Given the increased risk of barotrauma, HFOV should be applied with great caution and high mean airway pressures should generally be avoided.
Rescue ECMO or early referral for ECMO when access to an ECMO service is available is becoming standard of care. Several countries now have experienced ECMO retrieval teams in place. Keenly awaited results from the EOLIA (2), an international multicenter, randomised trial evaluating the effect of early initiation of ECMO in patients with the most severe forms of ARDS of ECMO are now available. This trial randomised ARDS patients with a PaO2:FiO2 <50 mmHg for more than 3 hours or a PaO2:FiO2 of less than 80 mmHg for more than 6 hours to ECMO. The control group received the most optimal conventional management possible setting high standards for control group management for future ARDS trials. This trial allowed cross over from conventional ventilation arm to ECMO in the case of refractory hypoxemia defined as blood arterial saturation SaO2 <80% for >6 hours, after mandatory use of recruitment manoeuvres, inhaled nitric oxide/prostacyclin and when clinically possible a trial of prone position. In the setting of a high cross over of control subjects to ECMO arm and the higher mortality in those who crossed over, a more controlled initiation of ECMO is rather desirable. Even though the EOLIA trial did not achieve the highly optimistic 20% reduction in mortality compared with conventional ventilation, it did highlight that a substantial proportion of patients fail conventional ventilation with adjuncts, to their own detriment. In this context, EOLIA essentially became a trial of early vs. salvage ECMO. Would EOLIA be a conventionally positive study if the investigators enrolled patients even earlier? e.g., PaO2:FiO2 <100–150 mmHg or if the patients remained in prone position on ECMO? Are the questions that need further investigation.
It should be noted that benefits of prone ventilation and paralysis were observed in patients with PaO2:FiO2 ratio <150 mmHg, Meade et al. report potential benefit with HFOV in patients with PaO2:FiO2 <100 mmHg and EOLIA randomised patients to ECMO when PaO2:FiO2 <50 for >3 h or PaO2:FiO2 <80 for >6 h or PaCO2 >60 mmHg and pH<7.25 for >6 h. The entry criteria and outcomes in both control group and treatment arms of the key ARDS trials are presented in Table 1. It appears that, many of these interventions listed in this Table were instituted at different time points and patient populations that may not be comparable. The heterogeneity in patient population and treatment effect of interventions based on timing of initiation and technique applied raise more questions (11). Are the patients included in the HFOV individual patient meta-analysis and the ones randomised to ECMO in EOLIA different? Even if that’s the case, data from a meticulously conducted randomised trial is more likely to guide clinical practice compared with an individual patient meta-analysis.
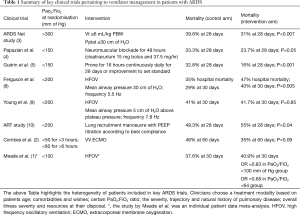
Full table
ECMO use has expanded all around the world. Equipoise for future ECMO vs. conventional ventilation trials also appears to be diminishing. It is likely that future trials in ECMO will focus mainly on testing best application of VV ECMO with adjuncts such as prone positioning. It is anticipated that, like refinements that occurred in mechanical ventilation over decades, there will be significant refinements in clinical application of ECMO. These refinements may allow further improvements in VV ECMO outcomes. In this setting, the prospects of a trial of HFOV vs. ECMO as rescue in severe ARDS will probably remain a hypothetical question. Determining the timing and threshold of randomisation to either, if such a trial were to ever occur is going to be challenging. Equally, on face value, patients randomised to ECMO in EOLIA appear to have more significant severity of disease at ECMO initiation when compared with those included in the meta-analysis. In that case, if a role for HFOV exists as the first line rescue prior to ECMO is another relevant question.
In summary, with many combinations of devices/strategies to choose from, individualising treatment to get best possible outcomes in ARDS can certainly be challenging. Can prone ventilation, HFOV and ECMO be applied in an incremental fashion in ARDS? Based on the findings of this meta-analysis, our current knowledge of ARDS management and lack of definitive evidence yet for ECMO, one cannot help but wonder—is there room to oscillate between prone ventilation and ECMO?
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Meade MO, Young D, Hanna S, et al. Severity of Hypoxemia and Effect of High-Frequency Oscillatory Ventilation in Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med 2017;196:727-33. [Crossref] [PubMed]
- Combes A, Hajage D, Capellier G, et al. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome. N Engl J Med 2018;378:1965-75. [Crossref] [PubMed]
- Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8. [Crossref] [PubMed]
- Papazian L, Forel JM, Gacouin A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 2010;363:1107-16. [Crossref] [PubMed]
- Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013;368:2159-68. [Crossref] [PubMed]
- National Heart Lung, Blood Institute Acute Respiratory Distress Syndrome Clinical Trials Network, Wiedemann HP, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 2006;354:2564-75. [Crossref] [PubMed]
- Brodie D, Bacchetta M. Extracorporeal membrane oxygenation for ARDS in adults. N Engl J Med 2011;365:1905-14. [Crossref] [PubMed]
- Ferguson ND, Cook DJ, Guyatt GH, et al. High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med 2013;368:795-805. [Crossref] [PubMed]
- Young D, Lamb SE, Shah S, et al. High-frequency oscillation for acute respiratory distress syndrome. N Engl J Med 2013;368:806-13. [Crossref] [PubMed]
- Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial Investigators, Cavalcanti AB, Suzumura EA, et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA 2017;318:1335-45. [Crossref] [PubMed]
- Matthay MA, McAuley DF, Ware LB. Clinical trials in acute respiratory distress syndrome: challenges and opportunities. Lancet Respir Med 2017;5:524-34. [Crossref] [PubMed]


