
Surgical stabilization for multiple rib fractures: whom the benefit? —a prospective observational study
Introduction
Rib fractures following blunt trauma are extremely frequent, but their potential impact on morbidity and mortality is most often underestimated. In the context of multiple trauma or extended lung contusion, rib fractures are at the backstage. Isolated rib fractures, even if multiple, are erroneously considered as a benign disorder. However, registry studies have shown that there are 2 parameters, which considerably influence mortality and morbidity of rib fractures: number of rib fractures in excess of 4, age of the patient above 45 (1). When both factors are combined, there is a significant increase of mortality and of specific complications such as pneumonia. Further, in patients older than 60 years dying after isolated blunt chest trauma, 55% had no more than multiple rib fractures (2).
The deleterious effect of multiple rib fractures is easily explained by pain and instability of the chest wall, which both lead to poor ventilation and inefficient cough. The main consequences are retention of secretion, followed by pneumonia and respiratory distress, and eventually fatal outcome.
Simple common sense suggests that surgical fixation of multiple fractures might improve outcomes (3). Stabilizing the chest wall will reduce pain, and improve respiratory dynamics, efficacy of cough, and clearance of secretions, and hence lower mortality and morbidity associated to multiple rib fractures. Economic outcome parameters such as duration of ICU stay and hospital stay, as well as duration of professional inability, should be shortened (4,5).
Management of fail chest and multiple rib fractures has gone through opposite time trends. During the 60ies and 70ies, chest wall trauma was treated first-hand by thoracic surgeons, and surgical fixation was quite popular in those years. The alternative treatment was application of external traction to the flail chest wall segment (6,7). With improving equipment and skills in intensive care units, patients with flail chest progressively escaped from the surgeon, as it was estimated that internal pneumatic ventilation achieves reliable stabilisation, and spares a surgical intervention to the patient (8). Finally, during the past few years, surgery is coming back to focus. Above all, the social cost of the treatment is to be reconsidered; we may hypothesize that recovery is quicker and that the complication rate is reduced with surgical management compared to conservative treatment based on prolonged intubation with deep sedation and mechanical ventilation (5). Besides, surgical tools have improved and allow for easier, more expeditive, and more reliable reconstructions.
While some evidence emerged from various observational studies, we can now rely on at least 3 randomized studies and 2 meta-analyses (9-13). Tanaka et al. randomized 37 patients with flail chest after 5 days of artificial ventilation and allocated them to 2 groups, consisting either of surgical repair or of conservative management. In the surgical arm, there was a significant reduction of ICU stay, duration of ventilation, duration of hospital-stay. There was a significant decrease of complications such as pneumonia or need for tracheostomy. At 6 month and 1 year, patients having undergone surgical repair had significantly better spirometry parameters, significantly less disabling symptoms, and a significantly higher proportion had resumed with normal activity. The social benefit of surgical repair was estimated 10,000$, owing to shorter ICU stay (9). Granetzny et al. randomized 40 patients with flail chest after isolated chest trauma between surgical fixation and conservative management. The authors concluded to a dramatic and highly significant decrease of duration of post-operative ventilation, ICU stay and global hospital stay (10). Further, functional parameters tested at 2 months showed significantly higher values in the surgical arm. Marasco et al. randomized 46 patients with flail chest who could not be weaned off the ventilator 48 hours after admission (11). Again, the surgical group showed quicker recovery and marked decrease of ICU stay and global hospital stay; need for tracheostomy was significantly lower (11). Cost of treatment was decreased by 14,000$ per patient in the surgical arm. The 3 randomized studies and a panel of case-control studies were included into 2 meta-analyses, summing up more than 500 patient records (12,13). Both conclude to a significant decrease of post-operative ventilator dependence (gain of 4.5 and 7.5 days), ICU stay (gain of 3.4 and 4.8 days) and hospital stay (gain of 3.8 and 4 days). They both demonstrate a decrease of mortality (OR 0.31 and 0.43) and pneumonia (OR 0.18 and 0.45). At medium term, symptoms such as dyspnoea and chest pain are decreased (OR 0.40), and there is less deformity (OR 0.11) after surgical stabilisation.
While 2 clinical studies estimated that the gain per patient obtained with surgical repair could be 10,000–14,000$, a theoretic simulation study with construction of a Markov transition state model was less optimistic (9,11). The hypothesis was set up with the example of a young adult suffering from isolated chest trauma (5). The risk for various complications was estimated on available publications and registry data. In conclusion, the authors estimated that surgical stabilisation reduces the cost of initial treatment by 1,541$.
We addressed the question whether surgery is useful in non-flail multiple rib fractures and reviewed available literature with an EBM methodology (14). We came to the conclusion that treatment time is shorter and complication rate is lower after surgical stabilisation of non-flail multiple rib fractures (14). The recent publication by Pieracci et al., comparing medical and surgical management of severe chest wall trauma in 2 subsequent 1-year period for each, came to the same conclusion; the authors included not only flail chest, but also extended rib fractures with deformity or poor pain control (15).
Based on available evidence in 2010, we set up an institutional consensus conference in June 2010, where we decided to discuss surgical fixation in any patient admitted with 4 or more rib fractures and/or older than 45 years, without anticipated need for prolonged mechanical ventilation such as severe brain injury or extended lung contusion. We hypothesized that patients extubated in less than 24 hours would have maximal benefit. This article was designed to check our hypothesis and to identify factors predicting early extubation.
Methods
Following an institutional consensus conference run in June 2010, we decided to discuss indication of surgical fixation of multiple rib fractures in any patient older than 45 years and/or with more than 4 rib fractures with the senior thoracic surgeon on call.
All operated patients following this consensus were entered into a prospective cohort database and were informed accordingly. Follow-up of the patients was maintained until discharge of the patients. The study has been submitted to the Ethical Committee of the French Society for Thoracic and Cardiovascular Surgery (registration number: 2017-1-9-21-46-30-OlAn).
Surgical indications
Surgical fixation was indicated in case of flail chest, marked deformity, or multiple fractures with poor pain control. Fixation was also considered in patients in whom there was an indication for thoracotomy for associated lesions.
In case of multiple trauma, indication for rib fixation and prioritisation of the different operations was discussed in a multidisciplinary fashion. Obviously, surgery was not considered in patients in whom prolonged mechanical ventilation was anticipated because of extensive lung contusion, TRALI or ARDS, and patients with severe cranio-cerebral trauma.
Surgery was only considered during the 1st week after trauma.
Technical considerations
Operations were conducted under general anesthesia with single lumen intubation. The patient was positioned in a lateral thoracotomy position.
The skin and soft-tissue incision was designed in 2 ways: for limited and grouped fractures, a muscle-splitting approach was applied; in presence of extended fractures, we used a large posterolateral approach, with the most peripheral possible division of the latissimus dorsi muscle, in order to preserve its vascularisation and innervation. We always strived to preserve the serratus anterior muscle. Next, the pleural cavity was inspected through a frank incision of the 5th or 6th intercostal space: any residual hemothorax was cleared; careful inspection screened for any additional intrathoracic injury. After revision of the pleural cavity, and before starting osteosynthesis, we inserted two 24 Fr chest tubes.
Our choice for osteosynthesis was the STRACOS/STRATOS system commercialized by MedXpert (Eschbach, FRG). The latter is based on titanium clips, which may be used alone (pink STRACOS clips) or in combination with extracostal struts (STRATOS, yellow straight clips and blue angulated clips). The clips can be moulded in 3 dimensions and perfectly fit to each individual situation. There is no need for deperiostation. Oblique fractures and 3rd fragments/loss of substance are not a problem and can easily be bridged. Limitations for its use are fractures located close to the spine or close to the sternum.
Fixation should address in priority those ribs with diaphragmatic insertions, i.e., 6–10. Ribs N° 11 and 12 do not need repair. Similarly, ribs N° 1–3 do not play a significant role in respiratory dynamics, and require a traumatic incision to be reached.
We do not need to exhaustively fix all ribs; the aim of surgery is to leave the patient with a stable chest wall. Stability may easily be tested by manual pressure during the operation.
Data collection
For each operated patient, following information and acceptance from the patient, we recorded demographic data, prior medical history, the number of fractures, and the associated traumatisms.
Regarding the surgical technique, we recorded the number of clips used for each patient, if needed the use of struts, the type of incision, if possible, the use of video-assisted technique.
As for the outcomes, the ICU and hospital stay, the postoperative delay for extubation and mechanical ventilation weaning, and the postoperative complications were recorded. We especially focused on the onset of pneumonia.
Endpoints
Our primary end-point was to compare outcome of patients who were extubated within 24 hours to those who required mechanical ventilation for more than 24 hours post-operatively. Our secondary endpoint was to determine factors predicting need for prolonged mechanical ventilation post-operatively.
Statistical analysis
Discrete variables were expressed as counts and percentages and continuous variables as mean and standard deviation, unless otherwise stated. Comparison between patients extubated within 24 hours and patients with mechanical ventilation longer than 24 hours were performed using the Chi-squared test and t-test for qualitative and quantitative data, respectively.
Predictive factors of mechanical ventilation greater than 24 hours were computed using logistic regression. The same method was used to determine predictive factors of patients undergo pneumonia and other complications. Variables with a significance level inferior at 0.2 were included in a stepwise logistic model. We have retained in the final model the variables whose significance level was less than 0.05. Model discrimination was assessed by the c-index and model calibration by the Hosmer-Lemeshow goodness-of fit statistics. All analyses were performed using SAS (version 9.3; SAS institute, Inc., Cary, NC, USA)
Results
Overall results and risk factors for post-operative complications
From July 1st, 2010 to March 31st, 2015, we recorded 132 patients who underwent thoracic osteosynthesis.
Preoperative demographic and medical data are summarized in Table 1. Mean age at the time of surgery was 60 (15.2) years. Patients presented with a mean number of 11 (5.2) fractures and 63% had flail chest. Prior to surgery, 28% of patients had active tobacco consumption at the time of traumatism, 12% had chronic obstructive pulmonary disease (COPD), 12% had a prior cardiac disease, and 15% had prior chronic atrial fibrillation. The overall mean duration of mechanical ventilation was 3.6 (6.9) days.
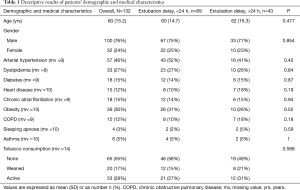
Full table
Thirty percent of patients developed pneumonia. Besides, 8% had urological complications, 6% had digestive complications, and 3.8% had heart complications. Five (3.8%) patients died in the post-operative period: three patient died from acute respiratory distress related to pneumonia, one patient died from massive bleeding due to an aortic arch rupture, and one patient died from multivisceral failure. Four patients were aged over 80 years and chest trauma was associated with abdominal and head trauma.
On univariate analysis, we found bilateral rib fractures and lung contusion prior to thoracic repair were significantly associated to the development of pneumonia in the post-operative course.
On multivariate analysis, independent risk factors for pneumonia were age over 70 years, and patients with active tobacco consumption. Both factors significantly increased the risk in a 5-fold manner. Prior medical history of heart disease, bilateral rib fractures, and lung contusion demonstrated a trend (P<0.1 in multivariate analysis) to risk factor participating in increasing the occurrence of post-operative pneumonia.
Overall outcomes after thoracic repair are summarized in Table 2.

Full table
Risk factors for pneumonia are summarized in Table 3.
Full table
Primary endpoint: outcome of patients extubated within 24 h following surgery
In a consecutive series of 132 patients with multiple rib fractures, more than two thirds (n=89; 67%) were extubated within 24 hours following surgical stabilization. In these patients, mean duration for mechanical ventilation was 2 (6) hours. Forty-three (33%) patients could not be extubated in the immediate post-operative course and were ventilated more than 24 hours following thoracic repair. In those patients, mean duration of mechanical ventilation was 11 (8.3) days and the median time to extubation was 8 days.
Patients with prolonged mechanical ventilation (over 24 hours) had significantly longer ICU stay and longer in-hospital stay (P<0.0001 both). Pneumonia occurred significantly more often in those patients (P<0.0001) and the overall post-operative complications rate was higher (P=0.0001). Four patients died in the group with prolonged mechanical ventilation.
Outcome for patients ventilated more than 24 hours are summarized in Table 2.
Secondary end-points: risk factors for prolonged mechanical ventilation (over 24 hours)
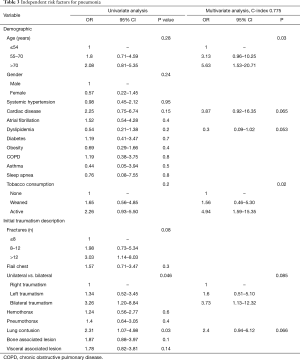
Univariate analysis identified the following risk factors: higher number of fractures, especially bilateral; other associated bone lesions (including cranial and pelvis bone fractures). There was no significant difference for the 24 hours extubation delay in patients with associated visceral lesions, as well as for patients with pulmonary contusion, hemothorax, or pneumothorax.
On multivariate analysis, bilateral rib fractures and pneumothorax at the time of initial traumatism were found to be significant independent risk factor for prolonged mechanical ventilation (>24 hours). In addition, cardiac comorbidity and number of fractures exceeding 12 predicted a more than a 4-fold increase in the risk for delayed extubation. Risk factors for delayed extubation over 24 hours are summarized in Table 4.

Full table
Discussion
In this study, we considered surgical stabilization for patients with flail chest or non-flail multiple rib fractures. Following surgical repair, two thirds of our patients were extubated within 24 hours. Mechanical ventilator support over 24 hours was associated with higher post-operative complications rate (including pneumonia), leading to longer ICU and hospital stay. Independent significant risk factors for delayed extubation and prolonged mechanical support (>24 h) were related with the initial extent of trauma: bilateral rib fractures, bone fractures of the limbs, and chest trauma presenting with initial pneumothorax.
There is a bulk of evidence, consisting of several observational studies, at least 3 randomized trials and 2 meta-analyses, supporting the advantages of surgical stabilizations of post-traumatic flail chest. In our series, we accrued 83 patients with flail chest (63%). Similarly to Pieracci and colleagues, we also elected patients with non-flail multiple chest fractures in case of severe deformity, or poor pain control, or need for thoracotomy for associated lesions (15). Severe deformity may be defined as an impaction leading to a loss of volume exceeding 30% in a hemithorax. Poor pain control means that the patients’ active mobilization is impeded by persistent pain despite optimized medical treatment with use of morphine mimetics and non-steroid anti-inflammatory drugs. Locoregional pain relieve with paravertebral blockade or epidural analgesia is ambiguous in the sense that it cannot be used over a prolonged period; on the other hand, rib fractures are still unstable and painful 4–6 days after initial trauma. Though we lack of randomized trials in the latter 2 categories, we retrieve evidence from non-randomized observational studies. Further, Pieracci and colleagues have used a staged approach, accruing patients for medical treatment during one year, and accruing patients with the same pattern of chest traumatism to routine surgical stabilization during the following year (15). Both groups (medical treatment versus surgical stabilization) were compared on the same outcomes: respiratory failure, tracheostomy, pneumonia, ventilator days, tracheostomy, length of stay, daily maximum incentive spirometer volume, narcotic requirements, and mortality. Surgical stabilization enabled a significant improvement in acute outcomes in these severely injured patients (15).
Finally, an evidence-based approach published in the “best bet” series concluded to an advantage of surgical stabilization in non-flail multiple fractures (14). In this context, we should remind the spontaneous risk for respiratory complications and even mortality in patients over 45, suffering from more than 4 rib fractures (1). On hand of these arguments, we cannot agree with the conclusion of a Cochrane meta-analysis, stating that we lack of randomized studies to evaluate the true benefits of surgical thoracic repair (16).
Only few reports address the issue of material or implants used for osteosynthesis. Obviously, simple sutures or encircling wires do not guarantee stability, and intracostal pins and struts are insufficiently stable and prone to migration with its inherent risks (17-20). There is actually competition between 2 reliable designs. A first concept is derived from the time-honored principle of plate & screw osteosynthesis, as it is used on limbs and mandible (21). Metal rib clips, initially designed by Judet in the 1970ies, represent an alternative (18,22). To our opinion, plate and screw osteosynthesis may appear logical for repair of one or 2 bones as for instance in a forearm fracture, but is lengthy and tedious when there is a need to fix several rib fractures. There is a need for many ancillary instruments, and a generous stock of screws of different sizes. In addition, there may be technical problems in case of complex fractures or 3rd fragments, or osteoporosis. As most surgeons would prefer titanium implants because of its excellent biological tolerance, the cost of material needs to be considered as well. We decided for clip osteosynthesis, mainly because it is more expeditious; gain of operating time may partly compensate the cost of the implant. More recently, nitinol implants have become available; they offer the same advantage in terms of tolerance; in addition, elasticity with memory of shape guarantees a dynamic osteosynthesis. Other potential advantages of clip osteosynthesis are the relatively few incontournable ancillaries. We also anticipate improved hemostasis and limited oozing due to optimal impaction and compression of the fractured segments.
Our study highlights that benefit of the surgical stabilization concerns mainly patients who had been extubated within 24 hours after repair. As previously mentioned, decision to operate was made after multidisciplinary discussion, and one of the key arguments in favor of repair was the assumption that the patient might be weaned shortly thereafter. In other terms, patients with severe brain trauma, extended lung contusion, and extended visceral trauma were not considered for surgical stabilization of rib fractures. It appears that peripheral bone fractures and bilateral rib fractures were associated with a need for prolonged mechanical ventilation, and with an increased risk for morbidity. The latter must be considered as surrogate marker of severity of trauma, even in absence of significant brain or visceral injuries. Surprisingly, neither cardio-respiratory comorbidities nor active smoking had any impact on the delay of extubation. We may hypothesize that surgical repair might have a protective effect in such fragilized patients, because surgical stabilization will favor relief of pain, efficacy of clearance of bronchial secretions, and earlier mobilization. Concurrently, Athanassiadi et al. demonstrated that the most reliable predictor of outcome for flail chest was the injury severity score which corroborates our findings on peripheral bones fractures and bilateral rib fractures as risk factors for increased morbidity (23). In their study, Athanassiadi et al. studied the outcome of 250 patients with flail chest according to the ISS score; patients were only treated with the best medical care. Osteosynthesis is not described and thoracotomy was performed only in case of associated mediastinal or lung associated injury. The ISS demonstrated to be significantly predictive of the outcome of patients (23). With our results we may extend the value as prognostic factor of associated lesions even in non-flail chest patients and in patients undergoing surgical stabilization.
Nevertheless, given the results of our study, extended trauma as a risk factor for prolonged mechanical ventilation should not be considered as a contraindication for surgical repair. Even in that group of patients, mean ventilation duration was 11 days and the mean ICU stay was 16 days which is shorter than the prior classical 3 weeks of pneumatic stabilization. The design of our study was able to define the group of patient who will mostly benefit from surgical stabilization. Further studies are needed to define whether surgical stabilization still represents an advantage for patients with extended trauma in comparison to other treatments. However, it is a well-known fact that most surgical randomized trials suffer from low patient accrual. Further, it may be problematic to obtain an informed consent from a patient or his relatives in the context of painful major chest wall trauma. Given the available evidence, we consider that surgical repair is an ethically sound option.
Conclusions
In conclusion, our study adds to the existing evidence that osteosynthesis is beneficial to patients with multiple rib fractures, including non-flail chest. Patients who may be extubated within 24 hours obtain maximal benefit. Extended trauma, but not comorbidities, is an indicator of need for prolonged ventilation, which questions the utility of surgical repair of the chest wall in such patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study has been submitted to the Ethical Committee of the French Society for Thoracic and Cardiovascular Surgery (registration number: 2017-1-9-21-46-30-OlAn).
References
- Holcomb JB, McMullin NR, Kozar RA, et al. Morbidity from rib fractures increases after age 45. J Am Coll Surg 2003;196:549-55. [Crossref] [PubMed]
- Kent R, Woods W, Bostrom O. Fatality risk and the presence of rib fractures. Ann Adv Automot Med 2008;52:73-82. [PubMed]
- Coleman FP, Coleman CL. Fracture of ribs; a logical treatment. Surg Gynecol Obstet 1950;90:129-34. [PubMed]
- Fitzpatrick DC, Denard PJ, Phelan D, et al. Operative stabilization of flail chest injuries: review of literature and fixation options. Eur J Trauma Emerg Surg 2010;36:427-33. [Crossref] [PubMed]
- Bhatnagar A, Mayberry J, Nirula R. Rib fracture fixation for flail chest: what is the benefit? J Am Coll Surg 2012;215:201-5. [Crossref] [PubMed]
- Cohen EA. Treatment of the flail chest by towel clip traction. Am J Surg 1955;90:517-21. [Crossref] [PubMed]
- Hudson TR, McElvenny RT, Head JR. Chest wall stabilization by soft tissue traction: a new method. J Am Med Assoc 1954;156:768-9. [Crossref] [PubMed]
- Avery EE, Benson DW, Morch ET. Critically crushed chests; a new method of treatment with continuous mechanical hyperventilation to produce alkalotic apnea and internal pneumatic stabilization. J Thorac Surg 1956;32:291-311. [PubMed]
- Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002;52:727-32; discussion 732. [Crossref] [PubMed]
- Granetzny A, Abd El-Aal M, Emam E, et al. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg 2005;4:583-7. [Crossref] [PubMed]
- Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg 2013;216:924-32. [Crossref] [PubMed]
- Leinicke JA, Elmore L, Freeman BD, et al. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg 2013;258:914-21. [Crossref] [PubMed]
- Slobogean GP, MacPherson CA, Sun T, et al. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg 2013;216:302-11.e1. [Crossref] [PubMed]
- Girsowicz E, Falcoz PE, Santelmo N, et al. Does surgical stabilization improve outcomes in patients with isolated multiple distracted and painful non-flail rib fractures? Interact Cardiovasc Thorac Surg 2012;14:312-5. [Crossref] [PubMed]
- Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg 2016;80:187-94. [Crossref] [PubMed]
- Cataneo AJ, Cataneo DC, de Oliveira FH, et al. Surgical versus nonsurgical interventions for flail chest. Cochrane Database Syst Rev 2015.CD009919. [PubMed]
- Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. J Thorac Cardiovasc Surg 1995;110:1676-80. [Crossref] [PubMed]
- Menard A, Testart J, Philippe JM, et al. Treatment of flail chest with Judet’s struts. J Thorac Cardiovasc Surg 1983;86:300-5. [PubMed]
- Albrecht F, Brug E. Stabilization of the flail chest with tension band wires of ribs and sternum. Zentralbl Chir 1979;104:770-6. [PubMed]
- Shah TJ. On internal fixation for flail chest. J Thorac Cardiovasc Surg 1996;112:849-50. [Crossref] [PubMed]
- Bottlang M, Helzel I, Long WB, et al. Anatomically contoured plates for fixation of rib fractures. J Trauma 2010;68:611-5. [Crossref] [PubMed]
- Judet R. Costal osteosynthesis. Rev Chir Orthop Reparatrice Appar Mot 1973;59 Suppl 1:334-5. [PubMed]
- Athanassiadi K, Theakos N, Kalantzi N, et al. Prognostic factors in flail-chest patients. Eur J Cardiothorac Surg 2010;38:466-71. [Crossref] [PubMed]


