
Effect of patient position during virtual-assisted lung mapping
Introduction
Virtual-assisted lung mapping (VAL-MAP) is a bronchoscopic technique in which multiple lung markings are made with the aid of virtual bronchoscopy to facilitate surgical resection of pulmonary nodules that seem impalpable and unidentifiable (1-5). VAL-MAP is approved by public health insurance in Japan, and may replace the computed tomography (CT)-guided percutaneous needle-mediated lung marking technique, which reportedly causes relatively high incidences of multiple complications (6). VAL-MAP has been widely performed in Japan, and a recent multicenter study confirmed the safety and reproducibility of VAL-MAP (5).
Although VAL-MAP is safe and effective, it does have some limitations. Marking failure reportedly occurs in approximately 10% of markings, although the lung map as a whole may still function appropriately even with the failure of one marking among multiple markings (5). Moreover, pneumothorax occurs in about 4% of cases (3,5). Previous studies have suggested that the quality of the markings may partially depend on the operator’s skill level (5,7). The success rate of markings must be increased to improve the quality of the VAL-MAP procedure.
No study has investigated the effect of patient positioning during the VAL-MAP procedure on the quality of markings, although expert opinion suggests that the lateral position might be better for marking the dorsal and ventral parts of the lung (such as the right middle lobe and the left lingular segment) (8,9). This assumption is based on the gravity effect, which would tend to make the dorsal part of the lungs collapse when the patient is in supine position, thus making it challenging to perform the dye injection. In addition, the supine position would create difficulty in injecting the right middle or left lingular segments, as the injected dye would tend to flow backward due to gravity. However, if patients were in lateral position with the marking side up during dye injection, gravity would have minimal negative impact on the quality of markings.
The purpose of the present study was to investigate whether patient positioning during dye injection in the VAL-MAP procedure affects the success rate and the quality of markings in VAL-MAP.
Methods
Patients
The present study included patients who underwent pulmonary wedge resection or segmentectomy using VAL-MAP from December 2016 to September 2017 in NTT Medical Center Tokyo. The inclusion and exclusion criteria for VAL-MAP are shown in Table 1. There was a two-step procedure for patient registration for application of VAL-MAP. Primary registration was completed if the patient satisfied inclusion criteria I to III, and did not meet the exclusion criteria; secondary registration was then completed once the case review committee approved and confirmed the fulfillment of the criteria.

Full table
Patients provided informed consent before being enrolled to undergo VAL-MAP in one of two prospective multi-center studies, either UMIN 000022991 (before June 2017) or UMIN 000008031 (after July 2017); these two studies were approved by the Ethics Committee of NTT Medical Center Tokyo (approval numbers 16-566 and 17-373, respectively). The patient data from these two studies was retrospectively analyzed in the present study, which was approved by the approval of the Ethics Committee of NTT Medical Center Tokyo (approval number 18-174).
VAL-MAP procedure
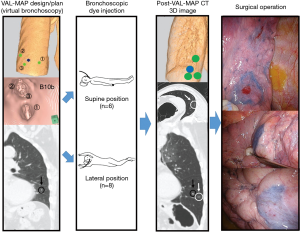
The mapping procedures were conducted as shown in Figure 1. One day before surgery, the patient was sent to the bronchoscopy suite for the creation of markings under local anesthesia and mild sedation. Dye markings were performed as reported previously (1-3,7). After the application of local anesthesia, a metal-tipped catheter (PW-6C-1; Olympus, Tokyo, Japan) was inserted through the working channel of the bronchoscope into the target bronchus under the guidance of virtual bronchoscopic imaging. The catheter tip was confirmed to have reached the visceral pleura using X-ray fluoroscopy (Ultimax-i; Canon Medical Systems Ltd., Japan). After confirming the location of the catheter tip, the patient was placed in supine or lateral position with the marking side up. The patient was maintained in the same position while the indigo carmine dye was injected. This process was repeated for all targeted bronchi. After the dye injections, chest CT was conducted in lateral position with the marking side up to confirm the actual locations of the markings and the target nodules. The post-VAL-MAP CT images were reconstructed into three-dimensional (3D) images for the surgical procedure.
The lateral position was defined as a decubitus position with the marking side up. During the VAL-MAP dye injections, all patients were maintained in fixed position, either supine or lateral. The initial five patients were in the supine position during the procedure, while the procedure was performed with the patient in the lateral position from the sixth patient to the 13th patient. The 14th patient needed to be in the supine position throughout the procedure to enable temporal ventilation assistance because the sedation introduced before bronchoscopy was so deep that the patient manifested temporal hypopnea at the very beginning of the procedure. We did not change the supine position of the 14th patient for the patient’s safety.
In this series, we did not notice any remarkable differences regarding peripheral oxygen saturation between patients with lateral position and those with supine position.
Grading of markings and definition of appropriate markings
The primary endpoint was quality of marking in this study. The quality of each marking was evaluated using a previously reported grading system as grade 0 (unidentifiable), grade 1 (identifiable, but faint), grade 2 (easily identifiable without a central red spot or target-like shape), grade 3 (easily identifiable with a central red spot), grade 4 (target-like appearance with or without a central red spot), or grade 5 (bulla formation) (3). Markings graded 2–4 were defined as “appropriate”, whereas those graded 0, 1, or 5 were defined as “inappropriate”.
We calculated and compared the rates of appropriate markings in the supine and lateral positions among the whole cohort. We also did the same analysis among the markings located in right S2/S4/S5/S6/S9/S10 and left S1+2/S4/S5/S6/S9/S10, as it is considered difficult to create appropriate markings in these locations (8,9).
Cumulative rate of appropriate markings
We estimated the cumulative rate of appropriate markings in accordance with the cumulative number of markings in order to show the effect of the learning curve, and created a plot via curve fitting. We excluded markings that could not be evaluated because of severe adhesion. Adhesiolysis would have enabled the evaluation of such markings; however, this was not done, as it would have caused lung injury.
Evaluation of the surgical procedure
Surgical success was defined as resection of the lesion with margins larger than or equal to the lesion diameter or 2 cm in accordance with the initial planned resection. If the resection margins were insufficient and additional resection was conducted, the resection was defined as a failure.
Data acquisition and analysis
We recorded the patient age, sex, number of lesions per patient, lesion sizes, tumor depth (distance between the closest pleura and the tumor), characteristics of the lesions on CT, planned and performed surgical procedures, grade of each marking, result of the surgical procedure (success or failure), pathological diagnoses, and complications within 30 days postoperatively.
The patient ages were described as the median (range). The number of markings per patient, and the size and depth of the lesions were described as the mean ± SD (range). We compared the number of markings per patient and the size and depth of the lesions in different positions using the Student’s t-test. Comparisons of appropriate markings rates between groups were conducted using the Fisher exact test. To assess the factors associated with appropriate markings, logistic regression analyses were conducted, considering patient position, marking locations, and the learning curve effect. We divided the marking locations into two groups: dorsal or ventral segments (right S2/S4/S5/S6/S9/S10 or left S1+2/S4/S5/S6/S9/S10), and others. We also divided the study period into two periods: early phase (from the first patient to the median patient), and late phase (from the median patient to the last patient).
All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan, 2012) (10). P<0.05 was considered to indicate a statistically significant difference.
Results
Patients, targeted lesions, and planned procedures
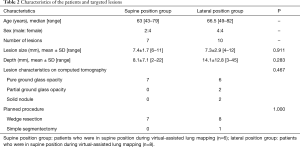
A total of 14 patients with 17 lesions underwent VAL-MAP, including six patients with six lesions who underwent VAL-MAP in supine position (supine position group), and eight patients with 10 lesions who underwent VAL-MAP in lateral position with the marking side up (lateral position group). To resect all 17 lesions, a total of 48 markings were planned. The markings were all performed as planned (3.4±0.9 markings per patient). The patient characteristics, targeted lesions, and planned procedures are shown in Table 2. There were no significant differences between the supine and lateral position groups regarding lesion size, depth, and characteristics on CT. Almost all of the planned procedures were thoracoscopic wedge resections (94%), while one procedure was a thoracoscopic left upper division segmentectomy.
Full table
Marking quality
The number of markings, evaluated markings, and performed procedures are shown in Table 3. In the lateral position group, one marking was not evaluated intraoperatively because of severe adhesion.

Full table
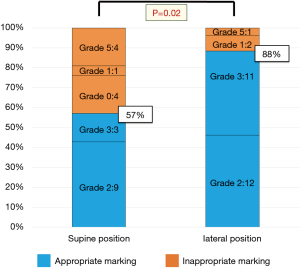
Figure 2 shows the quality of the markings and the rates of appropriate and inappropriate markings in both patient positions. The appropriate markings rate was significantly greater in the lateral position group (88%; 23 of 26) than in the supine position group (57%; 12 of 21; P=0.02).
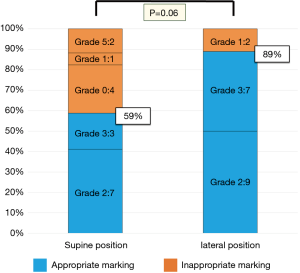
To explore the mechanism whereby the positional difference affected the quality of markings, we examined the effect of marking location. It has been suggested that the effect of gravity in the supine position makes it difficult to perform markings in the dorsal segments such as S6, S9, and S10, right S2, and left S1+2, and in the ventral segments in the right middle lobe and left lingular segments (9). Figure 3 shows the quality of the markings and the rates of appropriate and inappropriate markings located in the dorsal and ventral segments. The appropriate markings rate in the dorsal and ventral segments in the lateral position group (89%; 16 of 18) tended to be greater than that in the supine position group (59%; 10 of 17); however, this difference was not significant (P=0.06). There were too few markings made in segments other than the ventral and dorsal segments to examine the effect of patient position on the quality of markings.
Cumulative rate of appropriate markings
The plot of the cumulative rate of appropriate markings is shown in Figure 4. We performed the first 15 markings with the patients in supine position, the 16th to 41st markings with the patients in lateral position, and the last six markings with the patient in supine position.
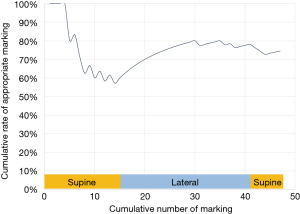
Figure 4 suggests that the cumulative appropriate markings rate increased when marking was performed with the patient in lateral position. Notably, even though the technique may have improved over time with the accumulation of experience, some of the final six markings performed with the patient in supine position were still inappropriate.
Surgical outcomes, final pathological diagnoses, and complications
The success rate of the surgical procedure was 78% in the lateral position group, and 100% in the supine position group (P=0.48). In the lateral position group, two lesions in two patients required additional wedge resections due to insufficient surgical margins in the initial wedge resection. Except for these two resections, there were no conversions of surgical procedures.
The final pathological diagnoses are shown in Table 3. Most of the tumors were adenocarcinoma (76%). There were no significant differences between groups in pathological diagnoses.
Complications associated with VAL-MAP were seen in two cases, including one case in the supine position group and one in the lateral position group. Both were minor pneumothorax that did not require chest tube drainage.
Multivariate logistic regression analyses to identify predictive factors for appropriate markings
As mentioned above, we assumed that the dorsal or ventral segments (right S2/S4/S5/S6/S9/S10 or left S1+2/S4/S5/S6/S9/S10) might be associated with inappropriate markings. We also assumed that the procedures performed in the early phase would be associated with a greater rate of inappropriate markings compared with the late phase due to the learning curve effect.
Multivariate regression analysis revealed that the lateral position was significantly associated with appropriate markings (P=0.014; Table 4). When the analysis was restricted to the markings located in the dorsal and ventral segments, the lateral position still remained significantly associated with appropriate markings (P=0.047; Table 5). The occurrence of inappropriate markings was not significantly associated with marking in the dorsal or ventral segments or procedures conducted in the early phase of the present study.

Full table

Full table
Discussion
The concept of our study was based on the hypothesis that performing the dye injection in VAL-MAP with the patient in the lateral position achieves good markings by avoiding the unfavorable effect of gravity (8,9). The present study demonstrated a significant difference in the quality of markings performed in the lateral versus supine position, and suggests that the lateral position is more favorable for achieving good quality markings in VAL-MAP (Figure 2).
Although no study has focused on the effect of patient positioning during the dye injection on the quality of markings in VAL-MAP, it has been suggested that the lateral position results in better outcomes. Two studies recommend that patients should be placed in lateral position with the marking side up for marking in the dorsal portion of the lung (8,9). This recommendation is based on the assumption that the lateral position with the marking side up would help to inflate the posterior region of the lung, which tends to be collapsed in supine position (11). Theoretically, collapsed lungs have greater resistance to dye injection, resulting in “central injection” (dye injection that does not reach the peripheral lung tissue and the pleura) or forceful injection that may lead to bulla formation and/or pneumothorax (1,9). In addition, one study suggested that the lateral position is also preferable for dye injection into the ventral portions of the lung (such as the right middle lobe or left lingular segment), as dye injected against gravity tends to flow backward rather than being successfully sprayed on the pleura (9). Thus, placing the patient in lateral position may avoid these unfavorable effects of gravity in the supine position. Indeed, in the present study, markings made in the dorsal and ventral regions of the lung tended to be of better quality when created with the patient in the lateral position rather than in the supine position (Figure 3, Table 5).
Although we could not examine the details of markings placed in regions other than the dorsal and ventral segments due to the limited number of markings, the lateral position may be favorable for all markings in VAL-MAP for the following two reasons. First, it may be easier to accurately locate the catheter tip with the patient in the lateral position rather than the supine position. In the present series, we confirmed the catheter tip location using X-ray fluoroscopy with C-arm equipment. With the patient in the supine position, the range of movement of the C-arm was limited to 131° (right anterior oblique 90°, left anterior oblique 41°), resulting in insufficient visualization of the catheter tip at some angles. Moreover, the patients’ upper extremities sometimes obstructed the X-ray and thus hindered visualization. In contrast, patients in the lateral position were able to be rotated anterolaterally or posterolaterally to achieve optimal visualization of the catheter tip; furthermore, if a patient’s upper extremity was obstructing the X-ray, it was easily mobilized outside of the field (Figure 1).
Second, the lateral position may enable the inflation of parts of the lung other than the dorsal part. As mentioned above, collapsed lung tissue may theoretically make dye injection difficult due to strong resistance during injection. In our VAL-MAP procedure, post-mapping CT is routinely performed with the patient in the lateral position (Figure 1). In general, this lateral position produces superior inflation of the marked side compared with an image taken in the supine position. Furthermore, other regions of the lung may also be better inflated in the lateral position. Thus, there may be multiple favorable effects of lateral positioning on the outcome of dye markings.
It seemed contradictory that, despite better quality of markings in the lateral position group, it showed 78% of success rate of the surgical resection while the supine position group did 100%. This discrepancy between the surgical success and success in marking is considered to be not due to marking quality, but to the depth of the necessary resection margins as reported recently (12). Indeed, in the two cases in which surgical procedures failed in the lateral position group, failure was attributed not to the poor quality of making but to the depth of the lesion and associated with surgical technique. We were actually able to identify the locations of nodules in the two cases thanks to good quality of markings.
Our study has several limitations. First, it was a retrospective analysis, and the patients’ positions were not randomized. Second, the result may be biased by the learning curve effect, as the procedure tended to be performed with the patient in the supine position in the early phase, whereas the lateral position was used in the late phase. Notably, however, the last markings made with the final patient in the supine position showed relatively poor outcomes (Figure 4). Moreover, the multivariate analyses including learning curve effect supported the favorable effect of lateral positioning (Tables 4,5). Third, there was a relatively small sample size, and the data was collected from a single institution. The effect of patient positioning during VAL-MAP must be confirmed in larger, prospective, multicenter studies.
Conclusions
In conclusion, placing patients in the lateral position during dye injection in VAL-MAP may enable the creation of better markings compared with the supine position.
Acknowledgements
We thank Dr. Kelly Zammit, BVSc, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Committee of NTT Medical Center Tokyo (approval number, 18-174), and written informed consent was obtained from all patients.
References
- Sato M, Omasa M, Chen F, et al. Use of virtual assisted lung mapping (VAL-MAP), a bronchoscopic multispot dye-marking technique using virtual images, for precise navigation of thoracoscopic sublobar lung resection. J Thorac Cardiovasc Surg 2014;147:1813-9. [Crossref] [PubMed]
- Sato M, Aoyama A, Yamada T, et al. Thoracoscopic wedge lung resection using virtual-assisted lung mapping. Asian Cardiovasc Thorac Ann 2015;23:46-54. [Crossref] [PubMed]
- Sato M, Yamada T, Menju T, et al. Virtual-assisted lung mapping: outcome of 100 consecutive cases in a single institute. Eur J Cardiothorac Surg 2015;47:e131-9. [Crossref] [PubMed]
- Nakao K, Sato M, Nitadori JI, et al. Bilateral segmentectomies using virtual-assisted lung mapping (VAL-MAP) for metastatic lung tumors. Surg Case Rep 2017;3:104. [Crossref] [PubMed]
- Sato M, Kuwata T, Yamanashi K, et al. Safety and reproducibility of virtual-assisted lung mapping: a multicentre study in Japan. Eur J Cardiothorac Surg 2017;51:861-8. [PubMed]
- Ichinose J, Kohno T, Fujimori S, et al. Efficacy and complications of computed tomography-guided hook wire localization. Ann Thorac Surg 2013;96:1203-8. [Crossref] [PubMed]
- Yamanashi K, Sato M, Marumo S, et al. Emphysematous lungs do not affect visibility of virtual-assisted lung mapping. Asian Cardiovasc Thorac Ann 2016;24:152-7. [Crossref] [PubMed]
- Sato M. Virtual assisted lung mapping: navigational thoracoscopic lung resection. Cancer Res Front 2016;2:85-104. [Crossref]
- Izumo T, Sato M. Kasou-Kikanshikyo Sakusei Manual. Tokyo: Igaku-Shoin, 2017: 110.
- Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 2013;48:452-8. [Crossref] [PubMed]
- Yanagiya M, Sato M, Kuwano H, et al. Management of lung nodules newly found by virtual-assisted lung mapping: a case report. Surg Case Rep 2017;3:49. [Crossref] [PubMed]
- Sato M, Kobayashi M, Kojima F, et al. Effect of virtual-assisted lung mapping in acquisition of surgical margins in sublobar lung resection. J Thorac Cardiovasc Surg 2018;156:1691-701.e5. [Crossref] [PubMed]


