
Talc pleurodesis for secondary pneumothorax in elderly patients with persistent air leak
Introduction
Treatments for secondary pneumothorax of elderly patients with pulmonary emphysema are often difficult because of the poor performance status (PS) and impaired pulmonary function. Pleurodesis is often effective in cases unable to tolerate surgical procedures (1-4). Of the many sclerosing agents, talc is considered to be the most effective and least expensive and is widely used based on the British Thoracic Society (BTS) guidelines (1,4-8). We adopted two treatment strategies using talc for secondary pneumothorax in elderly patients with persistent air leak who were ill-suited for standard pneumothorax therapies, including any interventional treatments.
We herein report the effectiveness of thoracoscopic talc poudrage (TTP) and talc slurry pleurodesis (TSP) via a chest tube for secondary pneumothorax in elderly patients with severe emphysema.
Methods
We assessed 17 elderly patients (over 65 years of age) with persistent air leak who received talc pleurodesis for secondary pneumothorax with severe emphysema from April 2013 to March 2017. Persistent air leak was defined as the medical condition of ongoing air leak for more than five days and no decrease in the amount of air leaking after the start of thoracic drainage (9,10). We confirmed that all patient’s lung was sufficiently expanding to the chest wall using computed tomography (CT) scan before talc pleurodesis.
The study was approved by institutional ethics committee board of Suzuka General Hospital (No. 186) and informed consent was obtained from all of the patients.
Japanese Pharmacopoeia talc was sterilized by dry heat at 200 °C for 3 h and used after cooling. The average particle diameter of this talc was 11.7 µm.
The indication for TTP was comprehensively determined based on the patients’ PS, cardiopulmonary function, comorbidity, and expansion of the lung. In patients able to tolerate general anesthesia, TTP (n=11) was performed. Four of the 11 patients in whom air leak was detected intraoperatively received pulmonary wedge resection to control persistent air leak. After poudrage using 10 g of talc, 2 chest tubes were placed (1 at the apex of the pleural cavity and 1 above the diaphragm). In patients unable to tolerate general anesthesia, TSP (n=6) was performed. Talc (10 g) dissolved in 200 mL saline solution was injected via the chest tube at the bedside.
In either approach, a continuous suction pressure of −20 cmH2O was applied until thoracic tube was removed. All patients took orally nonsteroidal anti-inflammatory drugs three times a day for one week after talc pleurodesis.
The subjects were classified into two groups of TTP and TSP according to the treatment strategies. We retrospectively examined the demographics, treatment-related variables (including complications), and outcomes. Continuous variables were expressed as the median and range. Categorical variables were presented as a number and percentage. The analyses between the two groups were performed using Wilcoxon’s rank sum test for continuous variables and Fisher’s exact test and a Chi-squared analysis for categorical variables. A p value of <0.05 was considered statistically significant. The statistical analyses were performed using the JMP software program (version 12.0.1; SAS Institute, Tokyo, Japan).
Results
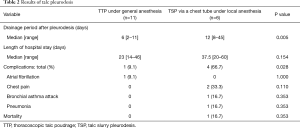
The median age was 75 (range, 65–90) years old; 6 patients (35.3%) were over 80 years of age. All patients in the study population were men. Regarding the affected side, 11 cases were affected on the right, 5 cases on the left, and 1 case on both sides. Four patients had a poor general condition (PS ≥2) and received TSP therapy. Comorbid lung disease aside from pulmonary emphysema included bronchial asthma (n=2) and interstitial pneumonia (IP) (n=4). The median drainage period before pleurodesis was 11 (range, 5–35) days (Table 1). The median drainage period after pleurodesis was 7 (range, 2–35) days. The TTP group showed a significantly shorter drainage period after pleurodesis than the TSP group (TTP: median, 6 days; TSP: median, 12 days; P=0.005). In the TTP group, no significant difference was found in the drainage period after pleurodesis between the four patients who received pulmonary wedge resection and the others (P=0.088).
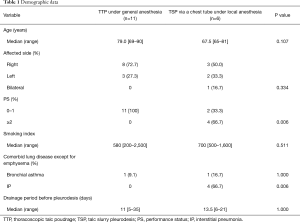
Full table
Complications after pleurodesis included atrial fibrillation (n=1) in the TTP group and chest pain (n=2), bronchial asthma attack (n=1), and pneumonia (n=1) in the TSP group (Table 2). All patients in the TTP group were discharged after pleurodesis. One patient in the TSP group in whom the air leak continued after pleurodesis died in the hospital due to acute exacerbation of IP on the 45th day after pleurodesis. The success rate was 94% (16/17). All patients visited our hospital every 3–6 months for observation after discharge. There were no cases of recurrence among the successfully treated cases during the observation period (median, 24 months; range, 2–75 months).
Full table
Discussion
Secondary pneumothorax sometimes develops in elderly patients with pulmonary emphysema (4). Secondary pneumothorax of elderly patients is more difficult to treat than primary pneumothorax due to these patients’ various comorbidities, poor PS, and impaired cardiopulmonary function (1-4). If an air leak cannot be stopped with thoracic drainage alone, it is necessary to apply additional treatment. However, there are some cases in which surgical intervention is not possible due to severe emphysema or the patient’s condition being too poor to tolerate general anesthesia. In such cases, pleurodesis is indicated as an effective therapy (1-4). When treating secondary pneumothorax, we must also consider the prevention of recurrence of pneumothorax, given the high recurrence rate (39% to 80%) and mortality rate (4.1%) associated with complications of pneumothorax (3,11-14).
A number of sclerosing agents for pleurodesis have been developed, among which talc is considered to be the most effective and least expensive. Talc is therefore widely used for chemical pleurodesis in European countries based on the BTS guidelines (1,4-8,15,16). In clinical practice in Japan, OK-432 (a pulverized product of heat-killed Streptococcus pyogenes) and minocycline are mainly used, but the recurrence rates associated with using these agents for pleurodesis are reportedly high (17-20), and complications, such as a fever and chest pain after pleurodesis, were found to be severe when compared with talc (4,20,21).
Many reports have shown the success rate of talc pleurodesis in the treatment of pneumothorax (defined as the percentage of patients whose thoracic tube is removed) to exceed 80% (1,5), and a meta-analysis showed that the overall success rate (defined as the percentage of patients without relapse after pleurodesis) was 91% (16,17,22). Although there are several reports of talc pleurodesis for spontaneous pneumothorax, including primary pneumothorax, there has been no reports on the utility of talc pleurodesis limited to secondary pneumothorax in elderly patients with persistent air leak. To our knowledge, only one study has directly compared TTP and TSP for secondary pneumothorax in patients over 50 years of age (23). In the present study, the success rate was 94%, which was better than those described in previous reports not limited to secondary pneumothorax (16,17,22). Furthermore, there were no cases of recurrence among the successfully treated patients in our study during the observation period. Talc pleurodesis was therefore deemed effective for the prevention of recurrence in patients with severe emphysema.
The most promising point of TTP is that the talc can be uniformly and intensively sprayed onto the points of severe air leak. In addition, the chest tube can be placed in the appropriate position. As a result, TTP has a significantly shorter drainage duration after pleurodesis than TSP. A report has described the successful performance of TTP under local anesthesia (1). With this method, it is possible to perform talc poudrage and place the chest tube in the proper position as with general anesthesia, thereby further expanding the indications for talc pleurodesis.
In the present study, pleurodesis failed in one patient with IP who had been treated with steroids. The position of the chest tubes was appropriate, and CT scan confirmed that the lung was sufficiently expanded to the chest wall, so TSP was performed. However, no adhesion was formed at all, and the air leak continued even after pleurodesis. In the other three patients who had IP as a basic disease but did not require steroid treatment, TSP was successful. Adhesion is believed to be difficult to form in patients treated with steroids due to the immunosuppressive reaction caused by the steroids (24,25). Acute exacerbation of IP or acute respiratory distress syndrome (ARDS) after talc pleurodesis mostly occurs within 48 h (7,26). One patient with IP who died had no findings of exacerbation before pleurodesis. He got acute exacerbation on the 42nd day after pleurodesis, and died on the 45th day, three days after the exacerbation. So, it is thus unlikely that the talc caused acute exacerbation in the patient. Talc pleurodesis for patients with IP should thus be cautiously indicated. When talc pleurodesis is planned in patients with IP, it should be confirmed that no other treatment is available for secondary pneumothorax, and adequate preparation should be performed in order to prevent ARDS and the acute exacerbation of IP.
Care should also be taken concerning the amount of talc used and the particle size. Previous reports have warned that the risk of developing ARDS is high when the amount of talc exceeds 10 g (27,28), and many studies related to talc pleurodesis have limited the use to a maximum of 5 g (1,5,16,22,29). In addition, talc with small particles migrates to the whole body through the pleural stomata (6,8,30) and causes systemic inflammation (15,31,32) and respiratory failure, including ARDS. It is thus necessary to use “graded talc” (with a large and uniform average particle size) (5,16,24,29). Based on these findings, using 5 g graded talc is thought to be better (17). In the present study, 10 g of talc was used, but we are now using 4 g of Unitalc® (Nobelpharma Co., Ltd., Tokyo, Japan). However, there is a report of ARDS developing even when only 2 g of graded talc was used (26), so sufficient observation and examinations of patients after talc pleurodesis are indispensable.
The main limitations of our study were the small number of patients and its retrospective design. Differences in the patient demographics between the two groups resulted in treatment selection bias. But our study was limited to elderly (>65 years of age) patients with persistent air leak who were ill-suited for standard pneumothorax therapies including any interventional treatments. We think that the patient background as described above is a distinctive point compared with other reports. Talc pleurodesis is not indication for all secondary pneumothorax patients and should be adapted for selected patients such as our study. We would like to provide good information obtained by two types of talc pleurodesis for secondary pneumothorax in elderly patients with persistent air leak. Larger prospective studies are needed to determine the best adaptation of talc pleurodesis for secondary pneumothorax in elderly patients, the most effective amount of talc, and precautions for complications.
TTP was deemed likely to be safe and effective in patients able to tolerate general anesthesia. When considering treatment with talc pleurodesis, caution should be exercised concerning its indication for steroid-dependent patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional ethics committee board of Suzuka General Hospital (No. 186) and informed consent was obtained from all of the patients.
References
- Tschopp JM, Brutsche M, Frey JG. Treatment of complicated spontaneous pneumothorax by simple talc pleurodesis under thoracoscopy and local anesthesia. Thorax 1997;52:329-32. [Crossref] [PubMed]
- Ishida A, Kida H, Muraoka H, et al. Intractable pneumothorax managed by talc pleurodesis and bronchial occlusion with spigots. Respirol Case Rep 2015;3:13-5. [Crossref] [PubMed]
- Sahn SA, Heffner JE. Spontaneous pneumothorax. N Engl J Med 2000;342:868-74. [Crossref] [PubMed]
- How CH, Hsu HH, Chen JS. Chemical pleurodesis for spontaneous pneumothorax. J Formos Med Assoc 2013;112:749-55. [Crossref] [PubMed]
- Bridevaux PO, Tschopp JM, Cardillo G, et al. Short-term safety of thoracoscopic talc pleurodesis for recurrent primary spontaneous pneumothorax: a prospective European multicentre study. Eur Respir J 2011;38:770-3. [Crossref] [PubMed]
- Fraticelli A, Robaglia-Schlupp A, Riera H, et al. Distribution of calibrated talc after intrapleural administration: an experimental study in rats. Chest 2002;122:1737-41. [Crossref] [PubMed]
- Sahn SA. Talc should be used for pleurodesis. Am J Respir Crit Care Med 2000;162:2023-4. [Crossref] [PubMed]
- Aelony Y. Talc pleurodesis and acute respiratory distress syndrome. Lancet 2007;369:1494-6. [Crossref] [PubMed]
- Chee CB, Abisheganaden J, Yeo JK, et al. Persistent air-leak in spontaneous pneumothorax--clinical course and outcome. Respir Med 1998;92:757-61. [Crossref] [PubMed]
- Liberman M, Muzikansky A, Wright CD, et al. Incidence and risk factors of persistent air leak after major pulmonary resection and use of chemical pleurodesis. Ann Thorac Surg 2010;89:891-7. [Crossref] [PubMed]
- Ng CK, Ko FW, Chan JW, et al. Minocycline and talc slurry pleurodesis for patients with secondary spontaneous pneumothorax. Int J Tuberc Lung Dis 2010;14:1342-6. [PubMed]
- Lippert HL, Lund O, Blegvad S, et al. Independent risk factors for cumulative recurrence rate after first spontaneous pneumothorax. Eur Respir J 1991;4:324-31. [PubMed]
- Light RW, O’Hara VS, Moritz TE, et al. Intrapleural tetracycline for the prevention of recurrent spontaneous pneumothorax. Results of a Department of Veterans Affairs cooperative study. JAMA 1990;264:2224-30. [Crossref] [PubMed]
- Isaka M, Asai K, Urabe N. Surgery for secondary spontaneous pneumothorax: risk factors for recurrence and morbidity. Interact Cardiovasc Thorac Surg 2013;17:247-52. [Crossref] [PubMed]
- Genofre EH, Vargas FS, Acencio MM, et al. Talc pleurodesis: evidence of systemic inflammatory response to small size talc particles. Respir Med 2009;103:91-7. [Crossref] [PubMed]
- Heffner JE. Chemical pleurodesis. Available online: https://www.uptodate.com/contents/chemical-pleurodesis
- MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [Crossref] [PubMed]
- Yoshida K, Sugiura T, Takifuji N, et al. Randomized phase II trial of three intrapleural therapy regimens for the management of malignant pleural effusion in previously untreated non-small cell lung cancer: JCOG 9515. Lung Cancer 2007;58:362-8. [Crossref] [PubMed]
- Olsen PS, Andersen HO. Long-term results after tetracycline pleurodesis in spontaneous pneumothorax. Ann Thorac Surg 1992;53:1015-7. [Crossref] [PubMed]
- Inoue T, Ishida A, Nakamura M, et al. Talc pleurodesis for the management of malignant pleural effusions in Japan. Intern Med 2013;52:1173-6. [Crossref] [PubMed]
- Luh KT, Yang PC, Kuo SH, et al. Comparison of OK-432 and mitomycin C pleurodesis for malignant pleural effusion caused by lung cancer. A randomized trial. Cancer 1992;69:674-9. [Crossref] [PubMed]
- Kennedy L, Sahn SA. Talc pleurodesis for the treatment of pneumothorax and pleural effusion. Chest 1994;106:1215-22. [Crossref] [PubMed]
- Kim SJ, Lee HS, Kim HS, et al. Outcome of Video-assisted Thoracoscopic Surgery for Spontaneous Secondary Pneumothorax. Korean J Thorac Cardiovasc Surg 2011;44:225-8. [Crossref] [PubMed]
- Marc N. Talc pleurodesis. Available online: www.uptodate.com/contents/talc-pleurodesis
- Teixeira LR, Vargas FS, Acencio MM, et al. Influence of antiinflammatory drugs (methylprednisolone and diclofenac sodium) on experimental pleurodesis induced by silver nitrate or talc. Chest 2005;128:4041-5. [Crossref] [PubMed]
- Griffo S, Musumeci A, De Luca G, et al. Talc-induced interstitial pneumonitis with respiratory failure. Anaesth Intensive Care 2009;37:127-9. [Crossref] [PubMed]
- Kennedy L, Rusch VW, Strange C, et al. Pleurodesis using talc slurry. Chest 1994;106:342-6. [Crossref] [PubMed]
- Rinaldo JE, Owens GR, Rogers RM. Adult respiratory distress syndrome following intrapleural instillation of talc. J Thorac Cardiovasc Surg 1983;85:523-6. [PubMed]
- Janssen JP, Collier G, Astoul P, et al. Safety of pleurodesis with talc poudrage in malignant pleural effusion: a prospective cohort study. Lancet 2007;369:1535-9. [Crossref] [PubMed]
- Ferrer J, Montes JF, Villarino MA, et al. Influence of particle size on extrapleural talc dissemination after talc slurry pleurodesis. Chest 2002;122:1018-27. [Crossref] [PubMed]
- Maskell NA, Lee YC, Gleeson FV, et al. Randomized trials describing lung inflammation after pleurodesis with talc of varying particle size. Am J Respir Crit Care Med 2004;170:377-82. [Crossref] [PubMed]
- Arellano-Orden E, Romero-Falcon A, Juan JM, et al. Small particle-size talc is associated with poor outcome and increased inflammation in thoracoscopic pleurodesis. Respiration 2013;86:201-9. [Crossref] [PubMed]


