
Sepsis: early interventions count but not RRT!
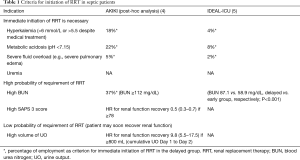
Acute kidney injury (AKI) frequently affects critically ill patients (1). While there are many measures to theoretically prevent the development of AKI or, at least, avoid worsening of AKI (2,3), ultimately, renal replacement therapy (RRT) is often required in the disease management of these patients. However, a continually vexing problem, which often arises when planning the initiation of RRT in critically ill patients, is finding the ideal time to instigate extracorporeal treatment. One can either decide to deliver rapid initiation of RRT or apply a delayed strategy waiting for “urgent” indications to occur (Table 1). The latter may provide the patient with additional time for possible renal recovery and negate the need for RRT. The importance of this is clear, when examining the results of the AKIKI trial (6). Here, 98% of patients in the early group received RRT, compared to 51% in the delayed group. It may therefore be argued that a considerable proportion of patients in the early group would have recovered renal function without ever needing RRT (7). However, the ELAIN trial (8), a single-center study including 231 mainly cardiac-surgical patients showed improved short term and even long-term survival if RRT was started at KDIGO stage 2 as compared to KDIGO stage 3. The majority of the patients included in this study had undergone cardiac surgery, they showed a high severity of disease often requiring mechanical ventilation as well as vasopressors. However, in the delayed group of ELAIN 91% of the patients received RRT, and there was only a 21 hours difference in starting RRT between the early and the delayed groups, giving little time for spontaneous recovery of renal function. As indicated by AKIKI, rapid initiation of RRT may lead to increased costs and staff requirements and may expose the patient to increased complications and side effects originating from the extracorporeal circuit. These include bleeding complications, catheter-related bloodstream infections (6) and leukocyte activation (9). Biomarkers are believed to aid in decision making in the future, however, the ideal biomarker for the initiation of RRT has yet to be determined (10).
Full table
In patients suffering from acute respiratory distress syndrome (ARDS) and AKI, up to 44% require RRT (11,12). In these patients, early RRT is frequently used to control fluid overload, a factor which is known to contribute to worsening respiratory function. A common rationale when treating these patients is, that initiating RRT early prevents fluid overload as well as uremia and therefore promotes faster recovery. However, there are several other pathophysiological pathways which can worsen pulmonary function in patients with AKI (13), throwing this argument open to debate. Similarly, in septic patients, RRT is believed to have an effect on inflammatory mediators (14), however, there is little evidence supporting this theory, when using standard RRT methods. Many pro-inflammatory mediators cannot be filtrated/dialyzed with standard filters/dialyzers because of their large molecular size (14).
To gain further insight into whether timing of RRT in patients with septic shock or ARDS may have an impact on outcome, Gaudry et al. have performed a post hoc analysis of the AKIKI trial (4). The Artificial Kidney Initiation in Kidney Injury (AKIKI) study has been extensively described before (6,7). In short, it was a multicenter randomized trial, in which patients with Kidney Disease: Improving Global Outcomes (KDIGO) stage 3 AKI have been randomized to receive RRT immediately after randomization (early group) or when severe complications due to AKI developed (delayed group). Six hundred and twenty patients were randomized, finding no difference in 60-day mortality between both groups. However, 49% of patients in the delayed group ultimately did not receive RRT. In the current post hoc analysis, patients were divided into subgroups, according to sepsis status, ARDS status, SAPS 3 and SOFA score. Of the 619 patients included in the AKIKI trial, 56% had septic shock at baseline while 33% suffered from ARDS and hence were included in this analysis. The primary endpoint, which the authors defined as 60-day mortality was not affected by the timing of RRT initiation. When assessing the secondary endpoints, nearly 50% of patients ultimately did not need RRT. While this is in line with the findings of the AKIKI main trial, it is a fact, that cannot be stressed enough. RRT is a common procedure on intensive care units (ICUs) and is considered relatively safe, however, there are still some risks associated with the extracorporeal circuit (15). Interestingly, there was no difference found in 2- and 7-day cumulative fluid balance between the early and delayed strategy, in contrary to the belief that early initiation of RRT is a method to avoid fluid overload. However, while cumulative ultrafiltration volume differed significantly between study groups, it was still relatively low during the first 7 days with 3,520 vs. 2,209 mL for the early and delayed group, respectively. Perhaps, a more aggressive approach may have yielded a greater difference in cumulative fluid balance between groups. Patients in the delayed group recovered their renal function significantly earlier than patients in the early group, a fact that was also shown by higher cumulative 2-day urine output in the delayed group. There were no significant differences found in other secondary endpoints, like mechanical ventilation-free days, ICU/hospital length of stay and RRT dependence.
The results are identical to those reported in the AKIKI trial and are somewhat expected, given this post-hoc analysis included 555 of 609 patients (i.e., 91%) analyzed in the AKIKI trial (6). But, with the recent publication of the IDEAL-ICU trial (5), the relevance of these findings for patients with sepsis gains credence (16). The IDEAL-ICU trial was a prospective, multicenter trial, randomizing patients into an early and delayed strategy. This trial was stopped for futility after randomization of 488 patients, as they did not notice a difference in their primary endpoint of 90-day mortality. However, a finding that has to be emphasized is, that while 17% of patients in the delayed group required emergency RRT, 38% of patients in this group did not receive RRT at all (17).
This is in line with the findings of the post hoc analysis of Gaudry et al., who found, as has already been mentioned, that 49% of patients in the delayed group ultimately did not need RRT (4).
So, what conclusion can be drawn from these findings? In a nutshell, a conventional approach of RRT using standard techniques and membranes in which initiation of RRT is triggered by “absolute criteria” including progressive azotemia, uremic symptoms, intractable volume overload, or severe acidosis or hyperkalemia seems to have no negative impact on outcome in septic or ARDS patients. On the other hand, a more aggressive approach, in which patients are treated with RRT relatively early in the course of disease, may prevent a significant proportion of patients from recovering their renal function spontaneously and, thus, from not needing RRT at all. Therefore, a cautious watchful waiting strategy may also be sensible for this specifically vulnerable set of critically ill patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: M Joannidis: Honoraria/Research support from Baxter Healthcare Corp, AM-Pharma, CLS Behring, Fresenius, and Astute Medical. L Forni: Honoraria/Research support from Astute Medical, Fresenius, Baxter Gambro Renal, Ortho Clinical Diagnostics. SJ Klein has no conflicts of interest to declare.
References
- Hoste EA, Bagshaw SM, Bellomo R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med 2015;41:1411-23. [Crossref] [PubMed]
- Joannidis M, Druml W, Forni LG, et al. Prevention of acute kidney injury and protection of renal function in the intensive care unit: update 2017: Expert opinion of the Working Group on Prevention, AKI section, European Society of Intensive Care Medicine. Intensive Care Med 2017;43:730-49. [Crossref] [PubMed]
- Joannidis M, Klein SJ, John S, et al. Prevention of acute kidney injury in critically ill patients: Recommendations from the renal section of the DGIIN, OGIAIN and DIVI. Med Klin Intensivmed Notfmed 2018;113:358-69. [Crossref] [PubMed]
- Gaudry S, Hajage D, Schortgen F, et al. Timing of Renal Support and Outcome of Septic Shock and Acute Respiratory Distress Syndrome. A Post Hoc Analysis of the AKIKI Randomized Clinical Trial. Am J Respir Crit Care Med 2018;198:58-66. [Crossref] [PubMed]
- Barbar SD, Clere-Jehl R, Bourredjem A, et al. Timing of Renal-Replacement Therapy in Patients with Acute Kidney Injury and Sepsis. N Engl J Med 2018;379:1431-42. [Crossref] [PubMed]
- Gaudry S, Hajage D, Schortgen F, et al. Initiation Strategies for Renal-Replacement Therapy in the Intensive Care Unit. N Engl J Med 2016;375:122-33. [Crossref] [PubMed]
- Bagshaw SM, Lamontagne F, Joannidis M, et al. When to start renal replacement therapy in critically ill patients with acute kidney injury: comment on AKIKI and ELAIN. Crit Care 2016;20:245. [Crossref] [PubMed]
- Zarbock A, Kellum JA, Schmidt C, et al. Effect of Early vs Delayed Initiation of Renal Replacement Therapy on Mortality in Critically Ill Patients With Acute Kidney Injury: The ELAIN Randomized Clinical Trial. JAMA 2016;315:2190-9. [Crossref] [PubMed]
- Lehner GF, Harler U, Feistritzer C, et al. Hemofiltration induces generation of leukocyte-derived CD31+/CD41- microvesicles in sepsis. Ann Intensive Care 2017;7:89. [Crossref] [PubMed]
- Klein SJ, Brandtner AK, Lehner GF, et al. Biomarkers for prediction of renal replacement therapy in acute kidney injury: a systematic review and meta-analysis. Intensive Care Med 2018;44:323-36. [Crossref] [PubMed]
- Darmon M, Clec'h C, Adrie C, et al. Acute respiratory distress syndrome and risk of AKI among critically ill patients. Clin J Am Soc Nephrol 2014;9:1347-53. [Crossref] [PubMed]
- Klein SJ, Husain-Syed F, Karagiannidis C, et al. Interactions between lung and kidney in the critically ill. Med Klin Intensivmed Notfmed 2018;113:448-55. [Crossref] [PubMed]
- Hassoun HT, Lie ML, Grigoryev DN, et al. Kidney ischemia-reperfusion injury induces caspase-dependent pulmonary apoptosis. Am J Physiol Renal Physiol 2009;297:F125-37. [Crossref] [PubMed]
- Murugan R, Wen X, Keener C, et al. Associations between Intensity of RRT, Inflammatory Mediators, and Outcomes. Clin J Am Soc Nephrol 2015;10:926-33. [Crossref] [PubMed]
- Klein SJ, Joannidis M. Renal replacement therapy in acute kidney injury. Med Klin Intensivmed Notfmed 2017;112:437-43. [Crossref] [PubMed]
- Perner A, Rhodes A, Venkatesh B, et al. Sepsis: frontiers in supportive care, organisation and research. Intensive Care Med 2017;43:496-508. [Crossref] [PubMed]
- Forni LG, Joannidis M. IDEAL timing of renal replacement therapy in critical care. Nat Rev Nephrol 2019;15:5-6. [Crossref] [PubMed]


