Intrapulmonary recurrence after computed tomography-guided percutaneous needle biopsy of stage I lung cancer
Introduction
Computed tomography-guided percutaneous needle biopsy (CT-PNB) is a useful diagnostic procedure that is used for the evaluation of pulmonary nodules, and is regarded as a relatively safe procedure. Although tumor seeding along the biopsy needle tract after CT-PNB is an extremely rare complication with a reported incidence of 0.06% in Japan (1), it can lead to unnecessary procedures or fatal outcomes. Most of the reported cases of implantation metastasis after CT-PNB were about the tumor seeding, which occurred in the chest wall or the pleura (2,3); however, we present here a case of intrapulmonary recurrence after CT-PNB.
Case presentation
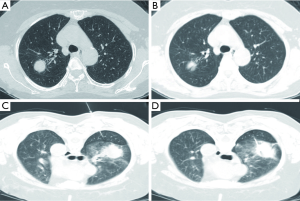
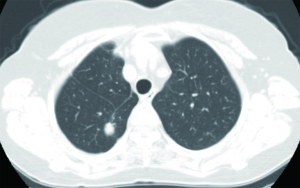
A 70-year-old woman was admitted to our hospital for the evaluation of a growing lung mass. She had undergone a thoracoscopic lobectomy of the right upper lobe 17 months ago, after CT-PNB, using a 22-gauge needle, which had confirmed the lung mass as an adenocarcinoma (Figure 1). She was discharged uneventfully and had been followed-up without additional treatment because there was no evidence of metastasis to the lymph nodes or to the distant organs (pT2aN0M0). On the follow-up according to our protocol for stage I lung cancer, a CT scan of the chest revealed a small lung nodule (0.5 cm in the longest diameter), which was located in the superior segment of the right lower lobe. Six months later, a repeat CT scan of the chest showed that the nodule had grown up to 1.2 cm (Figure 2). On admission, we performed successful CT-PNB of the lesion of the right lower lobe, and pathologic examination revealed an adenocarcinoma, which took the same characteristics as the previous diagnosis from the right upper lobe, which suggested a recurrence (Figure 3). We suspected implantation metastasis, and reviewed the previous biopsy procedures. Finally, we found that the biopsy needle had passed through the superior segment of the right lower lobe to target the right upper lobe lesion, and concluded that the new lesion might be an implantation metastasis, as a result of tumor seeding along the biopsy needle tract. She underwent segmentectomy of the superior segment of the right lower lobe, because there was no evidence of distant metastasis. She recovered well and was followed-up without additional treatment as before.

Discussion
Although tumor seeding along the needle tract after PNB of lung cancer is a rare condition and there are several reports on metastasis in the chest wall or the pleura (2,3), pulmonary parenchymal implantation has not been documented in the English literature. However, the true incidence of pulmonary parenchymal implantation metastasis, after CT-PNB, might be underestimated, due to its difficulty in differentiating a procedure-related implantation from a local recurrence. Moreover, many patients would die before the diagnosis of intrapulmonary recurrence, and more commonly, it might have been removed with the primary lesion, during the curative anatomical resection (4,5). On reviewing the biopsy procedure in this case, the patient was in a prone position because the scapula bone interfered with the anterior approach on the supine position (Figure 1), and the biopsy needle was targeted to the right upper lobe lesion, while passing through the superior segment of the right lower lobe. Therefore, we assumed that the new mass was an implantation metastasis that was related to the CT-PNB procedure rather than a local recurrence or a second primary tumor, because the mass was located in the parenchyma of the RLL, which was far from the pleura, and the biopsy needle had passed through the superior segment of the RLL during the first CT-PNB, where the new mass was supposed to be developed. This was confirmed by a pathologic examination, including an immunohistochemical staining of oncoprotein p53 (Figure 3).
Unfortunately, preventive measures against tumor seeding along the needle tract, while performing CT-PNB, such as the smaller size of the needle, co-axial system of puncture technique, and cauterization of the needle tract using radiofrequency pulses (4), are lack of conclusive proofs. Although they were not tried in this case, innovative bronchoscopic techniques, such as radial probe-endobronchial ultrasound and electromagnetic navigation bronchoscopy, may be safer than CT-PNB because the biopsy tract can be confined only in the parenchyma of the tumor-bearing lobe (6). We present here a lesson from this case that the biopsy needle should not pass through different anatomical compartments other than the target compartment, and this strategy should be kept in mind, especially, when the lesion is located deeply.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Tomiyama N, Yasuhara Y, Nakajima Y, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol 2006;59:60-4. [PubMed]
- Kim JH, Kim YT, Lim HK, et al. Management for chest wall implantation of non-small cell lung cancer after fine-needle aspiration biopsy. Eur J Cardiothorac Surg 2003;23:828-32. [PubMed]
- Inoue M, Honda O, Tomiyama N, et al. Risk of pleural recurrence after computed tomographic-guided percutaneous needle biopsy in stage I lung cancer patients. Ann Thorac Surg 2011;91:1066-71. [PubMed]
- Wiksell H, Schässburger KU, Janicijevic M, et al. Prevention of tumour cell dissemination in diagnostic needle procedures. Br J Cancer 2010;103:1706-9. [PubMed]
- Robertson EG, Baxter G. Tumour seeding following percutaneous needle biopsy: the real story! Clin Radiol 2011;66:1007-14. [PubMed]
- Leong S, Shaipanich T, Lam S, et al. Diagnostic bronchoscopy--current and future perspectives. J Thorac Dis 2013;5:S498-510. [PubMed]


