
Clinical efficacy of high-flow oxygen therapy through nasal cannula in patients with acute heart failure
Introduction
Acute heart failure (AHF) is life-threatening medical condition requiring hospital admission and appropriate oxygen therapy (1). In management of AHF with refractory or progressive hypoxemia after oxygenation via facemask, more intensive oxygen therapies including non-invasive ventilation (NIV) or invasive ventilation through endotracheal intubation are necessary. Earlier studies demonstrated NIV had efficacy and safety in acute respiratory failure (ARF) (2-6). Current guidelines for AHF recommend NIV is the first line oxygen therapy in cases of ARF (7).
Recent studies showed that high-flow oxygen therapy through nasal cannula (HFNC) could reduce intubation rate and mortality rate among patients with ARF (8-10). HFNC become a world-wide popular oxygen therapy in respiratory failure by various etiologies because it is relatively simple and comfortable method by non-invasive manner (11-13). However, physiological efficacy of HFNC lacks evidences (14), and there was no published data about clinical outcomes of HFNC in patients with AHF. Therefore, we analyzed the real-world data of oxygen therapy in patients with AHF focused on HFNC. We evaluated the physiological responses and clinical outcomes of HFNC by comparing with endotracheal intubation.
Methods
Study population
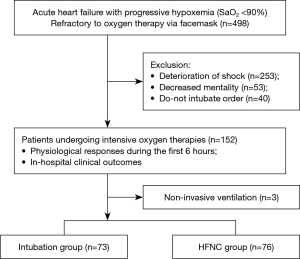
A retrospective cohort analysis was performed in cardiovascular intensive care unit at Gyeongsang National University Hospital, South Korea, from January 2011 to December 2016. In this study, AHF is defined as a heart failure syndrome that requires hospitalization and is characterized by a de novo heart failure presentation or worsening of previously chronic stable heart failure condition. A total of 498 patients had progressive hypoxemia with <90% of pulse oxygen saturation (SaO2) despite the oxygen therapy delivered through an open facemask at a flow rate of 10 L/min or more. Patients who were undergone the refractory hypoxemia were requiring more intensive oxygen therapy including endotracheal intubation, NIV, and HFNC. The decision on which intensive oxygen therapy should be utilized was dependent on the physicians’ opinion and agreement by patients or appropriate surrogate. Exclusion criteria were following: requiring immediate intubation such as shock state (mean arterial pressure <65 mmHg), decreased mental status (Glasgow coma scale <12), or do-not intubate order. Finally, total 149 patients were met the defined inclusion criteria, intubation group (n=73) and HFNC group (n=76) (Figure 1). The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee. The institutional review board approval was obtained from the local ethics committee, and the informed consent was waived.
High-flow oxygen therapy through nasal cannula
The HFNC device (Optiflow®, Fisher & Paykel Healthcare Ltd., Auckland, New Zealand) could deliver up to 60 L/min heated and humidified gas flow and between 0.21 and 1.0 fraction of the inspired oxygen concentration (FiO2). The initial gas flow was 30–40 L/min, which was later modified to achieve the goal of >90% SpO2. We applied the range of flow rate of 30–60 L/min and FiO2 of 40–100% to achieve a target SpO2.
Physiological responses and clinical outcomes
We compared the physiological responses during the first 6 hours between the intubation group and HFNC group. Physiological responses including the mean arterial pressure, heart rate, respiratory rate, and SpO2 were assessed every hour after administration of oxygen therapy.
We assessed the in-hospital clinical outcomes, including the duration of hospital stay, rate of vasopressor use, prevalence of sustained ventricular arrhythmia (more than 30 seconds), and mortality rates between two groups. Additionally, the rate of endotracheal intubation among patients in HFNC group was determined. We analyzed the cumulative incidence of re-admission for heart failure and cardiac mortality during 30 days. In the present study, the confirmation of cardiac death required the documentation of significant arrhythmia or cardiac arrest, death attributable to congestive heart failure, or myocardial infarction in the absence of any other precipitating factors.
Statistical analysis
The continuous variables were expressed as means ± standard deviation, whereas the categorical variables were presented as frequency (n) and percentage (%). Variables without homogeneous variance and normal distribution were expressed as median and interquartile range (IQR). Comparisons between the categorical variables were evaluated using Fisher’s exact test or Pearson’s chi-square test, as appropriate. Fisher’s exact test was used for pairwise comparisons. Meanwhile, repeated-measure analysis-of-variance test was utilized to compare the physiological responses of the two groups. Survival analysis for follow-up clinical outcome was performed using the Kaplan-Meier curve. In all analyses, a P value of <0.05 was considered to be statistically significant. All statistical analyses were performed using the SPSS V21.0 software program (SPSS Inc., Chicago, USA).
Results
Baseline characteristics
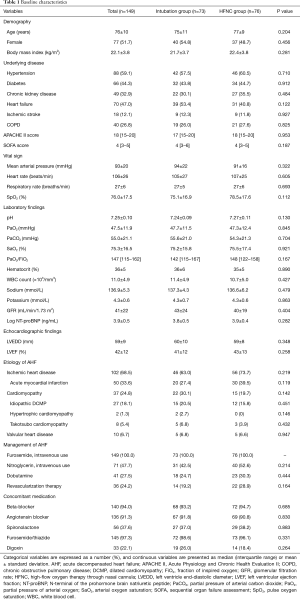
We divided the include patients into two groups, intubation group and HFNC group. Baseline characteristics of two groups were evaluated (Table 1). There were no differences in demographic findings between two groups. Prevalence of cardiovascular risk factors and past medical history were similar in two groups. Seventy-nine patients (53%) were diagnosed as a de novo heart failure presentation. The baseline vital signs and laboratory findings of arterial blood gas analysis and renal function were similar between intubation group and HFNC group. And, no significant differences were found in echocardiography findings of left ventricle dimension and left ventricle ejection fraction.
Full table
Ischemic heart disease was the major etiology of AHF and about half of these participants were diagnosed as an acute myocardial infarction in both groups (63.0% vs. 73.7%, P=0.219; 27.4% vs. 39.5%, P=0.119, respectively). The prescription rate of intravenous diuretics, vasodilator and dobutamine during hospital stay were similar in two groups. And, there were no differences in rate of revascularization therapy and concomitant medication.
Physiological responses of high-flow oxygen therapy through nasal cannula
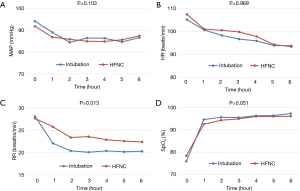
The physiological responses based on change of vital signs and oxygen saturation were assessed during the first 6 hours after the administration of oxygen therapy (Figure 2). Absolute values of vital signs were changed overtime in all parameters (P<0.001). Changes of mean arterial pressure, heart rate, and SpO2 were similar in two groups during the first 6 hours. Mean arterial pressure, heart rate and respiratory rate was remaining stable overtime. Mean values of SpO2 at 1 hour following the administration of oxygen therapy were achieved the treatment goal of >90% SpO2 in the two groups (94.6%±7.8% vs. 92.5%±5.8%, P=0.068).
Clinical outcomes of high-flow oxygen therapy through nasal cannula
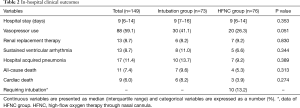
In-hospital clinical outcomes between the two groups were evaluated (Table 2). Median duration of hospital stay was 9 days (IQR, 6–14 days) in total patients and there were no differences depending on each intensive oxygen therapy. There were similar in-hospital clinical outcomes including vasopressor, renal replacement therapy, sustained ventricular arrhythmia, and hospital acquired pneumonia. Moreover, in-hospital mortality rate was not different between intubation group and HFNC group (all-cause death rate, 9.6% vs. 5.3%, P=0.313; cardiac death, 8.2% vs. 3.9%, P=0.274, respectively). Among HFNC group, 66 of 76 patients (86.8%) were successfully recovered from progressive hypoxemia without endotracheal intubation. And among patients who had experienced the endotracheal intubation before HFNC (n=10), 6 patients (60%) were survived during admission. Cumulative incidence of re-admission for heart failure and cardiac mortality during 30 days were statistically not different in intubation group and HFNC group (2.9% vs. 7.0%, P=0.298; 11.2% vs. 5.3%, P=0.212, respectively).
Full table
Discussion
To our knowledge, this study is the first to evaluate the clinical relevance of HFNC among participants with AHF by comparing it to intubation. Compared with intubation group, HFNC group had similar physiological responses including vital signs and pulse oxygen saturation. In-hospital and 30-day follow-up cardiac mortality of HFNC group were statistically not different compared with those of the intubation group. Additionally, most of patients among HFNC group (86.8%) were successfully recovered from progressive hypoxemia without invasive ventilation.
HFNC is now popular oxygen therapy for ARF in patients with various etiologies. However, it remains unclear whether HFNC have a clinical efficacy in patients with AHF. HFNC is one of the intensive oxygen therapies by non-invasive manner. HFNC have strengths that it can deliver heated and humidified gas (up to 100% oxygen) at a maximum flow rate of 60 L/min via nasal cannula (15). Moreover, HFNC can provide a constant FiO2 and oxygen supply through nasal cannula because its interface contributes to increased oxygenation by reducing respiratory dead space and ensuring constant positive pressure (16,17). These mechanisms decrease the breathing work and improve gas exchange, which result to the maintenance of adequate ventilation and oxygenation.
Earlier studies on HFNC suggested the clinical efficacy of HFNC in patients with heart failure. Carratalá et al. reported that patients with cardiogenic pulmonary edema were successfully treated using HFNC (18). Roca et al. conducted a study to determine the beneficial effects of HFNC in patients with stable New York Heart Association class III heart failure and ≤45% left ventricular ejection fraction (LVEF) by estimating the inspiratory collapse of the inferior vena cava (14). Furthermore, Hyun Cho et al. analyzed the predictors of successful HFNC therapy in patients with ARF (19). Their results showed that cardiogenic pulmonary edema as a cause of ARF was one of the predictors of success of HFNC treatment. Although the fact that recent studies have reported the efficacy and safety of HFNC, these studies only presented limited clinical evidences of HFNC in participants with AHF. Therefore, we addressed the clinical relevance of HFNC by determining physiological responses and clinical outcomes of selected patients with AHF.
Immediate invasive ventilation is life-saving oxygen therapy in presence of cardiac and respiratory arrest, life-threatening multi-organ failure, impaired consciousness, and high risk of aspiration. However, intubation in specific population may have potential risk for adverse effects due to originally invasive methods and oxygen toxicity. Liberation duration and adverse events associated with invasive ventilation may be increased in case of patients who have risk factors of elderly patients, renal and hepatic dysfunction, or underlying heart and lung disease. Hence, in tolerable patient with relatively low risk of collapse as defined inclusion criteria of present study, intensive oxygen therapy by non-invasive manner might have an important role among AHF patients. In present study, all patients of intubation group were administered with sedative agents, and the procedure was initiated through the assist-control mode. There was trend that numerically higher rate of vasopressor use was found in intubation group compared with HFNC group (41.1% vs. 26.3%, P=0.051). And, because respiration was mandatory in assist-control mode, respiratory rate decreased more rapidly in intubation group (P=0.013).
Many clinical evidences supported the efficacy and safety of NIV and it is a gold standard treatment of care for AHF (7). However, majority of patients (149 of 152 patients) met inclusion criteria were undergoing the intubation or HFNC, and only 3 patients experienced the NIV as first oxygen therapy in this study. There is a discrepancy between recommendation of current guidelines and real-world practice because compared with NIV, HFNC is more simple and comfortable oxygen therapy for physicians and patients (12,13). In the present study, 66 of 76 patients (86.8%) were successfully recovered from progressive hypoxemia without endotracheal intubation in HFNC group, which were comparable to the results of NIV (20-22).
Our data showed no significant difference in baseline characteristics of both groups. We studied patients who presented by congestive heart failure and admitted at cardiovascular intensive care unit. Therefore, patients had acute respiratory distress syndrome, severe pneumonia, and underlying serious lung disease were excluded. Also, we excluded patients who presented shock, decreased mentality, or refractory multi-organ failure. Because of those inclusion and exclusion criteria, we could compare between HFNC and invasive ventilation therapy based on well-balanced characteristics. To guess major consideration of decision by physicians, we analyzed the time from arrival to applying oxygenation therapy. The mean duration of intubation group was 351 minutes and that of HFNC group was 558 minutes. The 44 patients (60%) received the intubation within 60 minutes after oxygen supply. These results showed the intubation was decided urgently. However, we could not conclude that whether the clinical course of intubation group was more fulminant, and whether applying mechanical ventilation was more convenient to management.
This study has several limitations to consider when interpreting the results. First, present study was a small-sized single-center experience, which may limit its generalization. This study had specific inclusion and exclusion criteria among patients with AHF. Choice of intensive oxygen therapy was decided upon by the physicians’ discretion. Therefore, this study has potential indication and selection bias. A well-designed, prospective randomized trial is required to confirm the results derived from this retrospective study. Second, this study did not evaluate the comparison between HFNC and NIV. Hence, which oxygen therapy would have better physiologic responses and clinical outcomes is needed to be evaluated in the future trials.
In conclusion, this study showed HFNC group had a similar result of improvement of oxygen saturation and in-hospital clinical outcomes compared with intubation group in AHF. Present study supported HFNC could be considered as initial choice of oxygen therapy in selected patients of AHF.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The institutional review board approval was obtained from the local ethics committee (No. GNUH 2017-02-011-001), and the informed consent was waived.
References
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;62:e147-239. [Crossref] [PubMed]
- Masip J, Roque M, Sanchez B, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA 2005;294:3124-30. [Crossref] [PubMed]
- McDermid RC, Bagshaw SM. Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med 2008;359:2068-9. [Crossref] [PubMed]
- Winck JC, Azevedo LF, Costa-Pereira A, et al. Efficacy and safety of non-invasive ventilation in the treatment of acute cardiogenic pulmonary edema--a systematic review and meta-analysis. Crit Care 2006;10:R69. [Crossref] [PubMed]
- Peter JV, Moran JL, Phillips-Hughes J, et al. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet 2006;367:1155-63. [Crossref] [PubMed]
- Masip J, Betbese AJ, Paez J, et al. Non-invasive pressure support ventilation versus conventional oxygen therapy in acute cardiogenic pulmonary oedema: a randomised trial. Lancet 2000;356:2126-32. [Crossref] [PubMed]
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129-200. [Crossref] [PubMed]
- Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 2015;372:2185-96. [Crossref] [PubMed]
- Vargas F, Saint-Leger M, Boyer A, et al. Physiologic Effects of High-Flow Nasal Cannula Oxygen in Critical Care Subjects. Respir Care 2015;60:1369-76. [Crossref] [PubMed]
- Roca O, Riera J, Torres F, Masclans JR. High-flow oxygen therapy in acute respiratory failure. Respir Care 2010;55:408-13. [PubMed]
- Nishimura M. High-Flow Nasal Cannula Oxygen Therapy in Adults: Physiological Benefits, Indication, Clinical Benefits, and Adverse Effects. Respir Care 2016;61:529-41. [Crossref] [PubMed]
- Chanques G, Constantin JM, Sauter M, et al. Discomfort associated with underhumidified high-flow oxygen therapy in critically ill patients. Intensive Care Medicine 2009;35:996-1003. [Crossref] [PubMed]
- Frat JP, Brugiere B, Ragot S, et al. Sequential application of oxygen therapy via high-flow nasal cannula and noninvasive ventilation in acute respiratory failure: an observational pilot study. Respir Care 2015;60:170-8. [Crossref] [PubMed]
- Roca O, Perez-Teran P, Masclans JR, et al. Patients with New York Heart Association class III heart failure may benefit with high flow nasal cannula supportive therapy: high flow nasal cannula in heart failure. J Crit Care 2013;28:741-6. [Crossref] [PubMed]
- Wettstein RB, Shelledy DC, Peters JI. Delivered oxygen concentrations using low-flow and high-flow nasal cannulas. Respir Care 2005;50:604-9. [PubMed]
- Parke RL, McGuinness SP, Eccleston ML. A preliminary randomized controlled trial to assess effectiveness of nasal high-flow oxygen in intensive care patients. Respir Care 2011;56:265-70. [Crossref] [PubMed]
- Dysart K, Miller TL, Wolfson MR, et al. Research in high flow therapy: mechanisms of action. Respir Med 2009;103:1400-5. [Crossref] [PubMed]
- Carratalá Perales JM, Llorens P, Brouzet B, et al. High-Flow therapy via nasal cannula in acute heart failure. Rev Esp Cardiol 2011;64:723-5. [PubMed]
- Hyun Cho W, Ju Yeo H, Hoon Yoon S, et al. High-Flow Nasal Cannula Therapy for Acute Hypoxemic Respiratory Failure in Adults: A Retrospective Analysis. Intern Med 2015;54:2307-13. [Crossref] [PubMed]
- Nava S, Carbone G, DiBattista N, et al. Noninvasive ventilation in cardiogenic pulmonary edema: a multicenter randomized trial. Am J Respir Crit Care Med 2003;168:1432-7. [Crossref] [PubMed]
- Park M, Sangean MC, Volpe Mde S, et al. Randomized, prospective trial of oxygen, continuous positive airway pressure, and bilevel positive airway pressure by face mask in acute cardiogenic pulmonary edema. Crit Care Med 2004;32:2407-15. [Crossref] [PubMed]
- Yamamoto T, Takeda S, Sato N, et al. Noninvasive ventilation in pulmonary edema complicating acute myocardial infarction. Circ J 2012;76:2586-91. [Crossref] [PubMed]


