
Is two lung ventilation with artificial pneumothorax a better choice than one lung ventilation in minimally invasive esophagectomy?
Introduction
Esophagectomy is one of the most important treatments for esophageal cancer. Minimally invasive esophagectomy (MIE) has become the trend for esophageal surgery in recent years, in order to obtain less operative trauma and better postoperative recovery than open surgery (1,2). Traditionally, double lumen endotracheal tube (DLET) is used during thoracic surgery for the purpose of lung isolation and one lung ventilation (OLV) (3,4). Single lumen endotracheal tube (SLET) with bronchial blocker may be used as an alternative (5). However, there are some disadvantages along with OLV, such as the complicated procedure during intubation, possible dislocation during surgery, and postoperative pulmonary complications (6).
History of two lung ventilation (TLV)
TLV with single lumen endotracheal tube (SLET) and CO2 insufflation artificial pneumothorax were introduced into thoracoscopy very early. In 1993, using a pig model, Jones et al. studied the effects of CO2 insufflation on hemodynamics during thoracoscopy (7). Later, Wolfer et al., did related research in patients (8) and in 1995, Wong et al., used this insufflation in transthoracic endoscopic sympathectomy, showing very promising results (9). The first use of TLV in MIE was reported by Palanivelu et al. in 2006 (10). With 130 cases of MIE, their study presented a very low rate of postoperative pneumonia, and no complications of tracheal or lung injury. The history of developments concerning TLV and artificial pneumothorax in thoracoscopy is depicted in Table 1.
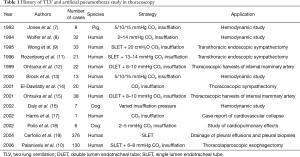
Full table
Pressure of CO2 insufflation in TLV
It’s still controversial whether TLV is a better choice than OLV in MIE (20). The first concern is the safety of CO2 pneumothorax. As reported by Jones et al., the adverse effects of hemodynamic changes could be observed at insufflation pressure of 5 mmHg or greater in pig model (7). Brock et al. tested these changes in human, and their results suggested that pressures of 10 and 15 mmHg might cause circulatory dysfunction (13). Harris et al. also reported a case of cardiovascular collapse caused by insufflation of CO2 (17). However, some other studies suggested that it is safe to use CO2 insufflation in patients with controlled insufflation pressure. Wong et al. reported successful application of 20 cmH2O (14.1 mmHg) CO2 insufflation in TLV during transthoracic endoscopic sympathectomy (9). These results were confirmed by Rozenberg et al. (11). Ohtsuka et al. proposed the use of 8–10 mmHg of insufflation pressure in thoracoscopic harvest of internal mammary artery (12). In MIE, most studies which focus on TLV and artificial pneumothorax have used CO2 pneumothorax with 6–8 mmHg insufflation pressure with the only exception of Cai et al. reporting 8–10 mmHg in MIE (21). In general the insufflation pressure of 6–8 mmHg for MIE is widely accepted (10,22). Circulation dysfunctions were rarely observed, and reversible after ending of insufflation. Our retrospective study with large samples has proved that the insufflation pressure of 8 mmHg is acceptable for thoracoscopy and MIE (23). According to literature and our own study, it seems that 8 mmHg of insufflation pressure is safe in thoracoscopy.
TLV and CO2 pneumothorax in MIE
There are a few studies which concern TLV and CO2 pneumothorax in MIE (Table 2). The first report was by Palanivelu (10). The largest study is from our center (23). Most studies are retrospective, and no RCT has been performed till now. In Palanivelu’s study, their main goal is about the outcome, safety, and feasibility of thoracolaparoscopic esophagectomy, but they considered SLET and CO2 pneumothorax to be helpful for the reduction of incidence of postoperative pulmonary complications. Bonavina et al. compared thoracoscopy in prone position with TLV to Ivor Lewis procedure by thoracotomy (24). Thoracoscopic esophagectomy in the prone position with TLV was associated with a significant improvement of global oxygen delivery and a significant reduction of the pulmonary shunt when compared to the Ivor Lewis operation.
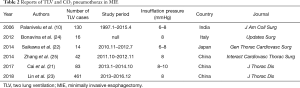
Full table
Saikawa et al. evaluated the safety and efficacy of TLV and CO2 pneumothorax in the prone position (22). Hemodynamics and oxygenation issues were discussed in detail in 14 cases of MIE, and no problems were encountered in their consecutive 62 cases of MIE. They concluded that TLV and CO2 pneumothorax are safe procedure in MIE. Other 3 studies about TLV in MIE have been performed in three different centers from China (21,23,25). They discussed the differences in surgical variables and perioperative complications between TLV group and OLV group in MIE. All of these studies agreed that TLV is safe and feasible in MIE. In minimally invasive pharyngo-laryngo-esophagectomy (MIPLE), Ogino et al. have reported the application of artificial pneumothorax in the prone position as well (26), which will not be discussed in this review.
OLV is essential for MIE in a lateral decubitus position (MIE-LP). But for MIE in prone position (MIE-PP), TLV is also acceptable because the gravity helps expose the surgical area (10,27). MIE-PP is believed to have shorter learning curve and better oxygenation than MIE-LP. However, emergent conversion might be difficult in MIE-PP. In recent years, the novel position—lateral prone position or semiprone position has been introduced for MIE in order to visualize better the upper mediastinum (28,29). Current reports suggest it as a safe and feasible approach with good postoperative outcome, where TLV is commonly adopted. However, more studies are needed to verify its possible advantages.
Disadvantages of OLV and benefits of TLV and CO2 pneumothorax
There are some disadvantages of OLV.
Katz et al. reported hypoxemia during endoscopic transthoracic sympathectomy with left OLV (30). Misthos et al. reported that prolonged OLV and lung re-expansion would cause postresectional pulmonary oxidative stress (31). Frolich et al. reported a case of postoperative atelectasis after OLV (32). An RCT compared DLET versus SLET and blocker in order to evaluate the safety of DLET (33). They found that the DLET group had more vocal cord injuries and postoperative hoarseness than the blocker group, while the incidence of bronchial injuries was similar in two groups (33). Moreover, there are already many reports of bronchial injury and hemorrhage due to blunt trauma with DLET (34-36). Even cardiac rupture is described as complication (37). Use of DLET also means complicated preoperative intubation and intraoperative management (38). From the technical point of view, decreased mobility of trachea and bronchus caused by DLET might impede subcarinal lymph node dissection.
TLV with pneumothorax has more advantages, depicted in Table 2. Using SLET is obviously easier and faster than using DLET. The maintenance of SLET is also easier than maintenance of DLET during thoracoscopy (19). Different studies have proved that TLV with SLET has a better oxygenation than OLV with DLET. Exposure of the operative field is also adequate by the CO2 pneumothorax and TLV (22,23). Moreover, there are no significant difference of surgical parameters between TLV group and OLV group according to current studies (23). When a conversion to open surgery is needed, TLV should be changed to OLV. With SLET, the use of a blocker is a good choice, being more convenient and faster than changing to DLET.
Disadvantages of TLV and CO2 pneumothorax
Concerning its disadvantages, as mentioned before, hemodynamic changes would become obvious if high pressure of CO2 is used for insufflation (7,13). Eight mmHg or lower has been proved safe in MIE (22-25). Another possible concern is air embolism during CO2 insufflation. However, no case has been observed till now in all of reported clinical studies. Some authors focus on acidosis and respiratory changes during CO2 pneumothorax (21-23). Parameters such as pH, PaO2, PaCO2, and air-way pressure, have been carefully recorded and discussed. Results suggested that the changes obtained are acceptable, and would recover very fast after finishing the artificial pneumothorax. One recent study has found that CO2 pneumothorax may impair the intraoperative coagulation of MIE patients (39). But this conclusion is still not for sure. They only studied intraoperative thromboelastogram parameter, the rest of coagulation parameters are lacking. No similar results have been reported by other authors.
Another potential problem of CO2 pneumothorax, which has not been discussed, is its effects on tumor proliferation, metastasis, and tumor invasion. Using pneumoperitoneum, a possible relationship is found between CO2 insufflation and the ability of tumor cell proliferation, metastasis, and invasion, especially under conditions of high insufflation pressure and prolonged insufflation time (27,29). However, no similar research has been performed in thoracoscopy till now, where further studies are needed.
Conclusions
The possible advantages and disadvantages of TLV and OLV have been listed in Table 3. The advantages of SLET include convenient intubation, easy intraoperative management, and good oxygenation. Hemodynamic and respiratory changes are acceptable and controllable with limited insufflation pressure in TLV. According to current clinical evidences, TLV and CO2 pneumothorax is safe and feasible in MIE. In accordance with this, we believe that TLV is a possible good alternative of OLV in MIE. However, further work is needed to verify some unsolved problems, such as its effects on coagulation function and tumor biology.

Full table
Acknowledgements
Funding: This study was supported by the National Nature Science Foundation of China (grant No. 81370587, 81500568, 81400681).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Luketich JD, Pennathur A, Awais O, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg 2012;256:95-103. [Crossref] [PubMed]
- Yerokun BA, Sun Z, Yang CJ, et al. Minimally Invasive Versus Open Esophagectomy for Esophageal Cancer: A Population-Based Analysis. Ann Thorac Surg 2016;102:416-23. [Crossref] [PubMed]
- Cohen E. One lung ventilation: prospective from an interested observer. Minerva Anestesiol 1999;65:275-83. [PubMed]
- Durkin C, Schisler T, Lohser J. Current trends in anesthesia for esophagectomy. Curr Opin Anaesthesiol 2017;30:30-5. [PubMed]
- Campos JH. Which device should be considered the best for lung isolation: double-lumen endotracheal tube versus bronchial blockers. Curr Opin Anaesthesiol 2007;20:27-31. [Crossref] [PubMed]
- Roth JV. Complications of One-lung Ventilation: Is It the Blood Flow or the Ventilation? Anesthesiology 2016;125:1253-4. [Crossref] [PubMed]
- Jones DR, Graeber GM, Tanguilig GG, et al. Effects of insufflation on hemodynamics during thoracoscopy. Ann Thorac Surg 1993;55:1379-82. [Crossref] [PubMed]
- Wolfer RS, Krasna MJ, Hasnain JU, et al. Hemodynamic effects of carbon dioxide insufflation during thoracoscopy. Ann Thorac Surg 1994;58:404-7; discussion 407-8. [Crossref] [PubMed]
- Wong RY, Fung ST, Jawan B, et al. Use of a single lumen endotracheal tube and continuous CO2 insufflation in transthoracic endoscopic sympathectomy. Acta Anaesthesiol Sin 1995;33:21-6. [PubMed]
- Palanivelu C, Prakash A, Senthilkumar R, et al. Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position--experience of 130 patients. J Am Coll Surg 2006;203:7-16. [Crossref] [PubMed]
- Rozenberg B, Katz Y, Isserles SA, et al. Near-sitting position and two-lung ventilation for endoscopic transthoracic sympathectomy. J Cardiothorac Vasc Anesth 1996;10:210-2. [Crossref] [PubMed]
- Ohtsuka T, Imanaka K, Endoh M, et al. Hemodynamic effects of carbon dioxide insufflation under single-lung ventilation during thoracoscopy. Ann Thorac Surg 1999;68:29-32; discussion 33. [Crossref] [PubMed]
- Brock H, Rieger R, Gabriel C, et al. Haemodynamic changes during thoracoscopic surgery the effects of one-lung ventilation compared with carbon dioxide insufflation. Anaesthesia 2000;55:10-6. [Crossref] [PubMed]
- El-Dawlatly AA, Al-Dohayan A, Samarkandi A, et al. Right vs left side thoracoscopic sympathectomy: effects of CO2 insufflation on haemodynamics. Ann Chir Gynaecol 2001;90:206-8. [PubMed]
- Ohtsuka T, Nakajima J, Kotsuka Y, et al. Hemodynamic responses to intrapleural insufflation with hemipulmonary collapse. Surg Endosc 2001;15:1327-30. [Crossref] [PubMed]
- Daly CM, Swalec-Tobias K, Tobias AH, et al. Cardiopulmonary effects of intrathoracic insufflation in dogs. J Am Anim Hosp Assoc 2002;38:515-20. [Crossref] [PubMed]
- Harris RJ, Benveniste G, Pfitzner J. Cardiovascular collapse caused by carbon dioxide insufflation during one-lung anaesthesia for thoracoscopic dorsal sympathectomy. Anaesth Intensive Care 2002;30:86-9. [Crossref] [PubMed]
- Polis I, Gasthuys F, Gielen I, et al. The effects of intrathoracic pressure during continuous two-lung ventilation for thoracoscopy on the cardiorespiratory parameters in sevoflurane anaesthetized dogs. J Vet Med A Physiol Pathol Clin Med 2002;49:113-20. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Sheils TM, et al. Video-assisted thoracoscopic surgery using single-lumen endotracheal tube anesthesia. Chest 2004;126:281-5. [Crossref] [PubMed]
- Takeuchi H, Kitagawa Y. Two-lung ventilation in the prone position: is it the standard anesthetic management for thoracoscopic esophagectomy? Gen Thorac Cardiovasc Surg 2014;62:133-4. [Crossref] [PubMed]
- Cai L, Li Y, Sun L, et al. Better perioperative outcomes in thoracoscopic-esophagectomy with two-lung ventilation in semi-prone position. J Thorac Dis 2017;9:117-22. [Crossref] [PubMed]
- Saikawa D, Okushiba S, Kawata M, et al. Efficacy and safety of artificial pneumothorax under two-lung ventilation in thoracoscopic esophagectomy for esophageal cancer in the prone position. Gen Thorac Cardiovasc Surg 2014;62:163-70. [Crossref] [PubMed]
- Lin M, Shen Y, Wang H, et al. A comparison between two lung ventilation with CO2 artificial pneumothorax and one lung ventilation during thoracic phase of minimally invasive esophagectomy. J Thorac Dis 2018;10:1912-8. [Crossref] [PubMed]
- Bonavina L, Laface L, Abate E, et al. Comparison of ventilation and cardiovascular parameters between prone thoracoscopic and Ivor Lewis esophagectomy. Updates Surg 2012;64:81-5. [Crossref] [PubMed]
- Zhang R, Liu S, Sun H, et al. The application of single-lumen endotracheal tube anaesthesia with artificial pneumothorax in thoracolaparoscopic oesophagectomy. Interact Cardiovasc Thorac Surg 2014;19:308-10. [Crossref] [PubMed]
- Ogino M, Ebihara Y, Homma A, et al. The surgical outcome of minimally invasive pharyngo-laryngo-oesophagectomy in prone position. J Minim Access Surg 2018. [Epub ahead of print]. [PubMed]
- Koyanagi K, Ozawa S, Tachimori Y. Minimally invasive esophagectomy performed with the patient in a prone position: a systematic review. Surg Today 2016;46:275-84. [Crossref] [PubMed]
- Li X, Lai FC, Qiu ML, et al. Minimally Invasive Esophagectomy in the Lateral-prone Position: Experience of 226 Cases. Surg Laparosc Endosc Percutan Tech 2016;26:60-5. [Crossref] [PubMed]
- Lin M, Shen Y, Feng M, et al. Minimally invasive esophagectomy: Chinese experiences. J Vis Surg 2016;2:134. [Crossref] [PubMed]
- Katz Y, Zisman E, Isserles SA, et al. Left, but not right, one-lung ventilation causes hypoxemia during endoscopic transthoracic sympathectomy. J Cardiothorac Vasc Anesth 1996;10:207-9. [Crossref] [PubMed]
- Misthos P, Katsaragakis S, Milingos N, et al. Postresectional pulmonary oxidative stress in lung cancer patients. The role of one-lung ventilation. Eur J Cardiothorac Surg 2005;27:379-82; discussion 382-3. [Crossref] [PubMed]
- Frölich MA, Janelle GM. Postoperative atelectasis after one-lung ventilation with the Univent tube in a child. J Clin Anesth 2003;15:159-63. [Crossref] [PubMed]
- Knoll H, Ziegeler S, Schreiber JU, et al. Airway injuries after one-lung ventilation: a comparison between double-lumen tube and endobronchial blocker: a randomized, prospective, controlled trial. Anesthesiology 2006;105:471-7. [Crossref] [PubMed]
- Chu CP, Chen PP. Tracheobronchial injury secondary to blunt chest trauma: diagnosis and management. Anaesth Intensive Care 2002;30:145-52. [Crossref] [PubMed]
- Kim HY, Baek SH, Kim KH, et al. Endobronchial hemorrhage after intubation with double-lumen endotracheal tube in a patient with idiopathic thrombocytopenic purpura for minimally invasive cardiac surgery: a case report. Korean J Anesthesiol 2014;66:59-63. [Crossref] [PubMed]
- Pandey V, Meena DS, Choraria S, et al. Tracheobronchial Injury caused by Blunt Trauma: Case Report and Review of Literature. J Clin Diagn Res 2016;10:UD01-3. [PubMed]
- Misao T, Yoshikawa T, Aoe M, et al. Bronchial and cardiac ruptures due to blunt trauma. Gen Thorac Cardiovasc Surg 2011;59:216-9. [Crossref] [PubMed]
- Kim HY, Baek SH, Je HG, et al. Comparison of the single-lumen endotracheal tube and double-lumen endobronchial tube used in minimally invasive cardiac surgery for the fast track protocol. J Thorac Dis 2016;8:778-83. [Crossref] [PubMed]
- Mao QX, Guo W, Huang BQ, et al. Impact of artificial capnothorax on coagulation in patients during video-assisted thoracoscopic esophagectomy for squamous cell carcinoma. Surg Endosc 2016;30:2766-72. [Crossref] [PubMed]


