
Risk factors of delayed awakening after aortic arch surgery under deep hypothermic circulatory arrest with selective antegrade cerebral perfusion
Introduction
Brain injury is a major complication of aortic arch surgery. The estimated rate of temporary and permanent brain damage after aortic arch surgery is 19–28% and 4–28%, respectively (1). Delayed awakening often results in prolonged mechanical ventilation and stay in the intensive care unit (2,3). However, the rate of delayed awakening after aortic arch surgery is not clear (2,3). In the current retrospective analysis, we collected the clinical data of all patients undergoing aortic arch surgery under deep hypothermic circulatory arrest (DHCA) in combination with selective antegrade cerebral perfusion (SACP) during a period from September 2015 to September 2017, and examined potential risk factors for delayed awakening.
Methods
Study objects
The research was approved by the ethics committee of Drum Tower Hospital in Nanjing (No. 2013-025-02). All cases of aortic arch surgery under DHCA + SACP during a period from September 2015 to September 2017 were identified. Surgery, anesthesia, cardiopulmonary bypass (CPB) and intensive care were performed by the same medical teams. Diagnosis of the underlying diseases was established using color doppler echocardiography (UCG) and computed tomography (CT). Delayed awakening was defined as recovery of consciousness 24 h after surgery.
Surgery
Surgery was carried out under CPB and combined intravenous-inhalation general anesthesia that consisted of etomidate, fentanyl, midazolam and sevoflurane at standard doses. CPB was instituted through cannulation in the right axillary artery, the right femoral artery and the right atrium. Proximal operation was carried out during the period of cooling and CPB was stopped when the anal temperature decreased to 18–22 °C. SACP was conducted through the right axillary artery at an initial flow rate of 10–15 mL/(kg·min); reconstruction of the descending aorta and aortic arch was completed during the period of SACP. Upon completion of the reconstruction, CPB was re-instituted. Protective measures other than SACP included ice cap cooling, methylprednisolone, magnesium sulfate and mannitol.
Postoperative management
Postoperative measures intended to minimize brain injury included head cooling with ice cap, intravenous infusion of piracetam (20 g, twice daily), trisialoganglioside-GT1b (60 mg, once daily), citicoline sodium (2 g, once daily), sodium aescinate (20 mg, once daily), 20% mannitol (200 mL, twice daily), and albumin (10 g, once daily). None of the patients received sedative agent prior to recovery of consciousness.
Measures of observation
In addition to demographic information, we also extracted relevant medical histories, including hypertension, diabetes, hyperlipidemia, cerebrovascular diseases, atrial fibrillation, and smoking status. Lab measures included hemoglobin, albumin, creatinine, and international standardization ratio (INR). Measure of cardiovascular functions included carotid artery involvement, left ventricular ejection fraction (EF), left ventricular end-diastolic diameter (LVDd), and the diameter of the ascending aorta. Collected intraoperative measures included operation time, CPB time, ascending aorta blocking time, DHCA time, SACP time, rewarming time, nasopharyngeal temperature, anus temperature, mean arterial pressure, selective cerebral perfusion flow rate, blood transfusion, Bentall operation, aortic arch replacement, CABG surgery, mitral valve plasty (MVP), and femoral artery intubation. Postoperative measures included timing of consciousness recovery, 24 h blood pressure range, and secondary chest hemostasis.
Statistical analysis
All statistical analyses were conducted using SPSS 13.0. Continuous variables are presented as mean and standard deviation (SD), and analyzed with Student’s t-test. Categorical variables were analyzed with Chi-squared test. A multivariate logistic regression model was used to analyze the risk factors for delayed awakening. P<0.05 was considered statistically significant.
Results
A total of 168 subjects (116 men and 52 women, average age: 50.46±11.35 years) were included in data analysis. Underlying diseases included aortic dissection of Stanford type A (n=141) and aneurysm of the ascending aorta or aortic arch (n=27). One hundred and twenty-nine cases were emergency surgery. Surgical procedures included ascending aorta replacement + aortic arch replacement + descending aorta trunk stent implantation (n=84), Bentall operation + aortic arch replacement + trunk stent implantation (n=29), ascending aorta replacement + aortic arch replacement (n=27), ascending aorta replacement + aortic arch and descending aorta implantation with bifurcation stent (n=13), Bentall operation + aortic arch replacement (n=10), Bentall operation + aortic arch and descending aorta implantation with bifurcation stent (n=7). Coronary artery bypass grafting (CABG) and MVP were carried out in 15 and 8 cases, respectively.
In-hospital mortality rate was 19.05% (32/168). All deaths occurred after 24 h of surgery. Causes of death included multiple organ failure (n=23), heart failure (n=7), mediastinal infection (n=1) and pulmonary hemorrhage (n=1). No death cases occurred within 24 h after the operation.
Delayed awakening occurred in 76 cases (76/168, 45.24%). Subjects with delayed awakening had older age, hypertension, higher rate of emergency surgery and blood transfusion, and longer CPB time and myocardial blocking time (Table 1). In-hospital mortality rate was 31.58% (24/76) in subjects with delayed awakening vs. 8.70% (8/92) in those without delayed awakening (P=0.003).
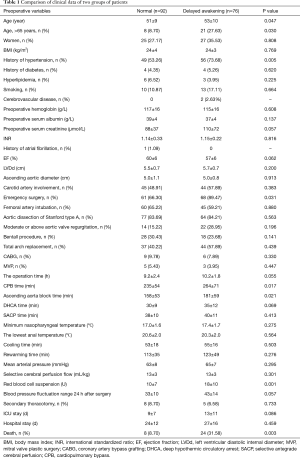
Full table
A total of 127 patients received follow-up beyond the time of discharge from hospital: 53 in patients with delayed awakening vs. 74 in those without delayed awakening. The follow-up duration was 4–27 months. Eight patients died during the follow-up period (5 vs. 3 in patients with vs. without delayed awakening). Causes of the death included cerebral apoplexy (n=2), heart failure (n=3), pulmonary hemorrhage (n=2), and unknown (n=1). One patient received second surgery at 13 months. Among the 119 patients surviving at the last follow-up, New York Heart Association functional class was grade I in 74 (26 in subjects with delayed awakening), grade II in 34 (19 in subjects with delayed awakening), and grade III in 11 (6 in subjects with delayed awakening).
Multivariate regression analysis
After adjusting for potential confounding factors, logistic regression analysis showed the following independent risks for delayed awakening: emergency surgery (P=0.005) and CPB time >240 min (P<0.001) (Table 2).
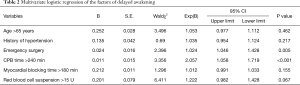
Full table
Discussion
A variety of factors have been associated with delayed awakening after surgeries under DHCA + SACP. Reported intraoperative factors include: (I) atherosclerotic plaque falling during the operation or small emboli occurring during CPB, (II) cerebrovascular contraction and reduced cerebral blood flow resulting from reperfusion injury and inflammatory reaction, (III) long circulatory arrest time, (IV) uneven cooling, and (V) pre-existing diseases (1,2,4). Postoperative factors associated with delayed awakening include high fever, hypoxemia, and intracranial hypertension (5,6).
Advanced age is a major risk for complications and mortality after aortic arch surgery (4-6). In elderly patients, many factors (e.g., low vital organ reserve, co-morbid diseases, and low immune response) may also contribute to delayed awakening after surgery under DHCA.
Previous studies suggested hypertension is a risk of delayed awakening (7). Sclerotic lesions in patients receiving surgery for aortic arch diseases decrease blood supply to the brain, and increase the likelihood of emboli. In patients with hypertension, especially those with combined diabetes and cerebrovascular diseases, the ability of cerebrovascular autonomic regulation significantly decreases and perioperative hypotension is more likely to occur and leads to delayed awakening (8).
Logistic regression analysis in the current study identified emergency surgery as an independent risk for delayed awakening. Most patients with acute aortic dissection of Stanford type A require emergency aortic arch replacement (9). A previous study showed much higher mortality rates (50%) for emergency surgery vs. 9% mortality rates for elective surgery (9). Surgical risks were closely related to whether the patients were in critical preoperative condition (10).
Consistent with previous findings, we found significantly higher rates of delayed awakening in subjects receiving CPB for longer than 240 min. In a study of 220 patients undergoing aortic arch surgery, Kazui et al. found that CPB of more than 300 min was a risk factor of brain complications (11). With increasing CPB time, more inflammatory cytokines were released, which in turn aggravated ischemic-reperfusion injury. In addition, patients with long time CPB are more likely to have severe aortic lesions and more chances of brain injury (10,11).
Transfusion of large amounts of blood disrupts coagulation and promotes microemboli formation. Also, the need for blood transfusion indicates the presence of brain hypoperfusion and embolism (12). Higher rates of blood transfusion in subjects with delayed awakening are generally consistent with these notions.
Low temperature and selective cerebral perfusion provide brain protection in patients undergoing aortic arch surgery (13,14). Selective cerebral perfusion extends the safety time for circulatory arrest. In the US, aortic arch surgery is typically carried out under deep low temperature. The prevailing belief is that the safety time for circulatory arrest depends on the final temperature of the brain and ASCP does not lower postoperative complications of the brain. They also believe that using medical ice cap intraoperatively is important to keep the balance of brain temperature (15). Mild hypothermic cerebral perfusion is used more often in European countries with encouraging clinical outcomes, including reduced risk of bleeding and blood transfusion and less severe coagulopathy (16). In the current study, core body temperature, DHCA/SACP time, cooling and rewarming time did not differ significantly between patients with vs. without delayed awakening.
In our study, SACP was conducted using the right axillary artery. Unilateral SACP can meet the demand of the brain for blood supply (17), but requires the presence of a competent Willi’s circle (18).
For surgeries under DHCA, SACP rate of 8–10 mL/(kg·min) is widely accepted and the right radial artery pressure is maintained at 40–60 mmHg (19,20). In the current study, the perfusion rate was 13.44±3.62 mL/(kg·min) during unilateral SACP while body temperature was maintained at 18–22 °C, with no significant difference in perfusion rate between subjects with vs. without delayed awakening. However, Numatas reported that satisfactory clinical outcomes (96.5% of the patients achieving consciousness within 8 h) could be obtained with a lower flow rate (500 mL/min during SACP).
In summary, the current study suggested that emergency surgery and CPB time >240 min are risk factors for delayed awakening in patients undergoing aortic arch surgery under DHCA + SACP.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The research was approved by the ethics committee of Drum Tower Hospital in Nanjing (No. 2013-025-02).
References
- Ueda T, Shimizu H, Ito T, et al. Cerebral complications associated with selective perfusion of the arch vessels. Ann Thorac Surg 2000;70:1472-7. [Crossref] [PubMed]
- Zhang Q, Ma X, Zhang W, et al. Surgical repair and reconstruction of aortic arch in debakey type I aortic dissection: recent advances and single-center experience in the application of branched stent graft. J Cardiothorac Surg 2017;12:86. [Crossref] [PubMed]
- Velasquez CA, Zafar MA, Saeyeldin A, et al. Two-Stage Elephant Trunk approach for open management of distal aortic arch and descending aortic pathology in patients with Marfan syndrome. Ann Cardiothorac Surg 2017;6:712-20. [Crossref] [PubMed]
- Nakano M, Kimura N, Matsumoto H, et al. Characteristics of Abdominal Aortic Aneurysm in Japanese Patients Aged 50 Years or Younger. Ann Vasc Dis 2017;10:119-24. [Crossref] [PubMed]
- Li ZD, Liu Y, Zhu J, et al. Risk factors of pre-operational aortic rupture in acute and subacute Stanford type A aortic dissection patients. J Thorac Dis 2017;9:4979-87. [Crossref] [PubMed]
- Colli A, Carrozzini M, Galuppo M, et al. Analysis of early and long-term outcomes of acute type A aortic dissection according to the new international aortic arch surgery study group recommendations. Heart Vessels 2016;31:1616-24. [Crossref] [PubMed]
- Barr JG, Sepehripour AH, Jarral OA, et al. A review of the surgical management of right-sided aortic arch aneurysms. Interact Cardiovasc Thorac Surg 2016;23:156-62. [Crossref] [PubMed]
- Schoenhoff FS, Carrel TP. Re-interventions on the thoracic and thoracoabdominal aorta in patients with Marfan syndrome. Ann Cardiothorac Surg 2017;6:662-71. [Crossref] [PubMed]
- Suzuki T, Asai T, Nota H, et al. Selective cerebral perfusion with mild hypothermic lower body circulatory arrest is safe for aortic arch surgery. Eur J Cardiothorac Surg 2013;43:e94-8. [Crossref] [PubMed]
- Pepe G, Giusti B, Sticchi E, et al. Marfan syndrome: current perspectives. Appl Clin Genet 2016;9:55-65. [Crossref] [PubMed]
- Kazui T, Washiyama N, Muhammad BA, et al. Total arch replacement using aortic arch branched grafts with the aid of antegrade selective cerebral perfusion. Ann Thorac Surg 2000;70:3-8. [Crossref] [PubMed]
- Zhao L, Chai Y, Li Z. Clinical features and prognosis of patients with acute aortic dissection in China. J Int Med Res 2017;45:823-9. [Crossref] [PubMed]
- Zou LH, Liu JP, Zhang H, et al. Cerebral Metabolic Profiling of Hypothermic Circulatory Arrest with and Without Antegrade Selective Cerebral Perfusion: Evidence from Nontargeted Tissue Metabolomics in a Rabbit Model. Chin Med J (Engl) 2016;129:702-8. [Crossref] [PubMed]
- Vranken NP, Weerwind PW, Sutedja NA, et al. Cerebral Oximetry and Autoregulation during Cardiopulmonary Bypass: A Review. J Extra Corpor Technol 2017;49:182-91. [PubMed]
- Bin Mahmood SU, Velasquez CA, Zafar MA, et al. Medical management of aortic disease in Marfan syndrome. Ann Cardiothorac Surg 2017;6:654-61. [Crossref] [PubMed]
- Colli A, Carrozzini M, Francescato A, et al. Acute DeBakey Type I aortic dissection without intimal tear in the arch: is total arch replacement the right choice? Interact Cardiovasc Thorac Surg 2018;26:84-90. [Crossref] [PubMed]
- Sun LZ, Ma WG, Zhu JM, et al. Sun's procedure for chronic type A aortic dissection: total arch replacement using a tetrafurcate graft with stented elephant trunk implantation. Ann Cardiothorac Surg 2013;2:665-6. [PubMed]
- Merkkola P, Tulla H, Ronkainen A, et al. Incomplete circle of Willis and right axillary artery perfusion. Ann Thorac Surg 2006;82:74-9. [Crossref] [PubMed]
- Gong M, Ma WG, Guan XL, et al. Moderate hypothermic circulatory arrest in total arch repair for acute type A aortic dissection: clinical safety and efficacy. J Thorac Dis 2016;8:925-33. [Crossref] [PubMed]
- Rimmer L, Fok M, Bashir M. The History of Deep Hypothermic Circulatory Arrest in Thoracic Aortic Surgery. Aorta (Stamford) 2014;2:129-34. [Crossref] [PubMed]


