
Spontaneous postpartum pneumomediastinum: beware of too much diagnostics
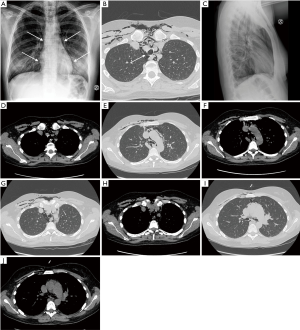
In this brief letter we present the case of a 33-year-old primiparous healthy woman in labour who entered our hospital at 38 weeks +6 days of gestational age. After 4 hours and 30 minutes of spontaneous labour, she delivered a healthy newborn. Two hours later she became slightly tachypneic and, in the subsequent 2 hours, developed chest pain at deep inspiration and subcutaneous emphysema that extended from the upper thorax to the neck and to the right side of the face. Heart rate and blood pressure remained normal at 88 bpm and 120/65 mmHg respectively, with an oxygen saturation of 98% on room air. Chest breath sounds were diminished, although present bilaterally. Due to subcutaneous emphysema, chest ultrasound did not provide further information. Patient chest X-rays and high-resolution computed tomography (CT) are shown in Figure 1. A 3-year board-certified, experienced radiologist’s CT report confirmed the pneumomediastinum, excluded pneumothorax and pulmonary embolism and pointed out one suspected tracheal lesion. The patient was then transferred to the subintensive care unit where she underwent a fiber optic bronchoscopy procedure (FOB). The FOB did not detect any tracheal tear. The day after, the patient was transferred to the obstetric ward with stable vital signs; control chest X-rays, 4 days after bronchoscopy and at 1 month after hospital discharge, showed no residual pneumomediastinum or subcutaneous emphysema.
Hamman’s syndrome is a rare condition characterized by spontaneous pneumomediastinum and subcutaneous emphysema associated with chest pain. First described by Macklin as “the transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum” it can be summarized as follows: alveolar ruptures, air dissection along bronchovascular sheaths, and spreading into the mediastinum (1). It mostly affects young men (13–35 years) and occurs after intense physical activity, forceful coughing from asthmatic bronchospasm or pulmonary infection, retching or vomiting, or excessive Valsalva maneuver (2).
A typical sign of this syndrome is the “Hamman’s sign” or “Hammond’s crunch,” a crunching, rasping sound, synchronous with the heartbeat, heard over the precordium and produced by the heart beating against air-filled tissues. Other features include retrosternal chest pain (usually irradiated to the neck) and subcutaneous emphysema. Dysphagia and dysphonia are related to pneumomediastinum, while dyspnea is associated with the presence of pneumothorax when air moves between visceral and parietal pleura (3). If a large pneumothorax is present, a chest drainage tube may be required.
Differential diagnosis is very important and must exclude life-threatening postpartum conditions such as pulmonary embolism, amniotic fluid embolism, aortic dissection, myocardial infarction, Boerhaave’s syndrome and pneumothorax. Under-pressure air trapping in the mediastinal space configures the so called malignant pneumomediastinum, that is a life-threatening condition characterized by hypotension and reduced cardiac output.
Chest X-ray is the single most important examination, which often allows a proper diagnosis of spontaneous pneumomediastinum (4). CT scan may be required in uncertain cases or in order to best define the extension of subcutaneous emphysema (5).
Except in rare cases of tension pneumomediastinum, Hamman’s syndrome is not a life-threatening condition and, once diagnosed, may require only supportive and symptomatic therapy, which includes oxygen, analgesics and sedatives as necessary. Patients can be safely discharged if clinically stable and without any condition at evolutive risk. Routine follow-up examinations are not necessary (3).
In our case, although highly sensitive and specific, the CT scan led to a false positive misinterpretation of tracheal wall rupture with a consequent unnecessary bronchoscopy. The key clinical message of our letter is that Hamman’s syndrome is a rare condition—one case in over 100,000 vaginal deliveries—that needs an early and proper diagnosis by excluding other life-threatening conditions. Moreover, in stable patients, further exams are not recommended as they can result in false positive misinterpretations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Macklin CC. Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: Clinical implications. Arch Intern Med 1939;64:913-26. [Crossref]
- Jayran-Nejad Y. Subcutaneous emphysema in labour. Anaesthesia 1993;48:139-40. [Crossref] [PubMed]
- Song IH, Lee SY, Lee SJ, et al. Diagnosis and treatment of spontaneous pneumomediastinum: experience at a single institution for 10 years. Gen Thorac Cardiovasc Surg 2017;65:280-4. [Crossref] [PubMed]
- Kouki S, Fares AA. Postpartum spontaneous pneumomediastinum 'Hamman's syndrome'. BMJ Case Rep 2013;2013. [Crossref] [PubMed]
- Kelly S, Hughes S, Nixon S, et al. Spontaneous pneumomediastinum (Hamman's syndrome). Surgeon 2010;8:63-6. [Crossref] [PubMed]


