The rise of human factors: optimising performance of individuals and teams to improve patients’ outcomes
Introduction
The improvement of outcomes has always been important for surgeons. This aim has been supported by the evolution of science in different fields, from medicine to technology. The majority of successes have been achieved working under the assumption that good surgical outcomes are mainly a result of technical skills. This model, although correct, is not exhaustive and has left out a number of variables that affect outcomes, of which a number can be grouped under the label of non-technical skills, which is a subset of human factors.
Human factors “is the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance., the human performance” (IEA Definition) (1).
Non-technical skills are developed to facilitate a shared mental model between team members, teams and their operational environment. They include situation awareness, decision-making, communication, teamwork, leadership and performance-shaping factors. The importance of these non-technical skills has been highlighted during the investigations of serious accidents in many high-risk industries like aviation, nuclear and oil & gas, highlighting their contribution to error detection, trapping and mitigation.
The investment in technical skills in terms of time and financial resources has delivered an improvement in surgical outcomes. There is a risk that the investment in this area will reduce its return as the nature of surgical interventions has moved away from relatively simple, linear activities to more complicated and complex procedures. Therefore there is a need to create a shared mental model in this uncertain, complex and ambiguous environment.
There is an almost untapped opportunity to improve outcomes focusing on non-technical skills. In healthcare, there has been an under-investment of time and resources in human factors in a wider sense, and non-technical skills specifically, despite it being shown to be relevant in other high-risk industries and to have delivered extremely significant reductions of accidents.
This theoretical paper supports the adoption of a broader model of human performance as a function of technical and non-technical skills, and the cultural and organisational context where these are at play. We also aim to highlight a pathway to increase the investment in non-technical skills following the most updated evidence.
Focus on outcomes
The focus on outcome is not new to our profession; all national and international databases support the trend that moves the major outcomes towards improvement. We have progressively reduced mortality (2,3), through the comparison of surgical techniques, identification of the technique with best outcomes (low mortality, low morbidity, best long-term survival), implementation of the best techniques and consequent reduction of variability. Databases sponsored by national societies offer reassurance to patients and governing bodies that individual surgeons perform within an acceptable range. Low-performing surgeons are investigated and supported to bring outcomes within the accepted range. However, it is recognised that these are lagging indicators, to use a term from the safety world, and that we should be looking to develop leading indicators or practices if we truly want to improve patient safety.
Technology has helped in the standardisation of surgical practices. For example, the use of staplers has reduced the variability of outcomes associated with surgical skills in a number of steps. During a lobectomy procedure, the quality of closure of bronchi, veins and arteries and the completion of fissures has been standardised, and results have become consistently more reproducible independent of surgical skills.
Models of performance
We use models of the world to make sense of what is happening around us and to predict what is going to happen next. In the healthcare context, like in many other domains, we accept that observed outcomes in a socio-technical environment are a function of human behaviours.
OBSERVED OUTCOMES = f (BEHAVIOURS)
Kurt Lewin, a social psychologist in 1936, for the first time, defined human behaviours with this formula.
BEHAVIOURS = f (P,E)
Where P stands for the entirety of a person (e.g., his or her past, present, future, personality, motivations, desires, knowledge, skills) and E represents the physical and cultural environment in which they are operating.
Combining these two formulae, we can accept that observed outcomes are a function of the persona of the individual involved in the task, and of the environment in which the action takes place.
OBSERVED OUTCOMES = f (P,E)
When we analyse human performance while accomplishing a task, what we see is the expression of the persona through his or her skills.
OBSERVED OUTCOMES = f (SKILLS, E)
The Oxford Dictionary defines skill as the ability to do something well. In other words, it is an expression of the individual or team that achieves a pre-defined or expected outcome.
As highlighted by Lewin, skillful actions do not happen in a vacuum but in a pre-defined environment. The technical, operational and cultural environments in which the surgical team is operating will have an impact on outcomes. Such influencers of performance could be surgical instrument design, shift patterns, operating theatre layout, safety culture within the organisation or national culture. The importance of the environment/context is highlighted, for example, in the WITH model (see Figure 1) from the Institute of Nuclear Power Operations (INPO). This model emphasises error-producing conditions within an operational environment and covers work environment, individual capabilities, task/demands and human nature (4,5). These all come under the wider umbrella of human factors, system design and system interaction, and are outside the scope of this paper. Focusing on technical and non-technical skills development without addressing these other factors in a meaningful way will have a limited impact on patient safety and patient outcomes.

For simplicity, we will refer to these aspects as context rather than “E” (Environment) (6).
OBSERVED OUTCOMES = f (SKILLS, CONTEXT)
Within the context factor, we can include physical resources needed to perform the procedure, staffing, organisational guidelines, etc.
In the surgical community, surgeons undertake significant training and development over a long period to enable technical skills. The focus on technical aspects during training induces the subconscious acceptance of a simplified model of surgical performance where only a subset of skills (the technical one) seems to have relevance in determining outcomes.
OBSERVED OUTCOMES = f (TECHNICAL SKILLS, CONTEXT)
Once surgeons and healthcare providers have accepted this model, it is only natural to invest time and resources to improve outcomes by refining the surgical technical skills, by improving the supporting technology and the environment in which the surgical procedures are performed.
The pervasiveness of this simplistic model is also reflected in the training curricula for aspiring thoracic surgeons in most countries (7), which focus attention almost exclusively on developing technical knowledge and skills.
Creating more accurate models
As models are approximations of reality, the more accurate we can make them, the more relevant they are to the problems we are trying to solve. The model f (TECHNICAL SKILLS, CONTEXT) omits a number of variables that affect outcomes. Informal conversations among surgeons have identified that, frequently, the concept of luck has been left out of the equation when it comes to outcomes—especially as it could swing the difference between a good outcome and a bad one, once surgical skills have been fully developed. Ironically, this is counter to the reductionist view of controlling all the variables within the system by reducing complex tasks to individual steps and associated checks.
OBSERVED OUTCOMES = f (TECHNICAL SKILLS, CONTEXT, LUCK)
Luck is a signpost for variability of performance, uncertainty and the possibility of “black swans”. Some aspects of luck will be explored in the following paragraphs.
Black swans have been defined as events that come as a surprise, have a major effect and are often inappropriately rationalised after the fact with the benefit of hindsight (8). In the surgical domain, this could be a massive pulmonary embolism and consequent death of a patient on day two after a successful lobectomy.
Note that variability of performance should not be included under the label of luck, although this is psychologically more acceptable. Variability of performance is an aspect of technical skills and can be addressed through training and deliberate practice (9).
We can assume that luck is at play when:
- A chance occurrence affects a person or group (e.g., a patient or a surgical team);
- The chance occurrence causes a good or bad outcome;
- It is reasonable to assume that another outcome was possible (10).
For example, a patient has an anaphylactic reaction to an antibiotic in theatre, is then treated according to the most updated guidelines, but dies. This is an unlucky event because it fulfils the above criteria: it was a chance occurrence, it caused a bad outcome and it was reasonable to assume that a good outcome was possible. For the patient and surgical team involved in this event, we can consider it unlucky.
Luck can also play a part in positive outcomes. There are situations where bad things happen and the overall outcome is good out of sheer luck. During mortality and morbidity audits, when investigating good outcomes after bad events, it is worth adding the question “what worked well and were we lucky or good?” to the proceedings. Good, in this context, would be the result of a system that is able to fail safely because those within it had predicted the possibility of failure, and barriers were in place to reduce the impact of the event (6).
Randomness and luck are related. It is useful to think that randomness operates at the level of the system, while luck operates at the level of the individual.
Looking at anaphylaxis it occurs in approximately 4 out of 100,000 administrations of antibiotics (11). An effect of randomness is the order in which patients present anaphylaxis, as we do not know for certain which four patients from the 100,000, will manifest it. Patients are blinded to their own susceptibility to anaphylaxis, unless it has occurred to them before, and so at an individual level this could be thought of as unlucky.
In the formula we are developing, at a system level, if we assume that resources available are constant, luck can be expressed by randomness. This assumption is interesting, given that healthcare is resource-limited.
OBSERVED OUTCOMES = f (TECHNICAL SKILLS, CONTEXT, RANDOMNESS)
There are negative events that are not explained by this model. Surgical teams with high levels of technical skills are occasionally able to produce extremely negative outcomes. A famous case in the UK was the removal of the wrong kidney (12), but similar events continued to happen as shown in a report commissioned by NHS Improvement (13). In these situations, similar to other high-risk industries, the adverse outcomes seem to be related to the lack of effective non-technical skills. The list of investigations supporting the importance of non-technical skills in the causation and avoidance of accidents is constantly increasing (14,15). This leads to the next version of the formula.
OBSERVED OUTCOMES = f (TECHNICAL SKILLS, CONTEXT, RANDOMNESS, NON-TECHNICAL SKILLS)
Definition of technical and non-technical skills
As seen before, a skill has been defined as the ability to do something well. The adjective ‘technical’ means having special and usually practical knowledge, especially of a mechanical or scientific subject. In relation to surgery, the best way of identifying what technical skills are is to start with a list: suturing, dissecting, reviewing scans and identifying anatomical structures are all technical skills. Improvement in the technical aspects of the surgeon’s job can be supported by the application of deliberate practice (9) and the development of direct technology (e.g., staplers, robots, etc.) and supporting technologies e.g., anaesthesia, drugs and camera systems.
What falls under the non-technical skills for surgeons has been organised in a taxonomy by Yule et al. (16) and is summarised in a publication of the Royal College of Surgeons (Edinburgh) Non-Technical Skills for Surgeons (NOTSS) Handbook Vol. 1.2. (17).
This publication identifies the following non-technical skills:
- Situation awareness: the gathering and understanding of information, and the ability to project and anticipate future states.
- Decision-making: formulation of options, selection of the most favourable option, communication and implementation of the option and, ideally, the review.
- Communication and teamwork: the ability to exchange information and, based on it, the ability to establish a shared understanding of the situation at hand; the ability to coordinate and collaborate within and across teams.
- Leadership: the ability to set and maintain standards, support others, and cope with pressure.
Performance-shaping factors like stress and fatigue are not included in the NOTSS Handbook, but Flin et al. highlight their importance as they can impact the effectiveness of both technical and non-technical skills (18). Stress and fatigue reduce the likelihood that errors will be detected, trapped and mitigated and, therefore, could have a significant impact on outcomes. These performance-shaping factors fit within the operational ‘context’.
OBSERVED OUTCOMES = f (TECHNICAL SKILLS, CONTEXT, RANDOMNESS, NON-TECHNICAL SKILLS, STRESS|FATIGUE)
The impact of technical skills on outcomes
During the last few decades, the continual improvements in technical skills and technological interventions within healthcare have led to progressive improvements in outcomes.
Although we have seen the progressive reduction of mortality in our specialty, we cannot avoid noticing that, within healthcare, there are still a number of patients dying unnecessarily. A paper published in 2016 in BMJ suggests that medical error is the third cause of death after heart disease and cancer. The study might be underreporting the number of deaths because of medical error. However, using the attribution ‘medical error’ does not necessarily improve learning, as it is a catch-all term that does not define how the error was propagated through the system, nor how it could have been prevented. Errors which lead to a fatality highlight the latent or potential lethality within the system and could be thought of as an outcome and not necessarily a cause of death. This might appear controversial, but any system which has a risk of death has a level of lethality within it, and it is only through humans creating safety that that lethality is kept at bay.
Error is a form of outcome. It is the unintentional deviation from an expected outcome. Conklin emphasises in his book that “these unintentional deviations are not detectable as deviations while the deviation is occurring” (6). Consequently, errors are not a choice, just one of the normal expected, although not desired, outcomes of the formula developed so far.
ERROR = f (TECHNICAL SKILLS, CONTEXT, RANDOMNESS, NON-TECHNICAL SKILLS)
When we look at errors as one of the possible outcomes, then the importance moves from avoiding errors to being “robust enough to recover effectively and gracefully” (6). Flight crews have formalised this process by moving beyond general non-technical skills to understanding what errors are likely to occur in the next activity e.g., taxi, take-off or approach and landing, and trapping or putting an activity in place to mitigate it. Crew recognise that errors cannot be removed from a system, but error-producing conditions are predictable. This process is known as “Threat and Error Management”.
When we look at death, we are only looking at the tip of an iceberg. Morbidity is significantly more common and, while the correlation between minor incidents, major incidents and fatalities in Heinrich/Bird’s triangle has been debunked, morbidity events provide significant opportunities for learning as ‘medical error’ will be present in these events too (19).
MORBIDITY = f (TECHNICAL SKILLS, CONTEXT, RANDOMNESS, NON-TECHNICAL SKILLS)
The number of adverse events reported within the NHS is increasing every year, and the same effect is evident in all healthcare systems currently recording these events.
The increasing number of reported events may be due to improving reporting. However modern healthcare systems are more complex and resources are reducing; therefore errors may be more likely. It is more plausible that it is combination of both theories.
To counter this rise, governing and regulatory bodies are investing in programmes to reduce the number of adverse outcomes through the use of evidence-based medicine and practice. This has led to standardised and optimised techniques which are widely deployed and available to the patient population (minimally invasive colorectal resections experienced in UK). However, such evidence-based practice is limited when it comes to non-technical skills.
Improving outcomes: return on investment and law of diminishing returns
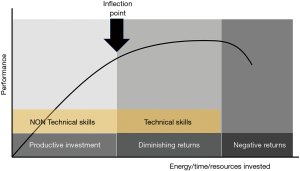
When we attempt to improve performance, the relationship between investment of resources and performance tends to be linear when the performance is really poor (see Figure 2). A small investment at this stage increases performance. Progressive investments increase performance in a linear way until an inflection point is reached. Prior to this point, the investment is productive. After the inflection point, we see a diminishing return and the curve becomes progressively flatter until it reaches a plateau. If we continue investing, it is likely that we will reach a point of diminishing returns. Performance will not increase with further investment and will very likely progressively decrease.
It is the opinion of the authors that the investment on the technical side i.e. technical skills development and technological solutions, has passed the point of inflection and entered the diminishing return phase. Looking at this through a different lens—that of human factors and non-technical skills—because of the lack of attention and, subsequently, the associated lack of investment, non-technical skills are still in the productive investment phase.
Improving outcomes: the importance of zero in multiplicative system
The formula we have slowly developed recognises a number of factors that have an effect on the outcomes. The factors within brackets are separated by a comma. This use of commas is intentional.
OBSERVED OUTCOMES = f (TECHNICAL SKILLS, CONTEXT, RANDOMNESS, NON-TECHNICAL SKILLS, STRESS|FATIGUE)
If the effect of the different factors is addictive (represented in the following formula by the sign “+”), then it is possible to deliver positive outcomes even if one of the factors is equal to zero.
OBSERVED OUTCOMES = f (TECHNICAL SKILLS + CONTEXT + RANDOMNESS + NON-TECHNICAL SKILLS + STRESS|FATIGUE)
This additive process introduces a bias as it may lead us to think that ‘non-technical skills’, ‘context’ and the impact of ‘stress/fatigue’ could be added, or not, to technical skills and still have a positive outcome. If the coefficient is between zero and one, the effect will be reductive and not positive. Consequently, we need to recognise that there are situations where ‘non-technical skills’ and ‘context’ could have a multiplicative effect.
OBSERVED OUTCOMES = f (TECHNICAL SKILLS × CONTEXT × RANDOMNESS × NON-TECHNICAL SKILLS × STRESS|FATIGUE)
If this is the formula, then we can see that if non-technical skills, context or stress/fatigue equal zero, then these factors are able to cancel the effect of all the other factors.
Ineffective situational awareness (non-technical skill coefficient = zero), for example, may allow the perfect execution of a surgical procedure on the wrong side (wrong kidney removed) and nullify the positive impact of all the technical skills and context. The same applies for context when time pressures, fatigue, operating room design and a lack of just culture impact human performance, leading to a suboptimal outcome. While teams may have great technical skills and effective non-technical skills, the positive outcomes can easily be destroyed if stress/fatigue and the context (organisational level) are not managed effectively.
As we can see, a lack of technical skills also has a multiplicative effect and creates unwanted outcomes. However, this occurrence is significantly less likely because of the way in which the training and accreditation of surgeons is designed. It is very unlikely for a surgeon to finish training, gain accreditation and be allowed to practice in the absence of technical skills (technical skills coefficient = zero).
Focus on non-technical skills in high-risk industries and outcomes
The importance of non-technical skills was originally noticed in the ‘70s and ‘80s. Investigations conducted to understand the reason behind catastrophic events in high-risk industries like nuclear and aviation showed that there was no lack of technical skills, but a failure in communication, situation awareness, decision-making and teamwork. Among those events were the Tenerife crash of two Jumbo Jets on the runway in 1997, the Chernobyl nuclear accident in 1986 and the Piper Alpha oil platform in 1988. While aviation started formal programmes for crew resource management (CRM) in the 1990s, it wasn’t until after the Macondo disaster (Deep Water Horizon) that the Institute of Oil and Gas Producers (IOGP) published Documents 501, 502 and 503 (20) which detailed Well Operations, CRM procedures and training for Oil and Gas workers.
Among the high-risk industries, aviation has achieved dramatic improvement of its safety profile. One of the reasons for this is the training of pilots and crew members in CRM. The benefits of CRM are seen in normal operations to prevent error, but they have significant benefits when in uncertain, complex and ambiguous situations, because it allows a shared mental model to be created within the operational team. Furthermore, CRM:
- Is a set of planning and operational procedures for use in environments where human errors can have devastating effects;
- Is used primarily for improving performance, leading to increased safety;
- Focuses on interpersonal communication, leadership and decision-making.
However, CRM is part of the wider human factors domain and all personnel working airside are mandated to have periodic human factors training to understand how human error is propagated through the system and what they can do to predict, trap and mitigate it.
Aviation, as an example of success, has reduced the number of accidents and become one of the safest industries. Still, it is difficult to demonstrate the link between CRM training and outcomes (21).
It should be noted that transferring CRM from one domain or culture to another has limitations. For example, when CRM programmes from the US were taken to the Far East, they were not as effective because of national cultures impacting individual and team performance (22).
Focus on non-technical skills in healthcare and outcomes
Despite numerous case studies, accident reports and research papers showing the benefit of the application of human factors and non-technical skills programmes, no coherent programme for the application of non-technical skills has been developed and deployed within the NHS. This is despite the constant pillars of CRM—situation awareness, decision-making, communication and teamwork and leadership—that have been adopted in healthcare.
For non-technical skills programmes to be effective, they need to be part of colleges’ training programmes, achieve a critical mass within the operational environment and require the leadership from government to healthcare units to be proactive in their support and development.
When we look at the currently published literature regarding the link between patient outcomes and non-technical skills, we can group the measured outcomes in four domains:
- Efficiency of patients’ care (time to perform);
- Complications;
- Length of stay;
- Survival/mortality.
A small number of studies (23,24) shows that CRM training improves efficiency of patient care but has no effect on mortality or other clinical outcomes. Two other studies (25,26) show that adopting HF/CRM programmes can have a positive effect on patient safety and financial resources. Both papers underline the need for an upfront investment of time and financial resources. One study (27) shows that, after CRM training, the mortality for paediatric cardiac arrest dropped and the survival improved from 33% to 50%.
Other authors (28) published an improvement of 37% in perinatal outcomes after non-technical skills simulation training.
A meta-analysis that looks at NTS in surgical teams, published in 2018 (29), shows that there are a small number of heterogeneous and mostly underpowered studies that look at the relationship between patient outcomes and NTS training. This analysis failed to identify a strong improvement in patient outcomes after NTS training, although the NTS skills of the team trained were improving. The authors suggest that improvement in patient outcomes could be demonstrated in well-conducted, appropriately powered prospective trials.
Other supporting evidence to NTS comes from the 4th National Audit Projects (14,15). This investigates major airways complications in the UK and confirms that human factors have played a significant role. More specifically, latent threats are predisposed to loss of situational awareness and poor decision-making (30).
One of the problems with delivering change regarding human behaviour and organisational performance is the need to make large investments in time and resources, and this might be why there is a lack of published literature showing how CRM or NTS improvement programmes can positively impact patient outcomes. Two research projects, one from Moffatt-Bruce et al., and another from Haerkens et al., have shown that, with such investment, significant benefits can be realised. Haerkens et al. showed that the standardised mortality ratio decreased from 0.72 in the baseline year to 0.60 in the post-implementation year, with cardiopulmonary resuscitation success rate increased from 19% to 55% and 67%. Moffat-Bruce et al. showed that the total number of adverse events avoided was reduced by 25.7%. The savings ranged from a conservative estimate of $12.6 million to as much as $28.0 million with an overall ROI for CRM training in the range of $9.1–24.4 million.
Morally, patient outcomes are important. However, most healthcare systems are run as businesses and, therefore, financial and resource outcomes also need to be addressed if a paradigm shift regarding adoption is to occur. Kuhn’s paradigm shift model (31) highlights that, until a model crisis is reached where the current paradigm is unable to match the reality of the problems faced, the current paradigm will be maintained. It is not clear what that crisis will be for healthcare to adopt human factors and non-technical skills in a more coherent manner, but limited financial resources and public outcry might be the trigger.
Developing non-technical skills
The way which we develop surgical skills is very different from the way in which we develop non-technical skills. When we look at an individual who is starting surgical training, he/she usually has no surgical skills prior to college, although they may have developed skills that can be the foundation of his/her surgical career. For example, a person who has spent time improving his/her fine motor skills will be at an advantage during surgical training. Most people will have an acceptable baseline of these skills that they have acquired during the previous years of their life, investing time in playing, practicing hobbies and engaging in normal daily activities.
Individuals starting surgical training will also have developed a degree of non-technical skills that have allowed them to survive normal daily tasks, school, university and they will be practiced at different levels of competence.
By examining the skillsets of those who enter surgical training programmes, we can see that the range of competencies in the non-technical area is much broader than in the technical. For this reason, non-technical skills are one of the major sources of variation in outcomes.
The lack of focus on non-technical skills during surgical training allows aspiring surgeons to end their surgical training without any real improvement of their non-technical skills. The training in technical skills moves the aspiring surgeons up towards proficiency; however, there is no similar transformation regarding non-technical skills.
The causal link between non-technical skills training and improvement of outcomes is difficult to demonstrate. Attempts in healthcare have shown differing degrees of success for a variety of reasons, not least the high number of confounding variables involved. Interestingly, this causal link has been hard to prove in aviation, where improvement in safety has been attributed to non-technical skills and human factors/ergonomics (21,22).
How to ensure that training drives changes in the workplace
Wood et al. (32) recommend the use of NOTSS as the gold standard for training individuals. They also recommend Oxford NOTECHS II as a training tool in non-technical skills for teams.
One of the main limits of non-technical skills training in healthcare is that the majority of resources are used in the delivery development of the training and very few are allocated to sustain behaviour in the workplace. A study by Brinkeroff in the workplace suggests that if enough resources are invested to support new behaviour in the workplace after training, the chances of sustaining this behaviour are in the range of 80%, while, if few or no resources are invested, the chances of sustaining new behaviour are as low as 15%.
How do we know when the training we have delivered is effective? Kirkpatrick developed a model identifying four levels at which we can evaluate training programmes. The first is the reaction of the participants to the training; they answer the question, “Did they like it?” The second answers the question, “Did I learn something?” The third assesses if there have been changes in behaviour when the trainees return to the workplace. The fourth is the most important, and assesses if the training delivers the final results that the organisation was looking for.
If a healthcare professional was attending non-technical skills training, he/she would say:
- Level I: “I like the training and I found it engaging”;
- Level II: “I’ve learnt something”. This statement could be objectively assessed to ensure that the learning has taken place, using a validated scoring system like NOTSS;
- Level III: “I routinely use what I have learned during the non-technical skills training in my day-to-day job”. Objective assessment of new behaviours could be performed in the workplace during audits. For example, consistent use of checklists and closed-loop communication;
- The organisation or sponsoring professional body should be able to assess level IV;
- Level IV: the hospital should be able to see a reduction in adverse events for the teams who have attended training.
A study (33) looked at the transfer of learning from “classroom” to workplace using the above classification. The authors identified nine studies in total. Out of these, four studies measured the transfer of simulation-based CRM learning into the clinical setting (Kirkpatrick level 3) and highlighted that adding simulation was more effective than didactic teaching. Five studies tried to look at patient outcomes (Kirkpatrick level 4). Only one found that simulation-based CRM training had a clearly significant impact on patient mortality (27).
Conclusions
Both positive and negative outcomes are multifactorial and can be summarised by the following formula.
OBSERVED OUTCOMES = f (TECHNICAL SKILLS, CONTEXT, RANDOMNESS, NON-TECHNICAL SKILLS)
A mnemonic aid for thoracic surgeons is “ThoRaCotomy or Not”.
OBSERVED OUTCOMES = f (ThoRaCotomy or Not)
T = technical skills;
R = randomness;
C = context;
Not = non-technical skills.
In healthcare, outcomes are frequently analysed in a reductionistic way, focusing on the technical aspects (performed procedure, administered drug, etc.) and patients’ physical characteristics. The lack of focus on non-technical skills, context and effect of randomness blinds us to a significant portion of possible causal explanations. In other high-risk industries, the exploration of these areas has delivered a significant improvement in performance. The evidence in healthcare is still lacking and is mainly limited to the report of investigations that have identified the lack of non-technical skills as likely precursors of severe adverse events limited to small heterogeneous studies.
The above formula and mnemonic might help surgeons when analysing outcomes to avoid the immediate tunnel vision effects of focusing on technical skills.
The identification of error precursors is important. Using tools similar to the WITH model from the nuclear domain, or the threat and error management process in aviation, will help thoracic surgeons and associated surgical teams to identify situations where there is a higher risk of error and reduce the risk of failing. In aviation, technical skills are taken for granted because of the ongoing professional competency assessments. Consequently, it is when randomness and context start to significantly shape the activity, that effective non-technical skills come into their own regarding outcomes, and can add a large multiplicative factor to the function if they are well developed.
A cultural change (see Figure 3) associated with effective training, if incorporated in properly designed studies, will offer the evidence to support the investment of resources. However, training delivery is not a simple process and can be likened to situational leadership. One size does not fit all, despite this being the wishes of organisation, who would like to have simple repeatability.

One of the ways we have to improve performance is to reduce variability and, ideally, move the average performance towards higher standards. However, the improvement in standards should not just be limited to technical skills where tangible improvements are more easily identified, but also in non-technical skills and improving the operational context, such as culture and system design. It is believed that improvements in this area will have significant multiplicative coefficients when it comes to outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Association IE. Definition of ergonomics (or human factors). Available online: https://www.iea.cc/whats/. Accessed 13/02/2019 2019.
- Ireland SfCSiGB. National thoracic surgery activity & outcomes report. Henley-on-Thames: Dendrite Clinical Systems, 2008-2012.
- Surgery ESoT. Silver Book: Database Annual Report. ESTS; 2015.
- Swinton T. Introducing the WITH model. CRJ Series 5 - Introducing the WITH model. Paradigm Human Performance 2018.
- Energy USDo. Human Performance Improvement Handbook. Washington: U.S. Department of Energy; 2009.
- Conklin T. The 5 Principles of Human Performance: A contemporary update of the building blocks of Human Performance for the new view of safety. Independently published (January 23, 2019); 2019.
- (SAC) JCoSTJCSAC. Curriculum for Cardiothoracic Surgery. 2012.
- Taleb NN. The black swan: the impact of the highly improbable. Rev. ed. London: Allen Lane; 2011.
- Ericsson KAH, Robert R, Kozbelt A, et al. The Cambridge handbook of expertise and expert performance. Cambridge: Cambridge University Press, 2018.
- Mauboussin MJ. The success equation: untangling skill and luck in business, sports, and investing. Boston: Harvard Business Review Press, 2012.
- Torjesen I. Antibiotics are the main cause of life threatening allergic reactions during surgery. BMJ 2018;361:k2124. [Crossref] [PubMed]
- Dyer O. Doctors suspended for removing wrong kidney. BMJ 2004;328:246. [PubMed]
- Burnett S. Surgical Never Events: Learning from 38 cases occurring in English hospitals between April 2016 and March 2017: NHS Improvement, London IC; 2018.
- Cook TM, Woodall N, Frerk C, et al. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth 2011;106:617-31. [Crossref] [PubMed]
- Cook TM, Woodall N, Harper J, et al. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. Br J Anaesth 2011;106:632-42. [Crossref] [PubMed]
- Yule S, Flin R, Maran N, et al. Surgeons' non-technical skills in the operating room: reliability testing of the NOTSS behavior rating system. World J Surg 2008;32:548-56. [Crossref] [PubMed]
- Yule S. The Non-Technical Skills for Surgeons (NOTSS) System Handbook v1.2. Edinburgh: The Royal College of Surgeons of Edinburgh, 2012.
- Flin RH, O'Connor P, Crichton MD. Safety at the sharp end: a guide to non-technical skills. Aldershot: Ashgate, 2008.
- Elliott J. Safety I and safety II: the past and future of safety management. Ergonomics 2016;59:859-60. [Crossref] [PubMed]
- Producers IAoOG. Documents 501, 502, 503. International Association of Oil & Gas Producers. Available online: https://www.iogp.org/bookstore/product/guidelines-for-implementing-well-operations-crew-resource-management-training/. Accessed 14/02/2019, 2019.
- Salas E, Burke CS, Bowers CA, et al. Team Training in the Skies: Does Crew Resource Management (CRM) Training Work? Hum Factors 2001;43:641-74. [Crossref] [PubMed]
- Helmreich RL. Fifteen Years of the CRM Wars: A Report from the Trenches Sidney, Australia: The Australian Aviation Psychology Association; 1993.
- Capella J, Smith S, Philp A, et al. Teamwork training improves the clinical care of trauma patients. J Surg Educ 2010;67:439-43. [Crossref] [PubMed]
- Steinemann S, Berg B, Skinner A, et al. In situ, multidisciplinary, simulation-based teamwork training improves early trauma care. J Surg Educ 2011;68:472-7. [Crossref] [PubMed]
- Moffatt-Bruce SD, Hefner JL, Mekhjian H, et al. What Is the Return on Investment for Implementation of a Crew Resource Management Program at an Academic Medical Center? Am J Med Qual 2017;32:5-11. [Crossref] [PubMed]
- Haerkens MH, Kox M, Lemson J, et al. Crew Resource Management in the Intensive Care Unit: a prospective 3-year cohort study. Acta Anaesthesiol Scand 2015;59:1319-29. [Crossref] [PubMed]
- Andreatta P, Saxton E, Thompson M, et al. Simulation-based mock codes significantly correlate with improved pediatric patient cardiopulmonary arrest survival rates. Pediatr Crit Care Med 2011;12:33-8. [Crossref] [PubMed]
- Riley W, Davis S, Miller K, et al. Didactic and simulation nontechnical skills team training to improve perinatal patient outcomes in a community hospital. Jt Comm J Qual Patient Saf 2011;37:357-64. [Crossref] [PubMed]
- Leuschner S, Leuschner M, Kropf S, et al. Non-technical skills training in the operating theatre: A meta-analysis of patient outcomes. Surgeon 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Jones CPL, Fawker-Corbett J, Groom P, et al. Human factors in preventing complications in anaesthesia: a systematic review. Anaesthesia 2018;73 Suppl 1:12-24. [Crossref] [PubMed]
- Kuhn TS, Hacking I. The structure of scientific revolutions. Fourth edition. ed. Chicago; London: The University of Chicago Press, 2012.
- Wood TC, Raison N, Haldar S, et al. Training Tools for Nontechnical Skills for Surgeons-A Systematic Review. J Surg Educ 2017;74:548-78. [Crossref] [PubMed]
- Boet S, Bould MD, Fung L, et al. Transfer of learning and patient outcome in simulated crisis resource management: a systematic review. Can J Anaesth 2014;61:571-82. [Crossref] [PubMed]