Uniportal complete video-assisted thoracoscopic lobectomy with systematic lymphadenectomy
Introduction
When it comes to perspectives in complete video-assisted thoracoscopic surgery (cVATS), it has become a consensus in thoracic community that is to further reduce the number and the length of the incisions (1). In Jun 2011, Gonzalez Rivas first report uniportal cVATS lobectomy which becomes a milestone in the development history of VATS lobectomy (2). Perhaps the demand for increasingly more minimally invasive surgical approaches is even more important within the Chinese culture, uniportal VATS development has grown in popularity in mainland recently.
However, uniportal approach poses several major challenges to cVATS lobectomists (2): (I) interference of the thoracoscope, stapler and the instrumentation in and out of the thoracic cavity? (II) whether the field of vision is enough or not without the other 1-3 ports to improve the exposure? (III) the optimal stapler introduction angle especially for upper and middle lobes resection? (IV) more importantly, the oncologic validity of uniportal procedures as well as the reduction of postoperative morbidity? This video demonstrates a case undergoing uniportal cVATS lobectomy with systematic lymphadenectomy for lung cancer. We here describe our technique for uniportal approach by using a combination of double-jointed and endoscopic instruments.
Clinical data
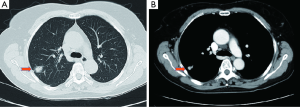
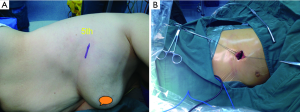
A 64-year-old female presented with a 2.0 cm × 2.0 cm × 1.0 cm nodule in posterior segment of right upper lobe and a ground glass opacity (GGO) in the left upper lobe on computed tomographic (CT) (Figures 1,2) was admitted in our institute on March 16th, 2014. The patient underwent preoperative staging and cardiac and pulmonary function assessment. PET-scan indicates no signs of metastasis. Under general anesthesia with double lumen tube, the patient underwent uniportal cVATS lobectomy for right upper lung tumor on March 19th, 2014 (Figure 3). The final pathologic TNM staging is T1aN0M0 (IA). Regular follow up was initiated for the GGO in the left upper lobe.

Operative techniques
Patient positioning, placement of the single incision
The patient is positioned in full lateral decubitus position with slight flexion of the table at the level of the mid-chest, which allows slight splaying of the ribs to improve exposure in the absence of rib spreading. This is similar to conventional VATS procedures. All lobectomies and segmentectomies were underwent via the 5th intercostal space about 3.5-4.5 cm long. Plastic wound protector was not used now and soft tissues are retracted by silk only to prevent the lung from expanding when suction is used. The 30° 10 mm thoracoscope (5 mm ever used) is placed in the posterior part of the above incision and fixed by a rubber band (Figure 4).
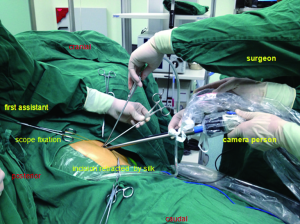
Different stance for the operating personnel and instruments
We now use a combination of endoscopic and double-jointed instruments and some specially adapted for uniportal cVATS including long and short curved suction tube and ring forceps (Figure 5). An articulating endoscopic linear cutter is preferred.
The operator and the scope holder always stand anterior to the patient whether the operator stands caudally or cranially varies depending on the procedures in the lower or upper thoracic cavity. The first assistant stands posteriorly responsible for the macro exposure. The surgeon always holds suction tube in the left hand for micro and dynamic exposure while in the right hand almost are the electrocautery or harmonic scalpel. From posterior to anterior at the incision level lies in turn the scope, the long curved ring forceps containing gauze for macro exposure, the energy devices and the suction tube (Figure 6).
Exploration
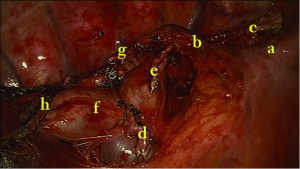
We begin the procedure with an exploration of the pleural cavity. The tumor is identified in the posterior segment of the right upper lobe. The frozen section analysis after wedge resection revealed infiltrating adenocarcinoma, so we proceed to right upper lobectomy with systematic lymphadenectomy.
Division and transection of truncus anterior artery
First cut open mediastinal pleura in the anterior hilum and underneath the arch of the azygos vein. Then dissect and indentify the gap between the superior pulmonary vein and truncus anterior artery. The lymph nodes are cleared at the same time. Dividing the truncus anterior artery first is often recommended in order to facilitate the insertion of the staplers for the upper lobe vein. We strongly recommend the use of silk ligation and hemolock in cases where the angle for stapler insertion is not optimal especially for the left upper lobectomy. The posterior ascending artery can be divided separately or at last together with the fissure.
Division and transection of superior pulmonary vein
The location of endostapler and the thoracoscope are interchangeable between two incisions in biportal approach. In uniportal approach, first dividing the artery is most commonly used. In unusual cases, dividing the superior vein following the truncus anterior artery and then the upper bronchus is used. Sometimes divide the minor fissure help first staple the superior vein from anterior and superior to the posterior and inferior direction.
Division and transection of right upper lobe bronchus
Identifying and clearing the lymph nodes between the upper and intermediate bronchus first. The bronchus can be transected via anterior or posterior approach by a stapler while the former is more convenient because of no need to expose the lung anteriorly.
Dissection of the horizontal fissure and the posterior halves of the oblique
The distal lymph nodes at the second carina should be dissociated to the distal end of the bronchus, and then removed en bloc with the right upper pulmonary lobe. The above fissures can be divided using stapler last. The lobe is extracted using a specimen retrieval bag.
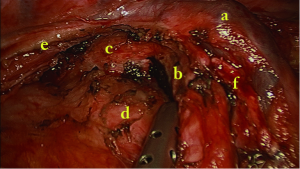
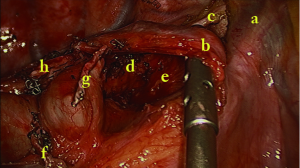
Mediastinal lymph node (MLN) dissection
Move the operating table anteriorly. Systematic lymph node dissection using en bloc excision, instead of systematic sampling, is applied for the removal of 2, 4, 7, 8 and 9 MLNs. We use the same method as in the biportal approach (4). Cut open mediastinal pleura by a “∩” shaped incision for 7th, a “⊿” above azygos vein and “– ” beneath azygos vein for 2th and 4th which greatly simplify the en bloc MLNs dissection (Figures 7,8,9).
Leakage testing, intercostals nerve blockade, insert drainage tube and incision closure
The lung is re-expanded for air leakage testing for the bronchial stump and the pulmonary resection margin. Finally a single 24# chest tube with enough side holes is placed in the posterior part of the incision up to the tip of the thoracic cavity (Figure 10).

Comments
After sustaining and rapid evolution for more than two decades, VATS has permeated our thoracic surgical practice and now will develop in depth towards a next level of minimally invasive surgery (MIS) (5). Irrespective of generation gaps and diversified perception within thoracic community, more and more surgical teams are adapting to this new era. Since Diego from Spain optimize uniportal cVATS major pulmonary resections, uniportal approach development has become an increasingly popular approach to manage thoracic surgical diseases because of the reduced access trauma and better cosmesis, with several centres in Hong Kong, Taiwan, Singapore, Mainland China and Korea beginning to perform uniportal VATS major lung resections (5-9).
From June 2012, more than 160 cases of uniportal cVATS procedures have been accomplished in our center. On 16th August 2013, we performed the 1st uniportal left lower lobectomy for bronchiectasis; on 26th November 2013, the 1st bilateral same-stage single-port thoracoscopic right upper lobectomy for lung cancer and left lower lobectomy for destroyed lung caused by bronchiectasis; on 18th December 2013, the 1st uniportal right lower basilar segmentectomy; on 6th March 2014, the 1st combined uniportal right upper lobectomy and right lower superior segmentectomy for lung cancer. Until now, we have performed 33 cases of uniportal cVATS lobectomy and 16 cases of segmentectomy (unpublished).
After all, cVATS lobectomy through a single incision is a challenging technique for most thoracic surgeons especially those without experiences in biportal procedures. We surely believe Shenzhen People’s Hospital experience partially combat the above obstacles and flatten the learning curve of uniportal approach.
(I) Interference of the thoracoscope, stapler and the instrumentation in and out of the thoracic cavity?
Initially, we use endoscopic and open-surgery instruments, 30° 5 mm thoracoscope and plastic wound protector. All the devices were crowded at the incision level and in and out of the thoracic cavity which require adequate patience and coordination between surgeon and camera person. Now, we abandon the use of plastic wound protector which leave much more space at the incision level. More importantly, certain modified tools are very helpful in the execution of uniportal procedures. The double-jointed and endoscopic instruments and articulating endostaplers contribute to avoid interference of the thoracoscope and the instrumentation. It is critical for adjust different stance for the operating personnel. The advantage of leaving the camera person in coordination with the surgeon anteriorly is that the vision is directed to the target tissue, bringing the instruments to address the target lesion from a straight perspective, thus we can obtain similar angle of view as for open surgery. Yet triportal VATS forces the surgeons to an unnatural eye to hand coordination compared to what they are used to in open surgery. The sagittal, caudo-cranial approach of uniportal cVATS amends this problem by letting the surgeon work along a plane he/she is mostly accustomed to in open (10). We have tried three cases of uniportal cVATS lobectomy via 3-dimension imaging system giving us the impression of raising one’s head and operating “open” surgery.
(II) Whether the field of vision is enough or not without the other 1-3 ports to improve the exposure?
With experiences from biportal approach and uniportal approach for minor procedures, we learned that adequate exposure of the lung is mandatory in order to successfully access the interested lobe. The first assistant stands posteriorly responsible for the macro exposure. The surgeon always holds suction tube in the left hand for micro and dynamic exposure while in the right hand almost are the electrocautery or harmonic scalpel. The camera person leaves the scope displaying a close-up view of the target tissue. For all the team members and his devices, each does his part and work together and then contribute to good exposure.
(III) The optimal stapler introduction angle especially for upper and middle lobes resection?
Uniportal cVATS upper lobectomies are usually more difficult than lower obectomies in uniportal approach (11). The difficulty is mainly based on the sharp angles that are required to use instruments and staplers. Adjust the order for division of different hilar structures is conducive to access the target. For right upper lobectomy, the most common surgical steps are truncus anterior, upper vein, posterior ascending artery, upper bronchus and fissure which are similar to those of left upper lobectomy. The two strategies mentioned above for dividing superior pulmonary vein in unusual cases is helpful sometimes. But we strongly recommend placing hemoclips and ligation when there is no good angle for the stapler.
(IV) More importantly, the oncologic validity of uniportal procedures as well as the reduction of postoperative morbidity?
MLN dissection is the most critical point for lung cancer and is a prevalent concern relates to the ability of thoracoscopic operations to achieve adequate staging (12). To my knowledge, long-term oncologic outcomes including lymph node dissection efficacy, local recurrence, and survival after uniportal approach for lung cancer are lacking. Based on our own experience (4,8) and review from the literature (2,6,7), we surely believe MLN assessment in patients who underwent uniportal cVATS lobectomy was as effective as in those who underwent traditional cVATS lobectomy in experienced centers, with no difference in number of N2 LN stations or total number of LN stations resected.
In conclusion, uniportal cVATS lobectomy with systematic lymphadenectomy is technically safe and feasible and alternative approach to conventional thoracoscopic lobectomy in lung cancer treatment. The issues of patient acceptability, the cosmetic and oncologic results, and cost-effectiveness remain to be determined in the future through multi-institution randomized controlled trials and long-term follow-up.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Rocco G. VATS and Uniportal VATS: a glimpse into the future. J Thorac Dis 2013;5:S174. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Wang GS, Wang Z, Wang J, et al. Uniportal cVATS lobectomy for lung cancer. Asvide 2014;1:247. Available online: http://www.asvide.com/articles/259
- Wang GS, Wang Z, Wang J, et al. Biportal complete video-assisted thoracoscopic lobectomy and systematic lymphadenectomy. J Thorac Dis 2013;5:875-81. [PubMed]
- Ng CS. Uniportal VATS in Asia. J Thorac Dis 2013;5:S221-5. [PubMed]
- Tam JK, Lim KS. Total muscle-sparing uniportal video-assisted thoracoscopic surgery lobectomy. Ann Thorac Surg 2013;96:1982-6. [PubMed]
- Wang BY, Tu CC, Liu CY, et al. Single-incision thoracoscopic lobectomy and segmentectomy with radical lymph node dissection. Ann Thorac Surg 2013;96:977-82. [PubMed]
- Wang GS, Wang Z, Wang J, et al. Uniportal complete video-assisted thoracoscopic surgery: a retrospective single-institution series of 106 cases. Chin J Endoscopy 2014;20:118-23.
- Kang do K, Min HK, Jun HJ, et al. Single-port Video-Assisted Thoracic Surgery for Lung Cancer. Korean J Thorac Cardiovasc Surg 2013;46:299-301. [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5:S214-6. [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Thoracoscopic lobectomy through a single incision. Multimed Man Cardiothorac Surg 2012;2012:mms007.
- Amer K. Thoracoscopic mediastinal lymph node dissection for lung cancer. Semin Thorac Cardiovasc Surg 2012;24:74-8. [PubMed]