
Bone cement is a suitable treatment for sternal reconstruction in patients with recurrent sternal wound infections
Introduction
Sternal wound infection (SWI) is a common complication of cardiovascular operations performed by median sternotomy, with an incidence rate of about 0.5–8% (1-4). As a challenging problem, it often prolongs hospital stay and increases medical cost. The infection can affect vital mediastinal organs, and improper treatment may lead to the death of patients. Currently, SWI is mainly treated by debridement and reasonable wound healing, which includes wire re-fixation, vacuum sealing drainage (VSD), and tissue flap transplantation (5). However, there is no widely recognized treatment for recurrent SWI accompanied by sternal defect after failed tissue flap transplantation.
Case presentation
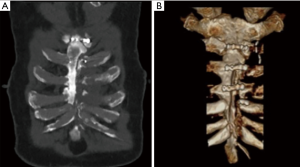
A 52-year-old male patient underwent coronary artery bypass grafting through median thoracotomy 18 months ago. He developed SWI and experienced delayed wound healing after the procedure, with a 6-cm defect in the anterior chest wall. He had received thoracic wall debridement and suture + skin flap transplantation + repair of chest wall defect in the department of plastic surgery and the department of burns in another hospital; one month later, he underwent thoracic wall wound debridement + VSD due to poor wound healing. Although symptomatic treatments including antimicrobials and glucose-lowering therapy were applied after these surgeries, wound healing was not improved. Computed tomography (CT) and three-dimensional reconstruction showed a 5.6 cm × 6.2 cm sternal defect at the lower segment of the sternum (Figure 1). The patient had a history of hypertension for 15 years, which was treated by oral administration of nifedipine, irbesartan, and metoprolol, and his blood pressure was 126/75 mmHg at admission. He had a history of type 2 diabetes mellitus for 10 years, which was managed by subcutaneous insulin injection, and his blood glucose level was 7.2 mmol/L, HgbA1C was 6%. He received a pancreatic surgery 10 years ago. He also had a history of uremia for 8 years, which was managed by long-term hemodialysis.
A second muscle flap, utilizing a different blood supply to the flap, would come with an increased risk of failure given the failure of the prior flap and the patient's co-morbidities including diabetes. Therefore, we performed radical treatment of osteomyelitis on the anterior chest wall, removal of the internal fixation of the sternum, and bone cement filling, followed by reconstruction of the sternum and primary closure. After general anesthesia, the patient was in a supine position. A spindle-shaped incision was made on the wound surface of the anterior chest wall (Figure 2A). The decaying meat on wound surface was extensively removed till the fresh tissue on the surface of the sternum was exposed. After the rigid plate and screws on the surface were removed, a 6-cm sternal defect was visible at the lower segment of the sternum. The infected bone on the surface was removed by a rongeur. Then, the wound was washed repeatedly with hydrogen peroxide, iodophor, and normal saline, and the surgical instruments were changed and cleaned. An orthopedic surgeon injected bone cement (Palacos R, Germany) containing vancomycin (250 mg) into the sternal defect, during which the heart surface was covered with a wet cotton pad to prevent the bone cement from burning the cardiac muscles. The cotton pad was removed after the sternal reconstruction was completed. The bone cement surface was smoothed with the sternum (Figure 2B,C). A drainage tube was placed at the lower segment of the sternum. The skin was closed with skin pins. The operation lasted 1 hour, and the intraoperative blood loss was about 20ml. The patient was sent back to his ward safely after recovering from anesthesia. Two months later, postoperative follow-up showed that the wound healed well (Figure 2D).

iMDT discussion
Discussion among physicians from the Taizhou Hospital of Zhejiang Province: Partial sternal defect accompanied by osteomyelitis is a challenging problem. It often occurs after sternotomy, especially in elderly people and patients with systemic diseases (i.e., diabetes). The sternum is surrounded by fewer soft tissues and more fibrous tissues. Once an infection occurs, the necrotic tissue cannot be easily removed, and the drainage can be difficult, resulting in delayed wound healing and causing great pain to the patients. Standard treatments include wound debridement, drainage, and transfer of vascularized tissue flaps to the wound to facilitate wound healing (5). In our current case, the skin flap transplantation failed. After consulting orthopedic surgeons, we decided to reconstruct the sternum with bone cement. As a fast and safe treatment, bone cement can fill the defective sternum, eliminate the infection foci, and promote wound healing. When the sternum is structurally damaged and combined with osteomyelitis, the traditional treatment is difficult to achieve a radical cure. Despite repeated surgical procedures, the sternum and its wound could not heal; furthermore, co-existing diseases such as diabetes and renal insufficiency also contributed to impaired wound healing.
In this case, there are several questions that should be further considered:
Question 1: Shall the patient continue the conservative treatment or switch to surgical treatment?
Expert opinion 1: Dr. Ahmet Kilic
Surgical wound infection following a sternotomy incision can be a complex and difficult complication for both patients and providers. In its simplest form, it can be a superficial skin or subcutaneous infection that often can be treated with local wound debridement and antibiotics. Unfortunately, when the deeper tissue is effected with either osteomyelitis, a non-healing sternotomy wound or mediastinitis it requires more radical debridement including removal of infected bone with some type of coverage of the space left behind - often times with musculocutaneous flaps.
This patient was treated in the same exact algorithm as I treat my patients. The initial steps for sternal wound infection following coronary artery bypass grafting—antibiotics, sternal debridement, and muscle flap to close the defect left behind from his infection were all appropriate.
This is successful in many patients who have this complication. However, despite all of these efforts, this particular patient was left with a large chest wall defect.
Expert opinion 2: Dr. Francesco Nappi
The case we are discussing is a complex lesion involving the anterior mediastinum and the chest wall. In such cases, conservative treatment is never recommended. No antibiotic treatment has the possibility to limit the damage related to the infectious/inflammatory process responsible for extensive tissue destruction.
Expert opinion 3: Dr. Taufiek Konrad Rajab
Sternal wound infection is a very serious complication of sternotomy. Management of this condition can be very difficult, and I would like to commend the authors in the highest terms for their innovative solution to this problem. Clearly, the described patient had failed conservative management and switching to surgical treatment was appropriate. The patient’s previous treatment most almost certainly failed because the infection had not been fully eradicated before the rigid plate hardware was implanted. As a result, the infection had persisted.
Expert opinion 4: Dr. Daniel Hernandez-Vaquero
Diabetes mellitus and renal dysfunction are risk factors for sternal dehiscence and mediastinitis. So, the patient was predisposed to this complication. Being a young patient, it would be interesting to know if the patient was treated with bilateral AMI since it is likely the main cause of mediastinitis.
At first, the patient presented a deep sternal wound infection, which was aggressively treated with wall debridement, skin flap transplantation, and repair of chest wall defect. This is the usual treatment for this complication, and it can usually solve the problem. This is a rare case where the problem was not solved. It is very important to know the microorganism involved and treat it based on the antibiogram as soon as possible.
Question 2: If surgical treatment will be performed, what is the appropriate timing for the surgery? Which procedure shall be applied?
Expert opinion 1: Dr. Ahmet Kilic
Surgical therapy should be performed any time there’s a concern for systemic uncontrolled sepsis, bacteremia or continues systemic inflammatory response syndrome that is not responding to antibiotic therapy. When there’s any evidence of an infected fluid collection, early separation and dehiscence of a sternal wound continued drainage from the incision site or evidence of necrotic/infected bone—surgery is indicated. The operative steps are to first get source control by trying antibiotics and surgical debridement of all necrotic or infected tissue. This often times requires multiple trips to the operating room to fully eradicate the infection and ensure healthy, bleeding tissue to allow healing. Following debridement, if there’s no large defect, re-wiring of the sternum can be attempted with a vacuum-assisted closure (VAC) dressing for the subcutaneous tissue. Certain times, sternal plating may also be appropriate. If however, there's a large defect, a muscle flap is the best next therapy to treat these patients.
Expert opinion 2: Dr. Francesco Nappi
Concern about the presence of extensive lesions to the heart, sternal bone tissue, cutaneous muscle structures requires immediate intervention. The structures involved must be treated by creating separate areas that no longer have any contact between them so as to circumscribe the infectious/inflammatory process.
Expert opinion 3: Dr. Taufiek Konrad Rajab
It is very important that the timing for surgery is not before the infection is completely eradicated.
Question 3: Is the rigid plate reliable for the fixation of the infected sternal incision?
Expert opinion 1: Dr. Ahmet Kilic
This case represents a very complex situation where all the previously mentioned techniques have been utilized to deal with the infection but have all been unsuccessful. The decision at this time would be to consider a second muscle flap utilizing a different blood supply to the flap. This would come with an increased risk of failure given the events of the prior flap attempt and the patient's co-morbidities that include diabetes, most likely use of the left internal mammary artery, hypertension and need for hemodialysis.
Given the risk vs. benefit profile of a second muscle flap procedure, a foreign body coverage for the sternal defect can be tried. The central question before employing such unconventional methodology is the choice of material and the risk of infection of this foreign material. If all of the bacteria has been eradicated and the only problem becomes filling the dead space, then the bone cement that was tried in this case can certainly be utilized as a last resort attempt.
This is somewhat analogous to lung cancer surgery when ribs are removed, and the chest wall has to be reconstructed, and foreign material such as methyl methacrylate can be utilized (6).
Expert opinion 2: Dr. Francesco Nappi
A Robicsek procedure on either side of the sternum is recommended for fractures when the sternocostal joints are intact. In the event of a disconnection sternocostal, the fixation plates are needed.
Expert opinion 3: Dr. Taufiek Konrad Rajab
If fixation of the sternum with a rigid plate is undertaken in an infected field, the fixation will be unreliable, and the infection will persist on the foreign body hardware despite antibiotic treatment.
Expert opinion 4: Dr. Daniel Hernandez-Vaquero
It is not appropriate to use rigid plate fixation while the sternum is infected because the foreign material can perpetuate the infection.
Question 4: What are the advantages of bone cement in sternal fixation?
Expert opinion 1: Dr. Ahmet Kilic
The advantages of utilizing bone cement are that it is readily available and can conform to the size and shape that is needed to fill this space. It can afford immediate coverage of the mediastinum and its contents and can protect against the complication of having sharp sternal edges that could lacerate the right ventricle with movement.
Expert opinion 2: Dr. Francesco Nappi
In this case, there is no advantage in using bone cement. This is recommended in the absence of infection and where there is good blood perfusion of the bone.
Expert opinion 3: Dr. Taufiek Konrad Rajab
The described case report indicates that bone cement is more resistant to infection than rigid plate sternal fixation. This would be a major advantage of bone cement.
Expert opinion 4: Dr. Daniel Hernandez-Vaquero
Finally, the authors solved the problem with other bone debridement and injecting bone cement into the sternal defect.
The use of bone cement together with wires has been published as an alternative to conventional sternal closure. Its possible advantage would be an earlier osteosynthesis, which would lead to a faster recovery and a lower percentage of dehiscence. At the best of my knowledge, this is the first time bone cement is used to treat this complication and can be a novel and proper option as long as the infection is eradicated.
Question 5: Which treatment strategy will you adopt for such patients?
Expert opinion 1: Dr. Ahmet Kilic
In these complex patients, I believe the authors followed an algorithm that many cardiac and plastic surgeons follow. First to gain control of the infection via antibiotics followed by sternal debridement. This is usually followed by some kind of muscle flap when the sternum cannot be put back together with primary re-wiring or sternal plating. The biggest question following this is whether or not a second flap procedure should have been tried. As I outlined above, the patient had many co-morbidities that could have affected his ability to heal and for this second flap to be successful. That being said, it would have afforded a patient a biological way of dealing with his infection. The big worry about utilizing the bone cement or even the methyl methacrylate for coverage is that it is the use of a foreign body with no blood supply in an already compromised defect where an infection already existed.
I think a couple of things that the authors could add that would make the article stronger would be:
- The HgbA1C of the patient to show how well his blood sugar was controlled.
- A CT scan at the same time as the figure 2d with 3d reconstruction would be helpful to show how the defect was (or was not) successfully treated with the bone cement several months later.
Expert opinion 2: Dr. Francesco Nappi
The structures involved must be treated separately and isolated from one another.
First phase. A complete debridement of the heart of being performed. Accurate washing with saline solution and betadine is recommended. At least 5 drains should be placed in the pericardial cavity ensuring complete vacuum aspiration drainage for at least 3 weeks.
Second phase. Sternal consolidation.
Third phase. Surgical treatment of the coetaneous muscle wall by separating the sternal and coastal parts from the coetaneous muscle. All the necrotic part must be removed. Four vacuums should be placed between the breastbone and the muscle-coetaneous wall, remaining active for at least 3 weeks.
Expert opinion 3: Dr. Taufiek Konrad Rajab
In difficult cases with recurrent sternal wound infections, I would either attempt treatment with an alternative tissue flap or consider using the innovative approach described in this case report by the authors from Wenzhou Medical University.
Expert opinion 4: Dr. Daniel Hernandez-Vaquero
To deal with this fatal complication, we usually use vacuum sealing drainage and adequate intravenous antibiotics until wound cultures are repeatedly negative. Once we achieve this, we proceed to debridement and sternal fixation using wires or, when necessary, rigid plate fixation. Only when the infection has destroyed much of the sternal bone, we perform pectoral muscle flap to achieve a certain degree of stability in the respiratory mechanics. Another option is to chronically treat, usually from 6 to 12 months, with a vacuum sealing drainage favoring healing by second intention. This can be usually done on an outpatient basis.
Conclusions
For sternal reconstruction in patients with recurrent sternal wound infection, bone cement is an appropriate treatment option as it can reconstruct the sternum and achieve good outcomes. Further prospective investigations and long-term follow up are indicated to clarify the applicability and benefits of this technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Matros E, Aranki SF, Bayer LR, et al. Reduction in incidence of Deep sternal wound infections: random or real? J Thorac Cardiovasc Surg 2010;139:680-5. [Crossref] [PubMed]
- Borger MA, Rao V, Weisel RD, et al. Deep sternal wound infection: risk factors and outcomes. Ann Thorac Surg 1998;65:1050-6. [Crossref] [PubMed]
- Gårdlund B, Bitkover CY, Vaage J. Postoperative mediastinitis in cardiac surgery—microbiology and pathogenesis. Eur J Cardiothorac Surg 2002;21:825-30. [Crossref] [PubMed]
- Badawy MA, Shammari FA, Aleinati T, et al. Deep sternal wound infection after coronary artery bypass: How to manage? Asian Cardiovasc Thorac Ann 2014;22:649-54. [Crossref] [PubMed]
- Immer FF, Durrer M, Mühlemann KS, et al. Deep sternal wound infection after cardiac surgery: modality of treatment and outcome. Ann Thorac Surg 2005;80:957-61. [Crossref] [PubMed]
- Suzuki K, Park BJ, Adusumilli PS, et al. Chest Wall Reconstruction Using a Methyl Methacrylate Neo-Rib and Mesh. Ann Thorac Surg 2015;100:744-7. [Crossref] [PubMed]


