Surgical management of multiple rib fractures/flail chest
Introduction
Twenty percent of patients presenting following trauma have thoracic injuries (1). Thoracic injury contributes to 25% of the death seen in trauma patients (2). This includes those with aortic transection, 85% of whom do not make it to the hospital (3). For the remaining the mortality is 10% of which 56% is within the first 24 hours (4). Mortality in the elderly population with multiple rib fractures has been quoted as high as 22% (5). Fifty-five percent of patients, greater than 60 years of age, who die following chest trauma, have isolated rib fractures (6). The risk of mortality, from rib fractures, in relation to age has been shown to increase from the age of 45 (7). It is important, however, to note that 33% of patients with thoracic injuries will have injuries outside the thoracic cavity (8). Thus, appropriate clinical assessment and investigations are key within the emergency department and subsequently on the wards.
Aetiology
Blunt trauma accounts for 90% of thoracic trauma and historically less than 10% of all thoracic trauma underwent surgical intervention (9). Chest radiographs are not sensitive enough at picking up the extent of thoracic trauma (58%) (10). Computerised tomography (CT) scans should therefore play a key role in demonstrating the extent of thoracic injuries, especially if they are highlighted by the aetiology of trauma or the primary survey findings. Rib fractures are associated in 43% of thoracic trauma (11). First and second rib fractures are associated with great vessel injury and this should be investigated by CT scan.
Non-operative management
Rib fractures can range from simple fractures to flail segments. Fail segments refers to multiple adjacent ribs with fractures of the same rib at multiple places. Simple fractures, even if multiple, are often tolerated well in the absence of underlying cardiopulmonary pathology. Analgesia, humidified oxygen, incentive spirometry and physiotherapy are the most important management components. Incentive spirometry and physiotherapy can be limited by pain therefore analgesia needs to be optimised first. Early discussion with the pain team will allow for escalation of analgesia and may include paravertebral blocks or high thoracic epidural analgesia (12). This is associated with improved outcomes and is recommended by the Eastern Association of the Surgery of Trauma Practice (13). Chest drain insertion may be required in patients who have pneumothoraces, a haemothorax or both. A low threshold should be kept for those requiring positive pressure ventilation. Patients with underlying chronic obstructive pulmonary disease and the elderly population, as mentioned before, may require greater observation and escalation of management. Pain control will be more challenging in these patients and thus they are more likely to develop atelectasis and subsequent chest infections, leading to an increased mortality risk (1). This is similar for those with flail segments.
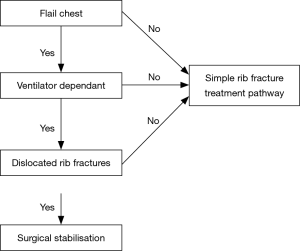
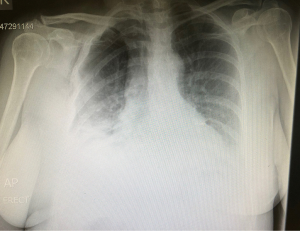
Posterior flail segments are often better tolerated than anterolateral flail segments due to the surrounding structures providing stability, such as the scapula. These, often therefore, do not require surgical intervention. Large anterolateral flail segments compromise respiratory mechanics by causing paradoxical movement of the chest wall. As the diaphragm moves down the intra-thoracic pressure decreases drawing air in. In the presence of flail segments the free segment also moves inward due to the lack of fixation by the spine posteriorly and the sternum anteriorly. Similarly, during expiration the flail segments moves outwards. This is often associated with underlying lung contusion which exacerbates the respiratory compromise. It is important to note that flail segments diagnosed by CT scan may not correlate with clinical paradoxical movement. Hence, clinical examination is imperative in the further management of these patients. In some patients, and when in doubt, a short period of observation is required to allow the chest wall to settle, following injury (Figures 1,2).
Further management
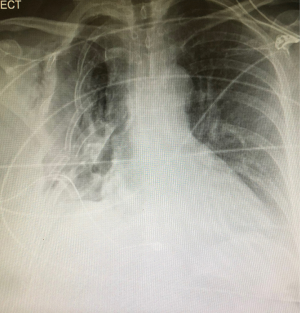
Management options, with regards to chest wall stabilisation, include pneumatic stabilisation in the form of positive pressure ventilation and external traction or osteosynthesis (surgical internal fixation). The principle of pneumatic stabilisation is to temporarily correct for the mechanical disruption while the underlying contusion and pain settles. There is an increasing move towards early surgical stabilisation. The advantages of this option are that it allows for exploration of the thoracic cavity, to drain possible pleural collections, and further identify associated injuries. Furthermore, it can aid in pain relief, improve respiratory mechanics, allow for decreased ventilatory support and allow for earlier mobilization. In turn, this decreases the longer-term complications associated with rib fractures; pneumonia and its associated mortality, chest wall deformity, chronic pain and restrictive respiratory failure. Thus, indications for surgical fixation includes; worsening respiratory failure, major deformity, poor pain control and if undergoing thoracic surgery for other indications, such as, drainage of haemothorax. There is little benefit in surgically fixating those who are beyond 8 to 10 days post-trauma. These patients often have atelectasis and potential developing pneumonia which will complicate surgical fixation and post-operative recovery. Patients with worsening respiratory failure or uncontrolled pain should be targeted earlier for surgical fixation. Randomisation, at day five post-trauma for ventilated patients, to surgical stabilisation versus ongoing pneumatic stabilisation revealed a decreased risk of pneumonia (24% vs. 77%, P<0.05), decreased length of ventilatory support (10.3 vs. 18.3 days, P<0.05) and decreased ITU stay (16.5 vs. 26.8 days, P<0.05) in clear favour of surgical stabilisation (P<0.05) (14). The positive effects of surgical stabilisation persisted beyond the hospital stay. At 1 month and beyond the percent forced vital capacity was higher in the surgical stabilisation group (P<0.05). Furthermore, 61.1% in the surgical stabilisation group versus 0.05% in the ongoing pneumatic stabilisation group had returned to work at 6 months. These findings, in favour of early surgical fixation of flail segments, are further substantiated by meta-analyses which demonstrated a decreased chest pain [odds ratio (OR) 0.4], decreased dyspnoea (OR 0.4), decreased risk of pneumonia (OR 0.18), decreased duration of ventilatory support (gain of 7.5 days), intensive care length of stay (decreased by 4.8 days) and overall hospital stay (decreased by 4 days), decreased mortality (OR 0.31) (15,16). In keeping with the current evidence an appropriate pathway has been created (Figure 1).
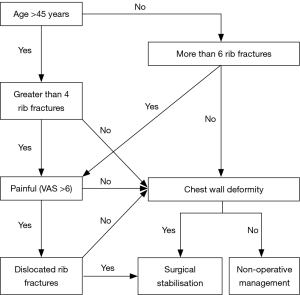
The role of surgical fixation in multiple simple rib fractures
The majority of patients who require fixation are those with flail segments. They are more likely to have respiratory compromise and suffer from pain. As discussed, the evidence is in favour for early surgical stabilisation for these patients. The evidence for surgical stabilisation in the setting of multiple simple rib fractures is less defined. A meta-analysis demonstrated that patients with painful, multiple rib fractures, that were not flail, benefit from surgical stabilisation with regards to pain, respiratory function and socio-professional disability (17). A more recent study corroborated these findings and further demonstrated shorter hospital stay (11.1% vs. 15.9%, P=0.013), fewer respiratory infections (4.6% vs. 17.0%, P=0.025), and an earlier return to work (28 vs. 42 days, P=0.028) (18). A further multicentre, randomised control trial of surgical stabilisation of rib fractures in patients with non-flail fracture patterns is ongoing (19). Given the current evidence an appropriate pathway has been created (Figure 2).
The optimal time for surgical stabilisation
Alongside the growth in surgical rib stabilisation, there is a trend towards early fixation of multiple rib fractures. Surgery within the first 48 hours resulted in a shorter stay in the intensive care unit (P=0.01), shorter invasive ventilatory period (P=0.03), decreased risk of pneumonia (P=0.001) and shorter overall hospital stay (11.5 vs. 17.3, P=0.008) (20).
Contra-indications and relative contra-indications to surgical stabilisation
In the setting of trauma, open rib fractures may be encountered. If there is a contaminated wound the insertion of metalwork will likely lead to chronic infection add morbidity and mortality. It is therefore contra-indicated to surgically fix ribs in this setting.
Severe contra-lateral or bilateral lung contusion will provide difficulty in single lung ventilation. Despite the ability to be able to fix ribs with double lung ventilation this can pose further threat to the respiratory stability of an already fragile patient. Further relative contra-indications include patients with poly trauma. In this setting a multi-disciplinary approach is advised to prioritise treatment.
Whilst not a contra-indication, patients who can be weaned from positive pressure ventilation should be without delay. As discussed, the aim for surgical stabilisation is primarily to decrease ventilatory time, morbidity and mortality. If the patient can return to non-invasive spontaneous ventilation this should be achieved. If at this point pain is an ongoing issue, then the risks versus benefits should be discussed with the patient at this point.
Technical considerations of surgical stabilisation
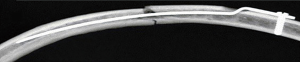
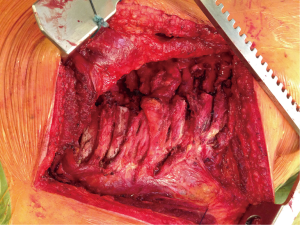
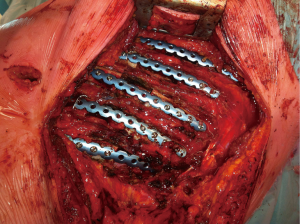
Pre-operative planning with the use of CT with 3D reconstructions are extremely helpful in identifying target fractures and planning incisions (Figure 3). Pre-operative analgesia in the form of a high thoracic epidural is highly recommended. The patient should be intubated using a double lumen tube allowing for single lung ventilation. This allows for the inspection of the pleural cavity including the diaphragm, drainage of a haemothorax and protection of the underlying lung when inserting stabilisation devices. If single lung ventilation is not well tolerated, intermittent apnoea is an appropriate alternative. A lateral decubitus position is appropriate for posterolateral fractures while a supine position maybe adequate for anterior fractures. Video-assisted thoracoscopy (VATS) will provide sufficient visualisation of the thoracic cavity. A well-planned thoracotomy incision, depending on the target fractures to be fixed, with a muscle splitting approach will allow for access without increasing the trauma burden. There is mounting evidence in the literature that often well-placed small incisions can allow good stabilisation without significant surgical trauma to respiratory muscles. Following rib stabilisation, a chest drain should be inserted, especially in those patients whom prolonged ventilation may be required. The aim, however, is to allow for early extubation. Peri-operative bronchoscopy maybe beneficial in providing tracheobronchial toileting and the optimisation of ventilation.

The most commonly repaired ribs are between 4 and 10. These are the most mobile and cause the most pain. Ribs 1 to 3 often require further dissection and may increase the traumatic burden and do not need to be stabilised.
Methods of osteosynthesis
There are several methods of rib stabilisation described in the literature as we have now a wealth of medical devices available for such purpose. These include: plating and bicortical screws, absorbable plating, Judet struts, Kirschner wires and intramedullary pins.
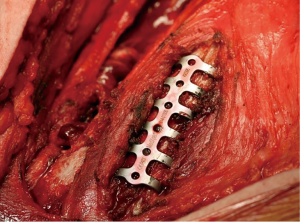
Plating and screws such as the MatrixRIB™ (DePuy Synthes™) system are very accurate and provide excellent stabilisation (Figures 4-7). The plates can be manipulated by length and curved to allow for precise contouring. They are however expensive and increase the operative time due to the need for additional contouring. They also maybe challenging to secure when faced with osteoporotic bone or deep fractures under musculature, under the scapula and those in close proximity to the spine.
Kirschner wires, while easy to place and cheap, do not offer guaranteed stabilisation. Sixty percent of those who are stabilised with wires did not maintain rib fracture stabilisation and thus do not reap the full benefits of rib fixation (21).
Intramedullary pins are technically easy to insert (Figure 8). They should be used mainly for simple, single fractures on a rib as cortical integrity is required for a successful stabilisation. One of the main risks of their use is breaching the rib cortex at the distal end of the pin. Fracture healing is also slower with this method. Marasco et al. in a study revealed that at 3 months patients exhibited complete healing and partial healing at 9% and 85% respectively. All fixed fractures demonstrated complete healing by 6 months (22). This in turn led to a delayed return to work rate of 71% at 90 days.
Intramedullary pins can also provide stability to very posterior fractures where other methods may fail access. Current guidelines suggest rib fractures closer than 2.5 cm from the transverse process should not be stabilised (23). There is a further risk of material migration.
Absorbable plate and screws seem advantageous in the lack of long-term metal work however there failure rate is higher with loss of rib alignment (17.2%) (24). They do provide a magnetic resonance imaging, safe alternative.
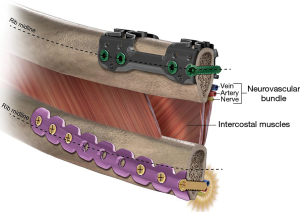
Judet struts provide stability though an anterior plate and are fixed to the ribs using crimps. StraTosTM and StraCosTM (MedXpert GmbH, Germany) clips allow for contouring and for modification of length with the bar (Figures 9,10). This can increase the risk of intercostal nerve impingement, however the RibLoc® U+ plate (Acute Innovations®) is designed to crimp over the superior aspect of the rib keeping free the inferior side where the intercostal bundle lies (Figure 11). These are fixed with locking screws and can house further cortical screws along its length. There is limited data comparing these methods. An in-vitro cadaveric study demonstrated a superiority to the U-plates when compared to plates and screws, when subjected to mechanics of breathing (25).
Titanium and nickel alloys have entered the market and are gaining popularity due to their unique qualities of shape memory and elasticity (26). These are clips such as NiTi Rib plates (Cosmos Medical International) are easy to site even with minimal access approaches (Figures 12,13). These plates are cooled in sterile ice and then applied over the fractured area. As they heat up to body temperature, they return to their original shape and form.
Conclusions
Rib fractures incur a great deal of morbidity and mortality. In addition, this poses a great burden on healthcare resources. Accurate early diagnosis by clinical examination and radiological methods can allow for an optimal management plan. Early discussion with thoracic surgeons should be carried out to allow for intervention within the first 72 hours, if deemed appropriate. There is good evidence that early rib fixation can facilitate pain management, reduce overall hospital stay and complications and allow earlier return to daily activities.
The general consensus is that fixation should take place early, unless there are associated injuries or severe lung contusion. Generally multiple displaced rib fractures require fixation, especially when anterior chest wall instability is evident. There is now a wealth of medical devices available for rib fixation and the best is the one that the surgeon has experience with and feels comfortable in utilising.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Yuh DD, Doty JR, Vricella LA, et al. Thoracic Trauma. In: Yuh DD, Vricella LA, editors. John Hopkins Textbook of Cardiothoracic Surgery. 2nd edition. New York, NY: McGraw Hill Education; 2014:9-24.
- Blyth A. Thoracic Trauma. BMJ 2014;348:g1137. [Crossref] [PubMed]
- O’Conor CE. Diagnosing traumatic rupture of the thoracic aorta in the emergency department. Emerg Med J 2004;21:414-9. [PubMed]
- Kulshrestha P, Munshi I, Wait R. Profile of chest trauma in a level I trauma centre. J Trauma 2004;57:576-81. [Crossref] [PubMed]
- Bulger EM, Arneson MA, Mock CN, et al. Rib fractures in the elderly. J Trauma 2000;48:1040-6. [Crossref] [PubMed]
- Kent R, Woods W, Bostrom O. Fatality risk and the presence of rib fractures. Ann Adv Automot Med 2008;52:73-82. [PubMed]
- Holcomb JB, McMullin NR, Kozar RA, et al. Morbidity from rib fractures increases after age 45. J Am Coll Surg 2003;196:549-55. [Crossref] [PubMed]
- Başoğlu A, Akdağ AO, Celik B, et al. Thoracic trauma: an analysis of 521 patients. Ulus Travma Acil Cerrahi Derg 2004;10:42-6. [PubMed]
- Ludwig C, Koryllos A. Management of chest trauma. J Thorac Dis 2017;9:S172-7. [Crossref] [PubMed]
- Hehir MD, Hollands MJ, Deane SA. The accuracy of the first chest X-ray in the trauma patient. Aust N Z J Surg 1990;60:529-32. [Crossref] [PubMed]
- Baghai M, Whitaker D. Thoracic trauma. In: Moorjani N, Viola N, Walker WS, editors. Key Questions in Thoracic Surgery. 1st edition. Shewsbury, UK: TFM publishing Ltd.; 2016:971-88.
- Bulger EM, Edwards T, Klotz P, et al. Epidural analgesia improves outcome after multiple rib fractures. Surgery 2004;136:426-30. [Crossref] [PubMed]
- Simon BJ, Cushman J, Barraco R, et al. Pain management guidelines for blunt thoracic trauma. J Trauma 2005;59:1256-67. [Crossref] [PubMed]
- Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomised study of management of severe flail chest patients. J Trauma 2002;52:727-32; discussion 732. [Crossref] [PubMed]
- Slobogean GP, MacPherson CA, Sun T, et al. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg 2013;216:302-11.e1. [Crossref] [PubMed]
- Leinicke JA, Elmore L, Freeman BD, et al. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg 2013;258:914-21. [Crossref] [PubMed]
- Girsowicz E, Falcoz P, Santelma N, et al. Does surgical stabilization improve outcomes in patients with isolated multiple distracted and painful non-flail rib fractures? Interact Cardiovasc Thorac Surg 2012;14:312-5. [Crossref] [PubMed]
- Qiu M, Shi Z, Xiao J, et al. Potential benefits of rib fracture fixation in patients with flail chest and multiple non-flail rib fractures. Indian J Surg 2016;78:458-63. [Crossref] [PubMed]
- Pieracci FM. A multicenter, randomised controlled trial of surgical stabilization of rib fractures in patients with severe, non-flail fracture patterns. 2018. Available online: https://clinicaltrials.gov/ct2/show/NCT03221595
- Iqbal HJ, Alsousou J, Shah S, et al. Early surgical stabilization of complex chest wall injuries improves short-term patient outcomes. J Bone Joint Surg Am 2018;100:1298-308. [Crossref] [PubMed]
- Abd-Elnaim MK, El-Minshawy A, Osman MA, et al. Plating versus wiring for fixation of traumatic rib and sternal fractures. Journal of the Egyptian Society of Cardio-Thoracic Surgery 2017;25:356-61. [Crossref]
- Marasco S, Quayle M, Summerhayes R, et al. An assessment of outcomes with intramedullary fixation of fractured ribs. J Cardiothorac Surg 2016;11:126. [Crossref] [PubMed]
- Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: Surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury 2017;48:307-21. [Crossref] [PubMed]
- Marasco SF, Sutalo ID, Bui AV. Mode of failure of rib fixation with absorbable plates: a clinical and numerical modeling study. J Trauma 2010;68:1225-33. [Crossref] [PubMed]
- Sales JR, Ellis TJ, Gillard J, et al. Biomechanical testing of a novel, minimally invasive rib fracture plating system. J Trauma 2008;64:1270-4. [Crossref] [PubMed]
- Bemelman M, Long W, Mayberry J. History of rib fracture management. In: de Moya M, Mayberry J, editors. Rib Fracture Management: A practical manual. 1st edition. New York, NY: Springer International Publishing; 2018:1-24.