
Revascularization of right coronary artery chronic total occlusion by bilateral knuckle technique
Introduction
The retrograde and hybrid approach have improved the overall success rate of the recanalization of chronic total occlusion (CTO) lesions.
However, the whole procedure requires excessive time and X-ray scanning, especially for complex lesions. The knuckle wire technique (1) is used to create a deliberate dissection plane in the sub-intima of the CTO lesion, and the wire, usually a polymer-jacketed guide wire, is pushed until a complex loop is formed and advanced through the lesion.
In the case of the CTO lesions we have just completed, we used the bilateral knuckle technique which significantly sped up the process of procedure in a safe way.
Case presentation
The patient was a 59-year-old man who had suffered chest pain for 5 years and was aggravated for 7 days. He had Hypertension and smoking history. The EKG showed ST depression in leads V5 and V6. The echocardiography showed inferior wall hypokinesis, left ventricular end-diastolic dimension (LVEDD) 61mm, and ejection fraction (EF) 41%. Blood test showed that cardiac troponin I (cTnI) was 2.501 ng/mL. Coronary angiography showed total occlusion of the distal segment of the left circumflex coronary artery (LCX) and total occlusion of the proximal segment of the RCA. The occluded LCX was recanalized and stented.
Several days later, we tried to open the CTO lesion of the RCA. We took a bilateral radial artery approach, with an AL1ST guiding catheter (cordis) engaged to the RCA from the right radial artery, and an EBU 3.75 guiding catheter (Medtronic) engaged to the LCA from the left radial artery.
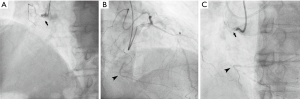
The coronary angiography we performed showed long occlusion of the RCA, blunt proximal stump, and bending within the occluded segment. Some septal collateral branch could be seen from the left anterior descending artery (LAD) to the RCA (Figure 1). The J-CTO score was 2 points (2).
Considering the low success rate of the antegrade approach, we decided to try the retrograde approach from the beginning.
With the support of a Finecross microcatheter (Terumo), a Sion guidewire (Asahi) was advanced to the mid-LAD, crossed a septal collateral, and successfully reached the distal end of the RCA occlusion segment, with the microcatheter advancing to the distal end of the RCA occlusion segment. The Sion guidewire could not go any further, and we attempted to cross a fielder-XT guidewire over the occlusion segment, but it still could not go any further. The fielder-XT wire was deliberately made to a knuckle cure, and pushed strongly into the body of the occluded lesion. We then went back to the antegrade side. With the support of another Finecross catheter, a Gaia 2nd guidewire was used to puncture the proximal cap of the CTO, and then another knuckled fielder-XT was pushed strongly to the distal of CTO until close to the retrograde knuckle wire (Figure 2A).
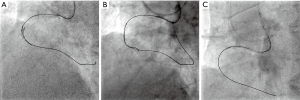
Then, the antegrade fielder-XT wire was changed to an Ultimate Bros 3 wire, and the wire was manipulated as close as possible to the retrograde wire. Next, multiview of fluoroscopy was performed to confirm that the antegrade wire and retrograde wire were all in the architecture of the artery. After reverse cart technique was performed (1) with a 2.0×20 mm balloon expansion, a new fielder-XT wire crossed the occluded lesion and advanced retrogradely to the proximal true lumen of the RCA, and then entered the AL1ST guiding catheter (see Figure 2B).
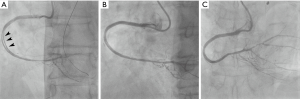
With the help of the Guidezilla (Boston Scientific), a retrograde microcatheter successfully entered the antegrade guiding catheter. In the antegrade AL1ST guiding catheter, a run-through guidewire was manipulated into the retrograde Finecross microcatheter (rendezvous technique, see Figure 2C) and advanced to the distal of RCA. After predilatation with a 2.5×20 mm balloon, 3 stents were implanted in the RCA. However, angiography showed a long thrombus in the stents (Figure 3A), although the blood flow was still TIMI 3 grade. Thrombus aspiration was performed and final angiography showed a good result (Figure 3B,C).
Discussion
The procedure was successfully completed within 2 h with 150 mL contrast, and it took only 76 min to cross the wire. The patient was discharged only 24 h after without any symptoms.
The knuckle wire technique is used to advance a looped polymer-coated wire (“knuckle”) in a subintimal space to cross a CTO lesion. This technique is based on the principle of differential resistance between tissue planes and capitalizes on the relative longitudinal weakness of the sub-intimal plane, which allows rapid tracking to the distal lumen. Dissection is usually achieved with a looped polymer-coated wire, which can be advanced safely and rapidly within the sub-intimal space, usually with the leading end being the junction between the stiff and floppy part of the wire. This safe method capitalizes on the distensibility of the adventitia; that is, blunt force can be easily applied within the vessel wall as it is delivered to the adventitia over a large area—causing blunt dissection, whereas stiff guidewire tips deliver significant force to a focal area with a high risk of perforation. In addition, the knuckled wire is less likely to find and perforate any side branches. The primary limitation with this technique in peripheral artery CTO procedures has been failure to re-enter the distal true lumen after sub-intimal crossing of the occlusion (success rate estimated to be approximately 20% with a guidewire alone) (3).
In this case, we used a bilateral knuckle technique, which achieved rapid and safe passage of the wire crossing, and, combined with the reverse cart technique, we completed the linkage of antegrade and retrograde wire. This technique is very effective for long CTO lesions with ambiguous proximal and distal cap.
Acknowledgements
None.
Footnote
Conflicts of interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
References
- Muramatsu T. Current technical and clinical features of the antegrade and retrograde approaches to percutaneous transluminal coronary intervention for chronic total occlusion – 2013 version. The Egyptian Heart Journal 2014;66:1-10. [Crossref]
- Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv 2011;4:213-21. [Crossref] [PubMed]
- Wilson W, Spratt JC. Advances in procedural techniques--antegrade. Curr Cardiol Rev 2014;10:127-44. [PubMed]


