Non-intubated single port thoracoscopic procedure under local anesthesia with sedation for a 5-year-old girl
Introduction
Medical thoracoscopy is a short and simple procedure for the diagnosis or biopsy of thoracic disease (1). In adult patients, it can be easily performed using local anesthetics with or without sedation under the cooperation of the patient (2). However, this is not feasible in pediatric thoracoscopy, which often requires general anesthesia (3). In pediatric patients less than 30 kg, carbon dioxide gas insufflation into the chest cavity through an air-tight port is needed to collapse the lung for operation (4).
In our case, we demonstrated the use of a non-intubated single port thoracoscopic procedure in a 5-year-old girl under local anesthesia with sedation for the management of a chest tube which was inadvertently sutured in the thoracic cavity.
Case report
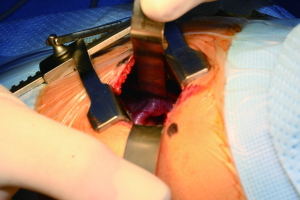
A girl aged 5 years and 2 months (height 109 cm, weight 18.6 kg) experienced recurrent pneumonia over a 2-year period. Chest radiographs and computed tomographic (CT) scan showed extra lobar pulmonary sequestration in the left lower lung. Her vital signs were stable, and no other anomalies were detected during preoperative evaluation. We resected the lesion through an incision in the left lateral thoracotomy (length, 3 cm) along the fifth intercostal space, under general anesthesia with a single lumen tracheal tube (Figure 1). After resection of the sequestrated lung, a 16-Fr chest tube was inserted into the seventh intercostal space. The intercostal space was repaired using a 4-0 absorbable suture. After two days, the chest tube could not be withdrawn. It seemed to have been inadvertently sutured beneath the thoracotomy incision inside the thoracic cavity. At this point, we decided to perform the thoracoscopic procedure through the chest tube insertion site under sedation without tracheal intubation.
Sedation was achieved using Intravenous (IV) dexmedetomidine (1.0 μg/kg) for over 15 min before the injection of local anesthetics, followed by 1 mg/kg of IV ketamine and dexmedetomidine 0.2-1.0 μg/kg/h IV (5). Oxygen at 6 L/min was administered via a pediatric face mask. The patient was monitored during sedation, and the bispectral index (BIS) was maintained between 45 and 65 during the procedure. The thoracoscopic procedure was performed in the right lateral decubitus position (Figure 2A). Local anesthesia was achieved around the hole where the chest tube was inserted, using a 2% lidocaine solution.
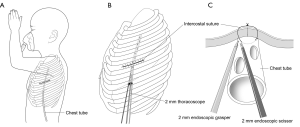
After the chest tube was pulled and shortened, a 2-mm thoracoscope was inserted through the chest tube site (5.5 mm incision) (Figure 2B). The ipsilateral lung was collapsed, during which the patient kept breathing with the contralateral lung. The intercostal suture material penetrating the middle part of the chest tube was found underneath the thoracotomy wound (Figure 2B). The suture was intrathoracically cut using 2-mm endoscopic scissor and grasper (Figure 2C), and the chest tube was removed. The new 16-Fr chest tube was inserted through the same hole, and anchored outside of the hole.
The patient’s vital signs were stable during the entire operation (intraoperative mean arterial pressure, 85-90 mmHg; intraoperative heart rate, 90-92 beats/min; and intraoperative SPO2, 99-100%). Ketamine 0.5 mg/kg (IV) was added as a bolus when involuntary movements or cough reflex occurred. The total operation time was 35 min, and the sedation time was 55 min. The IV dexmedetomidine infusion was discontinued at the end of surgery. After returning to the supine position, she was transferred to the recovery room.
The second chest tube was withdrawn immediately after checking the chest radiography. She was allowed to drink water one hour later, and was discharged after two days. No delayed complications were observed during the follow-up.
Discussion
In thoracoscopic procedures for pediatric patients less than 30 kg, comprehensive visualization of the surgical field is quite difficult, even under general anesthesia (3,4). A collapse of the ipsilateral lung is essential for the surgeon to be able to perform a thoracoscopic procedure in thoracic cavities which have limited space. Because there are no appropriate double lumen tracheal tubes, which are used for selective one lung ventilation in adult patients, generally, single lumen tracheal intubation is generally applied in small pediatric patients, with carbon dioxide gas insufflations through air-tight ports into the thoracic cavity to collapse a lung (3,4).
In the present case, a self-ventilating thoracoscopic procedure under local anesthesia with sedation was planned. We considered that the repeat of general anesthesia in a patient who had undergone general anesthesia for the surgery just three days before may be harmful, especially for performing a short and simple procedure, such as cutting a suture material in the thoracic cavity. In addition, the ventilation of two lungs using a single lumen tracheal tube has no benefit in thoracoscopic surgery.
Active negative ventilation and opened thoracic cavity can collapse the ipsilateral lung, maintaining the ventilation of the contralateral lung under local anesthesia with sedation. Previous studies reported non-intubated thoracosopic bleb resections and lobectomies under sedation combined with various local anesthetic methods (1,6-9).
Sedation with IV ketamine and dexmedetomidine was available, and could provide a stable condition for uncooperative pediatric patients during the procedure. Even a simple procedure cannot be performed under local anesthesia without sedation in younger than school-aged patients because of their uncontrollable movement (4). This creates the necessity of deep sedation, which can often cause respiratory depression (3). We chose to combine IV ketamine with IV dexmedetomidine for our patient. Dexmedetomidine has been shown to produce stable sedation without respiratory depression (10), and provides analgesia and hemodynamic stabilization. In addition, it may prevent tachycardia, hypertension, and emergence phenomena associated with ketamine, while ketamine prevents bradycardia and hypotension, which have been reported with dexmedetomidine (11).
The procedure through the single hole from the previous chest tube, that is, the single port procedure was adjustable for an unconscious sedated patient. If possible, less irritation of the wound during the operation is better to maintain sedation. Compared with multiple port surgery, the stimulation of the port site can be reduced in single port surgery.
To the authors’ knowledge, this report is the first report of a non-intubated single port thoracoscopic procedure under local anesthesia with sedation in a patient younger than school age. In the present case, non-intubated surgery improved the surgical view in pediatric thoracoscopic surgery, and single port surgery was effective under local anesthesia with sedation. However, our case was of a very short and simple procedure. Prospective randomized trials are required to determine the efficacy of non-intubated single port thoracoscopic surgery under local anesthesia and sedation in cases of complicated and long thoracoscopic procedures for pediatric patients.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Migliore M, Giuliano R, Aziz T, et al. Four-step local anesthesia and sedation for thoracoscopic diagnosis and management of pleural diseases. Chest 2002;121:2032-5. [PubMed]
- Solak O, Cuhadaroglu S, Sayar A, et al. Thoracic surgical operations performed under local anesthesia and sedation for diagnosis and treatment. Thorac Cardiovasc Surg 2007;55:245-8. [PubMed]
- McGahren ED, Kern JA, Rodgers BM. Anesthetic techniques for pediatric thoracoscopy. Ann Thorac Surg 1995;60:927-30. [PubMed]
- Kumar K, Basker S, Jeslin L, et al. Anaesthesia for pediatric video assisted thoracoscopic surgery. J Anaesthesiol Clin Pharmacol 2011;27:12-6. [PubMed]
- Tseng YD, Cheng YJ, Hung MH, et al. Nonintubated needlescopic video-assisted thoracic surgery for management of peripheral lung nodules. Ann Thorac Surg 2012;93:1049-54. [PubMed]
- Nezu K, Kushibe K, Tojo T, et al. Thoracoscopic wedge resection of blebs under local anesthesia with sedation for treatment of a spontaneous pneumothorax. Chest 1997;111:230-5. [PubMed]
- Pompeo E, Mineo TC. Awake operative videothoracoscopic pulmonary resections. Thorac Surg Clin 2008;18:311-20. [PubMed]
- Rocco G, Romano V, Accardo R, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for peripheral pulmonary nodules in a complete ambulatory setting. Ann Thorac Surg 2010;89:1625-7. [PubMed]
- Katlic MR, Facktor MA. Video-assisted thoracic surgery utilizing local anesthesia and sedation: 384 consecutive cases. Ann Thorac Surg 2010;90:240-5. [PubMed]
- Levänen J, Mäkelä ML, Scheinin H. Dexmedetomidine premedication attenuates ketamine-induced cardiostimulatory effects and postanesthetic delirium. Anesthesiology 1995;82:1117-25. [PubMed]
- Luscri N, Tobias JD. Monitored anesthesia care with a combination of ketamine and dexmedetomidine during magnetic resonance imaging in three children with trisomy 21 and obstructive sleep apnea. Paediatr Anaesth 2006;16:782-6. [PubMed]


