
The ideal methods for the management of rib fractures
Introduction
Rib fracture cases are one of the most common thoracic traumas, which accounts for about 2/3 of them (1). According to a statistical report, 300,000 patients in the US were diagnosed with rib fractures in 2004 (2); and this figure is increased to more than 350,000 in 2017 (3). However, most of the rib fracture patients did not have an effective medical treatment. For example, in the US, only 100,000 rib fracture patients were admitted to hospital for treatment in 2004. There is no official annual statistics about the rib fracture cases in China. However, based on the population, motor vehicle ownership, the crowded cities, and the busy traffic conditions, it is expected that there are over 1 million cases of rib fractures in China. This number is more than the annual sum of lung cancers and esophageal cancers, which are also the most common cases in Thoracic surgery department (4).
Although there are a significant amount of cases annually, the rib fractures treatment options are still lacking, and the rate of surgical treatment conversion is still very low. This situation is caused majorly by the lack of attention on chest trauma and the controversies and debates on the treatment options for rib fractures. Per the statistics data analysis of the Canada’s National Trauma Data Bank from 2007 to 2009, only 0.7% of the flail chest injury patients were treated by the surgical fixation of the chest wall (5). Dr. Yang surveyed in China and found that there were 17,600 rib fractures cases documented in 371 Chinese hospitals, but the surgical conversion rate on these cases was only 2% to 3%. Several main reasons could be attributed to the low conversion rate of surgery. Firstly, there is a lack of high-level convincing clinical research to confirm the evidence that surgery is a better treatment option for rib fractures.
Secondly, the disciplinary boundary for treating rib fractures is unclear. Currently, orthopedics, traumatologists, and thoracic surgeons, and others are all involved in the treatment of rib fractures. Geographically, patients with rib fractures in Europe and United States are mainly treated by traumatologists; while in China, over 95% of patients with surgical stabilization of rib fractures (SSRF) treatments would be mainly treated by thoracic surgeons. Compared to the treatment of other fractures such as the spine, limbs, etc., the treatment of rib fractures requires different pathophysiological and biomechanical requirements. Therefore, it is strongly recommended that the rib fractures treatment should be led by doctors who have a full understanding of these different needs. Thirdly, it is relatively difficult to carry out clinical research on rib fractures. Rib fracture cases are normally part of the complication of trauma. Due to the timeliness of trauma treatments, patients would be diverted to different departments. On the other hand, the conditions from rib fractures are very diverse. Both situations contribute to one of the biggest challenges of clinical research on having enough cases to form a research group(s). Fourthly, research progress on the internal fixation materials for rib fractures is relatively lacking compared to others. Currently, most of the internal fixation materials for the rib fractures are based on the requirements and concepts of orthopedic internal fixation materials. However, the shapes and biomechanical properties gap between ribs and orthopedics becomes one of the main obstacles for the rib fracture treatments.
Lastly, the concepts and understanding of rib fracture treatments are outdated. The knowledge regarding the science of rib fractures has not been updated in the recent decades. Due to the lack of convincing support from evidence-based medicine, medical personnel from thoracic surgery, emergency, trauma, orthopedics, and intensive care unit (ICU) departments, who are highly related to rib fractures patients, have a lack of knowledge about the progress on rib fracture treatments. Therefore, they are not familiar with the current clinical research on rib fracture treatments. Moreover, they also do not understand the corresponding instruments and surgical methods for the treatment of rib fractures (6).
This article analyzes and summarizes the existing evidence, published literature, and research, combined with the authors’ long-term experience in the treatment of rib fractures.
The core management of rib fractures can be described in four areas, damage control, pain management, fixation selection, and quality of life.
Damage control
Pulmonary contusion
Several studies have suggested that flail chest and multiple rib fractures with severe pulmonary contusion are not suitable for surgical treatment. In 1998, a German study divided the flail chest patients into four groups based on whether they had undergone surgical treatment and whether it was combined with a pulmonary contusion. The researchers, Voggenreiter et al. studied and concluded that for the flail chest with a pulmonary contusion research group, surgical chest wall stabilization increased the mortality and complications (7). In 2016, Farquhar et al. (8) conducted a retrospective cohort study comparing patients that were treated by rib fractures fixation surgery and patients that were treated nonsurgically by modern multidisciplinary protocols. The study results showed that the modern multidisciplinary protocols approach provided a better result and patients did not receive any benefits from the fixation surgery. Although the conclusion from this study still has worth for exploration and has limitations due to the fact that the proportion of pulmonary contusion in these two study groups was inconsistent (100% in the surgical group and only 58% in the nonsurgical group), and the injury in the surgical group was more severe; it does suggest that flail chest injuries with pulmonary contusion may not be suitable for fixation surgery, and the nonsurgical modern multidisciplinary protocols would be preferred. Clinically, there is a high proportion of patients have blunt chest trauma with pulmonary contusion, which is between 30% and 75% (9); also, it has been observed that patients in blunt chest trauma with pulmonary contusion did not have higher complications and mortality after the internal fixation. Therefore, whether the surgery option is suitable for a pulmonary contusion injury could be determined by the severe level of pulmonary contusion. However, currently, there is still no recognized standard for judging the severity of a pulmonary contusion. Some researchers have identified that a patient with a pulmonary contusion with a CTVI (CT volume index) score of over 20% will be relatively easier to develop the acute respiratory distress syndrome (ARDS) complication and has a higher mortality (10-12). On the other hand, it is still worthwhile for further studies to confirm whether the 20% CTVI pulmonary contusion score should be one of the criteria for a surgical treatment.
In many studies, severe pulmonary contusion is considered to be a contraindication to surgery. However, we believe this view is also worth exploration and reconsidering. We believe that surgery is still one of the options for a severe pulmonary contusion. Ventilation dysfunction, which is majorly caused by severe pulmonary contusions, cannot be improved by surgery. It is mostly treated by a comprehensive treatment of internal medicines (13), including respiratory monitoring (with or without mechanical ventilation), fluid resuscitation, respiratory management, and chest physiotherapy, etc. Severe pulmonary contusions require mechanical ventilation to improve the ventilation dysfunction condition; and multiple ventilation alternatives, including the positive end-expiratory pressure (PEEP), high-frequency oscillatory ventilation (HFOV), and independent lung ventilation (ILV) have been proven to be effective (14-18). Several types of research reported that pulmonary contusion would recover faster than ARDS. The condition of pulmonary contusion would start to improve after 24 to 48 hours. It would completely improve within 14 days after the injury (19-23). While the remote, paraneoplastic effects of pulmonary contusion often occur 8 hours after the injury. Therefore, some studies suggest that the surgery option can be considered if the surgery indications still exist after the condition of the pulmonary contusion improved. In order to avoid the exacerbation of the acute phase of severe pulmonary contusion, the remote effects, and the effect of anesthesia on lung function (24,25), one suitable surgical choice is to wait 48 to 72 hours after the peak of pulmonary contusion, which is the surgical opportunity mostly recognized by medical practitioners. In 2016, Pieracci et al. concluded that the SSRF, including some patients with pulmonary contusion, would have a better outcome compared to the nonsurgical group after the surgery when it is performed within 72 hours after the injury (26). Although there was no description of the severity of the pulmonary contusion, the number of the pulmonary contusions was limited in this research, the conclusion on supporting surgical treatment on pulmonary contusion would be worth a further study. Therefore, it will be relatively easier to understand that the surgical option is the principal application of damage control. We recommend that it would be appropriate to perform the surgical treatment for the rib fractures injury combined with a severe pulmonary contusion after 48 to 72 hours of the injury. However, further study will be needed to provide a clearer definition and an indication of a severe pulmonary contusion.
Brain injury
In the current clinical research on the surgical treatment of rib fractures, patients with severe craniocerebral trauma and spinal injury were excluded from the study. There is currently no direct evidence to support that these two groups of patients would not benefit from undergoing a rib reduction and internal fixation surgery. Based on the past efficacy efficiency study of rib fractures between the operative and nonoperative treatment, the most selected observation indicators are hospitalization time, ICU time, ventilator application time, and tracheotomy ratio. For rib fracture patients combined with severe craniocerebral trauma, they are either in the state of coma or under the application of sedative drugs for mechanical ventilation. Under these situations, even the patients which have undergone the internal fixation surgery, the hospitalization time, ICU time, and ventilator application time will not be reduced; furthermore, the advantages of the internal fixation surgery cannot be exemplified. On the other hand, based on our clinical observations, when these patients’ brain function has recovered, and they are trying to leave out the ventilator, the timely internal fixation surgery will help to reduce the application of sedative and analgesic drugs, shorten the application time of ventilator, and improve the success rate of the relief from the ventilator. Therefore, internal fixation surgery is not a contraindication for rib fractures patients combined with severe craniocerebral trauma; rather the intervention time for surgery will be a crucial decision.
Spinal injury
Similarly, patients with spinal fractures will need to stay in bed for recovery. Internal fixation surgery would not shorten the time of early out-of-bed activities. However, the surgery can stable the chest wall, relieve the pain, effectively promote cough and expectoration, and reduce respiratory complications caused by prolonged bed rest. With these benefits, the contemporaneous or staging internal fixation of rib fractures, during the surgical fixation of the spinal injury, could help reducing pain and complications, and benefit patients.
Therefore, for patients with composite trauma, it is necessary to evaluate and judge the impacts of multiple injuries. Under the damage control principle, selecting the right time for internal fixation of rib fractures can still provide benefits to the patients.
Pain management
Currently, three major randomized controlled trial (RCT) (27-29) studies have been completed that have compared the surgical treatment of rib fractures to nonsurgical treatments. Although the results of these studies all concluded that the surgical treatment group is better than nonsurgical treatment group, the enrolled patients for these three papers all had a flail chest injury, their sample size was relatively small, and the observation indicators and conclusions were not completely consistent. The conclusion that surgical treatment is better than nonsurgical treatment has not been fully accepted. Moreover, it is interesting to observe that the later the study started, the less advantageous it was to undergo the surgical treatment. The main reason could be attributed to the internal medicine improvement of the conservative treatment group. In 2012, the US Eastern Association for the Surgery of Trauma (EAST) released the Management of Pulmonary Contusion and Flail Chest: an Eastern Association for the Surgery of Trauma Practice Management Guideline, proposed and advocated that rib fractures need a multidisciplinary management model (13). In 2017, the US Western Trauma Associated published its algorithms Western Trauma Association Critical Decisions in Trauma: Management of rib fractures (30) and suggested that the most significant impact of flail chest injury on respiratory functions is the pulmonary contusion and pain. In contrary, the abnormal breathing, which is commonly accepted as the greatest impact on the respiratory function, actually has less of an impact when compared to a pulmonary contusion and the associated pain. Some scholars have even questioned the existence of the mediastinal oscillating gas from abnormal breathing.
The dangers of a flail chest on the body are the compounded harm, i.e., the possibility of a combination of the severe pulmonary contusion, pain, and abnormal breathing, etc. Current research suggests that almost all cases of death caused by flail chest are accompanied by a pulmonary contusion. When combined with a severe pulmonary contusion, the treatment plan of a flail chest should be focused on the care of the pulmonary contusion, rather than the fixation of the chest wall. Therefore, the surgical treatment would be a suitable option for the flail chest when it is not combined with a severe pulmonary contusion.
Pain is another major factor affecting respiratory functions, which should also be worthy of our full attention. In Europe and the United States, the abuse of painkillers has become a social problem. In the opposite, the traditional Chinese concept on handling pain by enduring it has caused patients to experience higher pain. This endurance philosophy indicates that the concern on pain control is insufficient.
Pain is not only a symptom. Its effects on respiratory function and the occurrence of cardiovascular and cerebrovascular complications are the main causes of rib fractures complications. Moreover, the pain would also cause other various harms and damages, although the long-term effects of pain are still unclear.
On average, each person breaths about 20,000 times a day. As the continuous breathing exercise, the rib fracture pain would be more severe. The rib fracture pain persists with respiratory movements, and it is an III–IV pain level on the pain grade scale. In principle, the pain treatment choice for a rib fracture patient is normally following a three-step analgesic program. It starts from oral nonsteroidal anti-inflammatory drugs (NSAIDs) to an intercostals nerve block, patient-controlled analgesia (PCA) pump, and finally to a continuous epidural anesthesia. In 2012, epidural analgesia or paravertebral analgesia was recommended as the best analgesia delivery option for rib fracture injuries by the practice management guideline issued by EAST (13). However, the excessive dosage and time usage of morphine will bring some side effects.
Moreover, chronic pain patients would also face a challenge for abusing analgesic drugs. On the other hand, clinical observations have found that the internal fixation of rib fractures is a very effective option for relieving pain. Nowadays, we can see that there is an increasing number of clinical studies which have used pain relief as one of the main indicators for the internal fixation on rib fractures.
In 2012, a meta-analysis conducted by Girsowicz et al. (31) found that surgery can significantly alleviate the post-operative pain and the occurrence of dysfunctions for the non-flail chest fractures, as well as providing other merits. Chronic pain under the conservative treatments leads to the long-term use of painkillers, prolonged return to work, and a lower quality of life, which all need our attention. Michelitsch et al. (32) reviewed data of 1,398 patients with rib fractures in a single medical center over a consecutive 5-year period. Among these patients, 235 patients had severe thoracic trauma (AIS >3). Twenty-three patients had internal fixation surgery and fixed a total of 88 rib fractures, where 18 patients underwent an average of 27 months of postoperative follow-up. There were no reported chronic pain and limited mobility. Slater et al. (33) reported a case—a flail chest patient with long-term chronic pain was treated with internal surgical fixation six years after the injury. The postoperative follow-up showed that the patient was able to return to work without any pain complaints.
However, pain is a subjective feeling. The level of pain assessment is very complicated. In 2017, EAST issued a practice management guideline on operation fixation of rib fractures. After analyzed twenty-two related studies, the guideline concluded that the internal fixation treatment for flail chest patients under certain conditions could reduce mortality. Moreover, it also could shorten the duration time of mechanical ventilation and ICU, and reduce the incidence of pneumonia and the need for a tracheostomy (34). A majority of flail chest patients are treated with high doses of analgesics, even tracheal intubation, and sedatives, and it would be extremely difficult to perform the post-operative pain assessment properly. In 2018, scholars from the Netherlands conducted a multicenter cohort study with the largest enrollments number to date. The main surgery indications for multiple rib fracture injury in this study were the pain. The study compared the treatment outcomes between the internal fixation and conservative approach on flail chest and multiple rib fractures injury. The study concluded that the surgical approach has no obvious advantages in the length of stay in hospital and ICU, and in improving pain relief (35). Despite these findings, we believe that as it was a retrospective study, it was not possible to compare the pain score and the effects of pain interventions. Under this circumstance, we believe these studies have missed the most potential benefits of the internal fixation. More other studies have been concluded that surgical treatment has an obvious advantage in pain relief compared to conservative treatment (36,37). These conclusions are consistent with the clinically observed treatment efficacy. We believe that for simple only multiple rib fractures case, the evaluation of surgery options should not be based on the length of stay in hospital and ICU. Because there are many other interference factors, such as compound injuries, doctor’s judgment, patient’s choices, etc. In actuality, the effectiveness of the pain control should be used as a critical criterion for evaluation of the surgery option. It is not only because pain is a direct symptom to rib fractures, but also it is closely related to the patient’s quality of life. Therefore, pain relief is a better and more suitable indicator to evaluate the surgical value of the internal fixation.
Currently, there is no generally accepted indication for the surgical treatment of rib fractures. Some countries or organizations have published guidelines for reference, and the content is very similar. One of the most controversial topics is what the purpose of the surgical treatment is for multiple rib fractures without a flail chest? We believe that the surgical indications for rib fractures are not only understood from the anatomical perspective of restoring the integrity of the thorax but also should be understood from the improvement of pathophysiological changes after an injury, after which will be helpful to better grasp the surgical indication of internal fixation in clinical practice. According to the surgery clinical indications consensus for rib fractures by the European and American experts in 2013 (38) (Table 1), the surgery option should be considered under the following three types of situations: the situation that surgery is the only option, pain control, and improving the long-term quality of life.
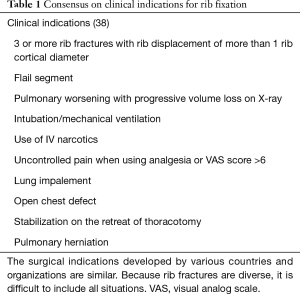
Full table
The indications for the first situation refer to severe rib fractures combined with some other special injuries, and a must for thoracotomy, such as there being progressive blood pneumothorax, open chest injury, pulmonary hernia, etc. Although the indications for the second situation included the requirement of the number of rib fractures and bicortical displacement, the flail chest, the dose of pain medication, and the pain score (26), they can all be classified as pain control. The surgical option is recommended when there are three or more rib fractures with obvious bicortical displacement. This recommendation is based on the previous studies concluded that there is a significant impact on respiratory function under this injury situation (39). This effect is mainly caused by pain limiting the respiratory movement and the effectiveness of coughing and drainage. For a flail chest patient, there is a greater amount and locations of the rib fractures. The impact and the feelings of pain will be more obvious. As mentioned in the previous section, flail chest patients would be required to use mechanical ventilation when the patients have a poor respiratory function. The flail chest patients with severe pulmonary contusion, the main purpose of using mechanical ventilation, which is also supported by Shackford et al., is to improve the barriers and disorders of ventilation exchange rather than the floating chest wall (40). The impact of abnormal breathing caused the disorder of respiratory function, and the pain would require internal surgical fixation to improve. Currently, although various guidelines suggest flail chest should be an indication for internal surgical fixation; clinically, not all of the flail chests are suitable for internal fixation. Especially when the flail chest injury is combined with other serious injuries, the early internal fixation surgery would not be a suitable and recommended treatment. Under this circumstance, the damage control principle should be considered first. Once other injuries and conditions damages are improved, the internal surgical fixation could be considered when it becomes appropriately. At this time, the main purpose of the strategy is to relieve pain and to reduce the occurrences of complications caused by the pain. Therefore, the managing strategy on flail chest injury should emphasize the combination of surgical and nonsurgical treatment, rather than a selection between one and another. We even believe that diluting the idea that the flail chest is the core surgical indication for rib fractures, would help to better understand the purpose of surgical treatment on multiple rib fractures without combined with a flail chest injury.
As described in the second situation, the dosage of the analgesic medicine used, and the analgesic effects are surgical indicators. Moreover, they can be directly related to pain management. If the core values of pain management are applied, we can more comprehensively cover all the situations that require internal surgical fixation. For example, injury with less than three rib fractures and costal cartilage fracture, etc. Therefore, the need for surgery is no longer defined by the number and locations of the fractures; rather, it is determined by the improvement after the treatment. Re-evaluation of the surgery options after an initial injury as damage control is also based on this criterion. However, pain is a relatively subjective indicator. It must be evaluated under the standardized pain assessment guideline after a standardized pain treatment. The surgical option should be evaluated by comparing the benefits of pain relief and the damage of the surgery itself. Otherwise, simply using pain relief as the only surgical indication can easily lead to excessive medical care problems.
The indications for the third situation, including chronic pain, chest wall collapse, etc., are related to the long-term quality of life. We will provide more detail description and discussion in the “Quality of Life” section (the fourth part) of this article.
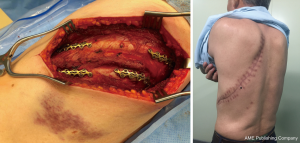
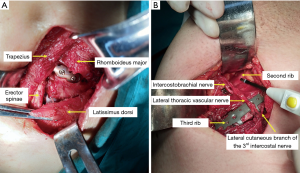
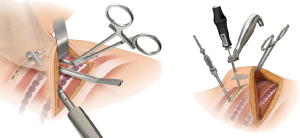
With the promotion and development of microinvasive surgery techniques, the concept of the microinvasive should be integrated into the internal surgical fixation as well. We should also protect the activity functions of the muscle and joint tissue as far as possible. Microinvasive incision has lesser damage and can reflect the surgery value as a more effective analgesic option and pain relief. For the internal fixation of rib fractures, large incisions and adequate exposure are not recommended (Figure 1). The incision selection criteria should be only based on fixation requirements. The concept applications of minimally invasive osteosynthesis (MIO) (Figure 2), biological osteosynthesis (BO), and minimally invasive plate osteosynthesis (MIPO) (Figure 3) are all shown the advantages of reducing tissue damage (Figure 4).

Fixation selection
As stated above, the purpose of the internal fixation for rib fractures should not be considered only from a recovery perspective of anatomical morphology, but more so it should be considered from the relief perspective of pathophysiological damage.
Multiple rib fracture injury does not require fixation for all fracture sites. Instead, a comprehensive injury assessment is necessary for the different fracture situations. First fixation priority should be applied on the fracture site with obvious physiological hazards. To eliminate and mitigate the hazards in mind, minimizing the damage of surgery should also be considered and evaluated. It is always critical to seek a balance between surgical damage and fixation benefit.
According to Tulay et al.’s (41) study, lateral fractures cause the most intense pain, followed by dorsal fractures, while anterior fractures are the lightest. Applying the pain control principle, the Dutch researchers concluded that lateral fractures should be the preferred fixation site because the lateral and lower ribs have a relatively larger degree of motion, and the effect on the pain is the greatest and obvious (35). Secondly, a dislocation friction of the fractured rib is the main cause of severe pain, and it should be closely monitored and actively treated. As the importance of the fracture dislocation impact, in 2013, the American Association for Surgery of Trauma and the American College of Surgeons have recommended the surgical interventions if the degree of fracture dislocation is wider than one rib cortical diameter. In 2017, the American Surgical Stabilization of Rib Fractures Rib Fracture Colloquium Clinical Practice Guidelines defined severely displaced fractures as exceeding the bicortical width of the rib (3).
The anatomic relationship around the rib fractures site is also a considering factor in fixation selection. Ribs 1 to 3 are in a deep position, which are difficult to expose and have relatively low mobility. The impacts on the respiration function are considered small if it was fractured. However, the sites of ribs 1 to 3 have important blood vessels and nerve tissues. The surgical risk is relatively high. Therefore, the internal fixation on these sites would be not recommended unless the fracture does involve damages to blood vessels and nerve tissue (26). As technology improves, experienced surgeons can consider the internal fixation in these areas. For the ribs 11 and 12 sites, because they are floating ribs, the separate fixation will be not recommended if there is no risk to liver and spleen damage. Posterior scapular fracture is typically in a deep position and relatively difficult for fixation operation. It will require a relatively larger incision and exposure, which results in relative larger damage. In the past, internal surgical fixation would be not recommended. Currently, the application of auscultation triangle helps to achieve the muscle sparing incision, which can reduce the surgical damage. This application turns the surgical fixation on these sites into a possible.
Moreover, the application of MIPO instruments can facilitate the operation of deep tissue and position, which also support the fixation in those sites. The stability of the thorax is mainly maintained by ribs 4 to 10 (42). The fixation selection should be prioritized on these sites. Once the middle part of the rib fractures is fixed in which can play the support role, the displacement and mobility of the uppermost and lower rib fractures are reduced, as well as the damage to the body of these fractures site is reduced. Under this situation, the fixation on those sites would be not strongly demanded as it would cause a longer incision and more tissue damages. We do not recommend the selective intermittent internal fixation as it does not provide merits, such as reducing trauma, to patients (26). In the case of posterior fractures of left ribs 5 to 9, if there is a potential risk that the fractured end can pierce the aorta to cause an aortic ulcer (43), and induces fatal bleeding, the internal surgical fixation will be strongly recommended.
Under the traditional internal fixation concept of the rib fractures, there is insufficient understanding of the importance and necessity of fixation. Many people think that elderly patients would have an increased surgical risk and the selected treatments on those are leaner to conservative treatment. However, this view could be wrong. Some literature reported that age over 65 is a high-risk factor for increasing death risk from rib fractures (44). However, Fitzgerald et al. (45) have a different view. They compared the outcomes of the surgical and nonsurgical treatment on patients, age over 65, with more than one rib fracture. So, they concluded that the patients’ mortality and respiratory complications were reduced after the internal surgical fixation. Because of the age, the post-injury pain would more likely than not cause respiratory insufficiency and cardiovascular and cerebrovascular complications. Therefore, for such patients, the internal surgical fixation can more effectively alleviate pain and improve respiratory function; and it also would be conducive to cough, expectoration, and improve pulmonary hygiene. Compared to young patients, the advantages of internal fixation on elder are more prominent.
Currently, the internal fixation materials are mostly metal, which is a lack of elasticity. Excessive fixation on rib fractures sites would indeed limit the movement of the chest wall, which will result in increasing postsurgical discomfort and harm long-term ventilation functions. Therefore, in the main purpose of achieving chest wall stabilization and pain relief, it is not necessary to fix each rib fractures site. It should be sufficient to select the right fixation amount of the fracture sites. On the other hand, compare to the metal materials, the absorbable materials have the advantages of elasticity, toughness, and no need for second removal operation, etc., which are the instrument materials development direction for the internal fixation.
Quality of life
Should we recommend surgical or nonsurgical treatment on rib fractures and flail chest? The 2005 RCT result from Germany concluded that both surgical and nonsurgical treatments show improved blood analysis, and there was no difference in mortality (28). In other words, it is not about which treatment would succeed or fail, rather a question of which one will be better under specific circumstances. For the patient, the consideration is not only about survivial but to live a better quality of life. In modern society, focusing on improving the quality of life is even more important than curing the disease itself.
The indicators of the short term treatment efficacy of rib fractures included acute pain, intubation time, ventilator application time, and time of early out-of-bed activities, etc.; the indicators of the long term treatment efficacy included the chronic pain after injury, vital capacity, return to work rate and return to work time, quality of life, and the appearance of the chest wall, and so on.
Followed up with 203 rib fractures patients without undergoing surgical treatment, Gordy et al. (46) analyzed patients’ post-treatment pain with the McGill Pain Questionnaire. They found that post-treatment pain exists in 22% of the patients after six months of the injury. It is worth to be aware that 89 patients with only a single rib fracture and the reported chronic pain rate on these patients are as high as 28%. Fabricant et al. (47) also found that the chronic pain rate reported is about 59% after two months of the injury. Tulay et al. (41) noticed that rib fractures patients have a higher pain score after half-month, three months, and six months after injury and required long-term pain relief medication. Especially for the older patients, the fracture healing would take a longer time, and the chronic pain caused by fractures dislocation is significantly severer than fractures without dislocation.
Improving the quality of life is one of the main reasons for choosing internal surgical fixation. A single medical center retrospective study (48) in Australia from 2005 to 2011 found that 397 patients with severe rib fractures under the conservative treatment group had a significant reduction in their quality of life, with only 50% being able to return to work within 6 months, and only 71% being able to return to work within 2 years. While, Khandelwal et al. (36) conducted a study including 67 patients, which 38 patients underwent surgical treatment. Patients with surgical treatment had a significant reduction in pain intensity and could return to work earlier. Undergoing the nonsurgical treatment, rib fracture patients with severe dislocation may have sequelae, such as thoracic deformity, decrease respiratory functions, and pseudarthrosis formation (28), etc. instead, the surgical treatment can effectively restore the appearance of the thorax, improve respiratory functions, eliminate the pseudarthrosis formation, and promote the recovery of body functions. Fagevik et al. (49) demonstrated that the range of thoracic motion of the patients with surgical treatment is significantly increased, and the standing, flexion and extension functions are significant dominant than patients with nonsurgical treatment. Moreover, the stability of the chest wall and long term pulmonary functions in the surgical group are much better than the nonsurgical group (28). After one-month follow-up study after injury, Tanaka et al. (27) also illustrated the surgical group could relatively quicker to resume work, and the respiratory functions were able to improve significantly compared to the nonsurgical group.
Conclusions
In this article, we concluded a four-core value of the rib fractures management, which are damage control, pain management, fixation selection, and quality of life. This four-core value does not only reveal the focus of rib fractures treatment but more importantly, it also outlines an ideal rib fractures treatment management process. In the admission stage, rib fractures patients should be first judged if whether there are other significant injuries and whether or not the injury control principle should be applied to these conditions. The internal surgical fixation should be centered on pain management. When the nonsurgical treatment is ineffective in providing pain relief, the surgical treatment should be actively applied to improve the relief. The selection of the surgical timing, fixation sites and numbers, surgical approaches and incision, and the fixation materials should be assessed and evaluated according to patient’s specific circumstances and needs. It is not necessary to fix each fracture site. Moreover, the evaluation of the treatment efficacy should include rapid short-term recovery and long-term improvement in the quality of life.
The treatment of multiple rib fractures requires a multidisciplinary management solution. It should be not limited to the application of only one certain kind of treatment. Both surgical and nonsurgical treatments have their focuses and advantages. We should change the wrong concepts of surgical and nonsurgical treatment from the past and improve our understanding. We should combine these two treatments and apply them effectively on different circumstances, which we believe this approach will bring the greatest benefits to patients.
Acknowledgements
Funding: This work was supported by the Medical, scientific research funds of Guangdong (A2017123), Military logistics research program (CGZ16C005) and Science and Technology Program of Guangzhou, China (201804010022).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Simon BJ, Cushman J, Barraco R, et al. Pain management guidelines for blunt thoracic trauma. J Trauma 2005;59:1256-67. [Crossref] [PubMed]
- Lafferty PM, Anavian J, Will RE, et al. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am 2011;93:97-110. [Crossref] [PubMed]
- Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: Surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury 2017;48:307-21. [Crossref] [PubMed]
- Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. [Crossref] [PubMed]
- Dehghan N, de Mestral C, McKee MD, et al. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg 2014;76:462-8. [Crossref] [PubMed]
- Mayberry JC, Ham LB, Schipper PH, et al. Surveyed opinion of American trauma, orthopedic, and thoracic surgeons on rib and sternal fracture repair. J Trauma 2009;66:875-9. [Crossref] [PubMed]
- Voggenreiter G, Neudeck F, Aufmkolk M, et al. Operative chest wall stabilization in flail chest--outcomes of patients with or without pulmonary contusion. J Am Coll Surg 1998;187:130-8. [Crossref] [PubMed]
- Farquhar J, Almahrabi Y, Slobogean G, et al. No benefit to surgical fixation of flail chest injuries compared with modern comprehensive management: results of a retrospective cohort study. Can J Surg 2016;59:299-303. [Crossref] [PubMed]
- Allen GS, Coates NE. Pulmonary contusion: a collective review. Am Surg 1996;62:895-900. [PubMed]
- Miller PR, Croce MA, Bee TK, et al. ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma 2001;51:223-8; discussion 229-30. [Crossref] [PubMed]
- Hamrick MC, Duhn RD, Ochsner MG. Critical evaluation of pulmonary contusion in the early post-traumatic period: risk of assisted ventilation. Am Surg 2009;75:1054-8. [PubMed]
- Strumwasser A, Chu E, Yeung L, et al. A novel CT volume index score correlates with outcomes in polytrauma patients with pulmonary contusion. J Surg Res 2011;170:280-5. [Crossref] [PubMed]
- Simon B, Ebert J, Bokhari F, et al. Management of pulmonary contusion and flail chest: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 2012;73:S351-61. [Crossref] [PubMed]
- McGee EM, Trinkle JK. Pulmonary contusion--pathogenesis and current management. Rev Surg 1972;29:224. [PubMed]
- Tanaka H, Tajimi K, Endoh Y, et al. Pneumatic stabilization for flail chest injury: an 11-year study. Surg Today 2001;31:12-7. [Crossref] [PubMed]
- Schweiger JW, Downs JB, Smith RA. Chest wall disruption with and without acute lung injury: effects of continuous positive airway pressure therapy on ventilation and perfusion relationships. Crit Care Med 2003;31:2364-70. [Crossref] [PubMed]
- Chan KP, Stewart TE. Clinical use of high-frequency oscillatory ventilation in adult patients with acute respiratory distress syndrome. Crit Care Med 2005;33:S170-4. [Crossref] [PubMed]
- Cinnella G, Dambrosio M, Brienza N, et al. Independent lung ventilation in patients with unilateral pulmonary contusion. Monitoring with compliance and EtCO(2). Intensive Care Med 2001;27:1860-7. [Crossref] [PubMed]
- Pape HC, Remmers D, Rice J, et al. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma 2000;49:496-504. [Crossref] [PubMed]
- Schild HH, Strunk H, Weber W, et al. Pulmonary contusion: CT vs plain radiograms. J Comput Assist Tomogr 1989;13:417-20. [Crossref] [PubMed]
- Lomoschitz FM, Eisenhuber E, Linnau KF, et al. Imaging of chest trauma: radiological patterns of injury and diagnostic algorithms. Eur J Radiol 2003;48:61-70. [Crossref] [PubMed]
- Miller LA. Chest wall, lung, and pleural space trauma. Radiol Clin North Am 2006;44:213-24. viii. [Crossref] [PubMed]
- Wanek S, Mayberry JC. Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury. Crit Care Clin 2004;20:71-81. [Crossref] [PubMed]
- Bastos R, Calhoon JH, Baisden CE. Flail chest and pulmonary contusion. Semin Thorac Cardiovasc Surg 2008;20:39-45. [Crossref] [PubMed]
- Hellinger A, Konerding MA, Malkusch W, et al. Does lung contusion affect both the traumatized and the noninjured lung parenchyma? A morphological and morphometric study in the pig. J Trauma 1995;39:712-9. [Crossref] [PubMed]
- Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg 2016;80:187-94. [Crossref] [PubMed]
- Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002;52:727-32; discussion 732. [Crossref] [PubMed]
- Granetzny A, Abd EM, Emam E, et al. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg 2005;4:583-7. [Crossref] [PubMed]
- Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg 2013;216:924-32. [Crossref] [PubMed]
- Brasel KJ, Moore EE, Albrecht RA, et al. Western Trauma Association Critical Decisions in Trauma: Management of rib fractures. J Trauma Acute Care Surg 2017;82:200-3. [Crossref] [PubMed]
- Girsowicz E, Falcoz PE, Santelmo N, et al. Does surgical stabilization improve outcomes in patients with isolated multiple distracted and painful non-flail rib fractures. Interact Cardiovasc Thorac Surg 2012;14:312-5. [Crossref] [PubMed]
- Michelitsch C, Acklin YP, Hässig G, et al. Operative Stabilization of Chest Wall Trauma: Single-Center Report of Initial Management and Long-Term Outcome. World J Surg 2018;42:3918-26. [Crossref] [PubMed]
- Slater MS, Mayberry JC, Trunkey DD. Operative stabilization of a flail chest six years after injury. Ann Thorac Surg 2001;72:600-1. [Crossref] [PubMed]
- Kasotakis G, Hasenboehler EA, Streib EW, et al. Operative fixation of rib fractures after blunt trauma: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 2017;82:618-26. [Crossref] [PubMed]
- Beks RB, Reetz D, de Jong MB, et al. Rib fixation versus non-operative treatment for flail chest and multiple rib fractures after blunt thoracic trauma: a multicenter cohort study. Eur J Trauma Emerg Surg 2018. [Epub ahead of print]. [PubMed]
- Khandelwal G, Mathur RK, Shukla S, et al. A prospective single center study to assess the impact of surgical stabilization in patients with rib fracture. Int J Surg 2011;9:478-81. [Crossref] [PubMed]
- Majercik S, Cannon Q, Granger SR, et al. Long-term patient outcomes after surgical stabilization of rib fractures. Am J Surg 2014;208:88-92. [Crossref] [PubMed]
- Diaz J SAM, Gasparri M LL, Pohlman T. Special report: Integrating surgical rib fixation into clinical practice: A report from the rib fracture consensus meeting. General Surgery News. 2013.
- Ahmad MA, Delli SE, Giannoudis PV. Assessment of severity of chest trauma: is there an ideal scoring system. Injury 2010;41:981-3. [Crossref] [PubMed]
- Shackford SR, Smith DE, Zarins CK, et al. The management of flail chest. A comparison of ventilatory and nonventilatory treatment. Am J Surg 1976;132:759-62. [Crossref] [PubMed]
- Tulay CM, Yaldiz S, Bilge A. Do we really know the duration of pain after rib fracture. Kardiochir Torakochirurgia Pol 2018;15:147-50. [Crossref] [PubMed]
- Sarani B, Schulte L, Diaz JJ. Pitfalls associated with open reduction and internal fixation of fractured ribs. Injury 2015;46:2335-40. [Crossref] [PubMed]
- Morimoto Y, Sugimoto T, Sakahira H, et al. Successful management of threatened aortic rupture late after rib fracture caused by blunt chest trauma. Ann Vasc Surg 2014;28:1035.e11-3. [Crossref] [PubMed]
- Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury 2012;43:8-17. [Crossref] [PubMed]
- Fitzgerald MT, Ashley DW, Abukhdeir H, et al. Rib fracture fixation in the 65 years and older population: A paradigm shift in management strategy at a Level I trauma center. J Trauma Acute Care Surg 2017;82:524-7. [Crossref] [PubMed]
- Gordy S, Fabricant L, Ham B, et al. The contribution of rib fractures to chronic pain and disability. Am J Surg 2014;207:659-62; discussion 662-3. [Crossref] [PubMed]
- Fabricant L, Ham B, Mullins R, et al. Prolonged pain and disability are common after rib fractures. Am J Surg 2013;205:511-5; discussion 515-6. [Crossref] [PubMed]
- Marasco S, Lee G, Summerhayes R, et al. Quality of life after major trauma with multiple rib fractures. Injury 2015;46:61-5. [Crossref] [PubMed]
- Fagevik Olsén M, Slobo M, Klarin L, et al. Physical function and pain after surgical or conservative management of multiple rib fractures - a follow-up study. Scand J Trauma Resusc Emerg Med 2016;24:128. [Crossref] [PubMed]


