
Pulmonary arteriovenous fistula: a rare cause of spontaneous hemothorax
Introduction
Pulmonary arteriovenous fistulas (PAVFs) are uncommon vascular malformations (1). Dyspnea and fatigue are the most common symptoms, with spontaneous hemothorax being a rare complication. Herein, we present a case with spontaneous hemothorax caused by the intrapleural rupture of the PAVF.
Case presentation
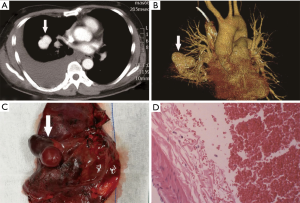
A 51-year-old male patient was admitted to our hospital due to severe right chest pain lasting 7 hours. Physical examination revealed signs of pleural effusion. Plain and contrast-enhanced chest computed tomography (CT) showed a large amount of fluid in the right chest cavity (Figure 1A), and an oval mass of about 4 cm in diameter in the right lower lobe, with the same density as a blood vessel (Figure 1B). A right thoracotomy and right lower lobectomy were performed. Approximately 1,000 mL of blood and 600 g of blood clot were found in the right thoracic cavity intraoperatively. The mass was located in the right lower lobe adjacent to the oblique fissure, with a diameter of about 4.5 cm (Figure 1C), and the blood flowed into the thoracic cavity through the pleural on the top of the lesion. Pathologic analysis revealed a PAVF in the lower lobe (Figure 1D). No postoperative complications occurred. The patient recovered successfully and was discharged from the hospital on the 8th day postoperatively.
Discussion
PAVF refers to a vascular malformation in which there is direct traffic between the pulmonary artery and pulmonary veins (1). Abnormal capillary development is considered to be the cause of PAVFs, including capillary dysplasia or disappearance of the vascular septum of the arteriovenous plexus (2). PAVF is rare (2 to 3 cases per 100,000 population), is more common in females than that in males, and most related lesions are located in the lower lobe (3-5).
Dyspnea and fatigue are the most common symptoms, and other clinical features include cyanosis, digital clubbing, and polycythemia (6). PAVF patients with thrombocytopenia are often accompanied by hemoptysis, but it is not common in those cases with spontaneous hemothorax caused by ruptures (7-9).
PAVF has a high mortality rate, which requires it to be treated in most patients. Major treatment approaches are angiographic interventional embolization and surgical resection, and most patients can be treated with angiographic embolization. However, surgical resection is the optimum treatment for the patients with large and central PAVFs, and those with short necks (1). Furthermore, PAVFs can also be treated by local excision since most of the lesions are located in the lung (10). Puskas and other authors reported the treatment therapy for PAVFs (see Table 1). In this case, PAVF was large and central; therefore, we performed lobectomy.
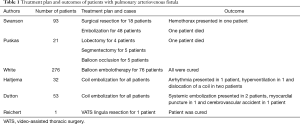
Full table
Conclusions
In conclusion, we reported a rare case of spontaneous hemothorax caused by the intrapleural rupture of PAVFs. All patients with PAVFs have a fatal risk of bleeding and should be treated promptly.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Pick A, Deschamps C, Stanson AW. Pulmonary arteriovenous fistula: presentation, diagnosis, and treatment. World J Surg 1999;23:1118-22. [Crossref] [PubMed]
- Anabtawi IN, Ellison RG, Ellison LT. Pulmonary arteriovenous aneurysms and fistulas. anatomical, variations, embryology, and classification. Ann Thorac Surg 1965;1:277-85. [Crossref] [PubMed]
- Hodgson CH, Kaye RL. Pulmonary Arteriovenous Fistula and Hereditary Hemorrhagic Telangiectasia: A Review and Report of 35 Cases of Fistula. Dis Chest 1963;43:449-55. [Crossref] [PubMed]
- Dines DE, Arms RA, Bernatz PE, et al. Pulmonary arteriovenous fistulas. Mayo Clin Proc 1974;49:460-5. [PubMed]
- Puskas JD, Allen MS, Moncure AC, et al. Pulmonary arteriovenous malformations: therapeutic options. Ann Thorac Surg 1993;56:253-7; discussion 257-8. [Crossref] [PubMed]
- Shumacker HB Jr, Waldhausen JA. Pulmonary arteriovenous fistulas in children. Ann Surg 1963;158:713-20. [Crossref] [PubMed]
- Dalton ML Jr, Harry JD. Experimental pulmonary arteriovenous fistulas. Surg Forum 1960;11:209-11. [PubMed]
- Spear BS, Sully L, Lewis T. Pulmonary arteriovenous fistula presenting as spontaneous haemothorax. Thorax 1975;30:355-6. [Crossref] [PubMed]
- Kotsuka Y, Konishi T, Fujita M, et al. A case of intrapleural rupture of pulmonary arteriovenous fistula (author's transl). Kyobu Geka 1981;34:146-9. [PubMed]
- Dines DE, Clagett OT, Bonebrake RA. Hereditary telangiectasia and pulmonary fistula. Case of large right-to-left shunt surgically corrected. Arch Intern Med 1967;119:195-7. [Crossref] [PubMed]
(English Language Editor: Gray John Ayric, AME Publishing Company)


