
Risk factors for recurrence of primary spontaneous pneumothorax after thoracoscopic surgery
Introduction
Surgery represents the most effective treatment for preventing recurrence of spontaneous pneumothorax. Thoracoscopic surgery is widely performed for spontaneous pneumothorax. However, the recurrence rate of pneumothorax after thoracoscopic surgery is higher than that for open thoracotomy (1,2). The reasons underlying the high recurrence rate after thoracoscopic surgery are speculated to be the fewer adhesions observed after thoracoscopic surgery than after thoracotomy, and failure to identify bullae intraoperatively. However, the factors affecting the high recurrence rate after thoracoscopic surgery remain unclear. The aim of this study was to identify the risk factors for postoperative recurrence for primary spontaneous pneumothorax after thoracoscopic surgery.
Methods
This study was approved by the institutional review board, and the informed consent requirement was waived. A retrospective review was conducted on all consecutive patients aged <50 years who underwent thoracoscopic surgery for primary spontaneous pneumothorax at Jikei University Hospital from January 2010 to December 2016. The age, sex, body mass index (BMI), smoking history, serum albumin level, degree of pneumothorax, history of ipsilateral pneumothorax, degree of emphysema, identification of bullae before surgery on computed tomography (CT), surgical procedure, and follow-up time were evaluated. All surgeries were performed by the same surgical team. Bullae or blebs were resected with a stapling device. In some patients, staple line coverage was performed with a polyglycolic acid (PGA) sheet with fibrin glue at the surgeon’s discretion. A follow-up was conducted for all patients. All the statistical analyses were performed with EZR statistical software (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) (3). Categorical variables were evaluated using the chi-square test and the t-test was utilized to analyze continuous variables between the two groups. In addition, follow-up analysis using time-to-event data was also performed, with the event rates estimated bay Kaplan-Meier methods and compared with log-rank test. Differences with P values of <0.05 were considered to be statistically significant.
Results
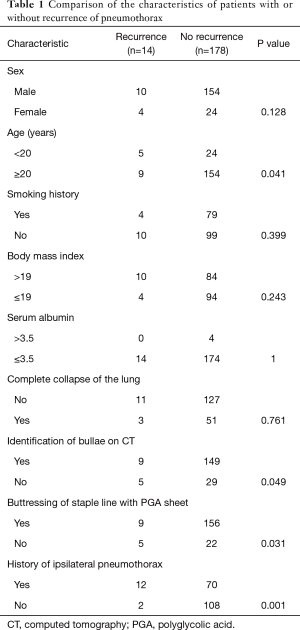
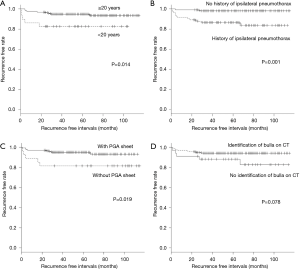
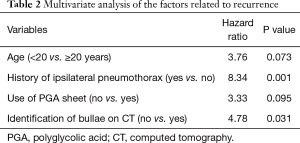
We identified 192 patients who underwent thoracoscopic surgery. Of these 192 patients, ipsilateral recurrence occurred in 14 (7.3%). The differences in sex, smoking history, BMI, and serum albumin level between the patients with and without recurrence were not significant (Table 1). The incidence of recurrence was higher in the patients aged <20 years than in the patients aged ≥20 years (P=0.041). Complete lung collapse on chest roentgenogram was not related to the postoperative recurrence of pneumothorax. Identification of bullae on preoperative CT was associated with a lower recurrence rate. The incidence of recurrence was higher in the patients who did not undergo intraoperative staple line reinforcement with PGA sheets (P=0.031), and in those with a history of ipsilateral pneumothorax (P=0.001). Kaplan-Meier curves for age, history of ipsilateral pneumothorax, the use of PGA sheet, and the identification of bullae on CT are shown in Figure 1. Patients aged <20 years, the history of ipsilateral pneumothorax, the use of PGA sheet were related to recurrence of pneumothorax (P<0.05). Identification of bullae on CT was marginally related to recurrence (P=0.078). Multivariate analysis revealed that history of ipsilateral pneumothorax, and negative preoperative identification of bullae on CT were related to recurrence of pneumothorax (Table 2).
Full table
Full table
The clinical details of the 14 patients who experienced postoperative recurrence are provided in Table 3. There were eight patients in which pneumothorax recurred within 1 year of surgery. The median time from surgery to recurrence was 5.5 months.

Full table
Discussion
Thoracoscopic surgery for spontaneous pneumothorax is currently established as a standard surgical procedure. However, recurrence of pneumothorax after thoracoscopic surgery has been reported to occur in 5–19% of patients (4-6). Nonetheless, the specific reasons underlying pneumothorax recurrence after thoracoscopic surgery remain unclear, and prevention of recurrence remains a challenge for thoracic surgeons.
We evaluated the risk factors for postoperative recurrence of primary spontaneous pneumothorax in patients who underwent thoracoscopic surgery. We found that patients aged <20 years had a higher recurrence rate in the univariate analysis. Five of 29 patients aged <20 years experienced recurrence of pneumothorax, and four of these patients did not have reinforcement with PGA sheets. We believe that the low rate of PGA sheet use may have influenced the results. Another reason for the higher incidence of recurrence in the younger population is that the rapid development of the body in younger patients causes imbalance of the body and lungs, which leads to fragility of the visceral pleura (7). We also found that patients aged <20 years, the history of ipsilateral pneumothorax, the use of PGA sheet were related to recurrence of pneumothorax in the time dependent analysis.
Preoperative identification of bullae on CT was associated with a lower incidence of postoperative recurrence in the univariate and multivariate analyses. We identified bullae on preoperative CT in 158 of 192 patients (82.3%), which was a similar finding to that of a previous study (8). We speculate that the reason for the lower recurrence rate in the patients in whom bullae were identified on preoperative CT was that such identification leads to easier intraoperative detection of bullae, resulting in appropriate resection of the bullae and a consequent decrease the recurrence rate. We also found that the size of the pneumothorax was not related to postoperative recurrence, which was comparable with the findings of a previous study (9). Staple line coverage with PGA sheets resulted in a lower incidence of postoperative recurrence of pneumothorax as determined by the univariate analysis. Postoperative recurrence of pneumothorax is speculated to result from the formation of new blebs adjacent to the staple line, or incomplete resection of bullae at the time of surgery. Applying a PGA sheet to the resection margin causes inflammation of the pleura and accompanying infiltrations of eosinophils and macrophages (10), resulting in reinforcement of the pleura.
The multivariate analysis indicated that a preoperative history of ipsilateral pneumothorax was a significant risk factor for recurrence after surgery. This is the first report that a preoperative history of ipsilateral pneumothorax was related to the postoperative recurrence. We were unable to determine the exact reason for this finding. However, a history of ipsilateral pneumothorax may be related to fragility of the visceral pleura, which might be a risk for postoperative recurrence. The median time from surgery to recurrence in this study was 5.5 months. We believe it is necessary to conduct careful observation for 1 year after surgery.
This study has several limitations, including the fact that this was a retrospective, single-center study. In addition, although the number of the patients included in this study was large, only 14 patients experienced recurrence. Furthermore, selection bias may have been present, which limits the power of the statistical analysis.
Conclusions
A history of ipsilateral pneumothorax, and negative preoperative identification of bullae on CT were risk factors for postoperative recurrence of pneumothorax.
Acknowledgments
None
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional review board (IRB) approval for this study was obtained from the Medical Research Ethics Committee of Jikei University (approval number 30-245). Informed consent was waived by the IRB because of the retrospective nature of this study.
References
- Sawada S, Watanabe Y, Moriyama S. Video-assisted thoracoscopic surgery for primary spontaneous pneumothorax: evaluation of indications and long-term outcome compared with conservative treatment and open thoracotomy. Chest 2005;127:2226-30. [Crossref] [PubMed]
- Uramoto H, Shimokawa H, Tanaka F. What factors predict recurrence of a spontaneous pneumothorax? J Cardiothorac Surg 2012;7:112. [Crossref] [PubMed]
- Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 2013;48:452-8. [Crossref] [PubMed]
- Sudduth CL, Shinnick JK, Geng Z, et al. Optimal surgical technique in spontaneous pneumothorax: a systematic review and meta-analysis. J Surg Res 2017;210:32-46. [Crossref] [PubMed]
- Lee S, Kim HR, Cho S, et al. Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 2014;98:2005-11. [Crossref] [PubMed]
- Horio H, Nomori H, Kobayashi R, et al. Impact of additional pleurodesis in video-assisted thoracoscopic bullectomy for primary spontaneous pneumothorax. Surg Endosc 2002;16:630-4. [Crossref] [PubMed]
- Fujino S, Inoue S, Tezuka N, et al. Physical development of surgically treated patients with primary spontaneous pneumothorax. Chest 1999;116:899-902. [Crossref] [PubMed]
- Kawaguchi T, Kushibe K, Yasukawa M, et al. Can preoperative imaging studies accurately predict the occurrence of bullae or blebs? Correlation between preoperative radiological and intraoperative findings. Respir Investig 2013;51:224-8. [Crossref] [PubMed]
- Choi SY, Park CB, Song SW, et al. What factors predict recurrence after an initial episode of primary spontaneous pneumothorax in children? Ann Thorac Cardiovasc Surg 2014;20:961-7. [Crossref] [PubMed]
- Kuwata T, Shinohara S, Takenaka M, et al. The impact of covering the bulla with an absorbable polyglycolic acid (PGA) sheet during pneumothorax surgery. Gen Thorac Cardiovasc Surg 2016;64:558-60. [Crossref] [PubMed]


