
Influence of marital status in patients undergoing transcatheter aortic valve implantation
Introduction
Transcatheter aortic valve implantation (TAVI) has been shown to be superior to surgical aortic valve replacement (SAVR) in high-risk patients (1) and non-inferior in intermediate-risk patients (2,3). Therefore, the use of this treatment option is rapidly increasing especially among an elderly, multimorbid patient population. With increasing operator experience, improved patient selection as well as continuous evolution of prosthetic valves and refinement of delivery systems, a considerable improvement in outcomes has been achieved with a reduction of 1-year mortality from 24% to 12% with older and newer generation devices (2,4). In addition to procedural factors, mortality rates are known to be influenced by age, higher pre-operative risk, alternative access sites (5,6).
Several baseline risk factors have been identified in patients undergoing TAVI, so far (7,8). Marital status has been associated with differences in survival and clinical outcomes for a variety of medical conditions including cardiovascular diseases (9-11). Results after cardiovascular surgery, interventions for acute coronary syndrome, elective percutaneous interventions, and cardiac bypass graft surgery have been shown to correlate with marital status (12-15). To date, the influence of marital status and its impact on prognosis in patients undergoing TAVI has not been evaluated. Therefore, we sought to investigate whether unmarried patients are at an increased risk for adverse outcome, i.e., at one year after TAVI compared to married patients.
Methods
Patient population
Between April 2011 and November 2015, 810 patients underwent transfemoral TAVI for severe aortic valve stenosis or bioprosthesis degeneration at the Klinik für Herz-und Kreislauferkrankungen, Deutsches Herzzentrum München, Munich, Germany. Of these, 779 patients (96.2%) had available information on marital status and formed the final study population. All patients were considered suitable for the procedure by an interdisciplinary Heart Team and provided written informed consent prior to the procedure and were included in the AVIATOR TAVI registry (NCT01390675; institutional ethics review board no. 5081/10). Data were prospectively collected according to the updated Valve Academic Research Consortium (VARC)-2 criteria (16). All procedures performed were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Follow-up and definition of endpoints
Follow-up was obtained by direct patient contact at our outpatient clinic, by contacting the treating physician or by telephone, and censored at one year or last contact, respectively. Follow-up was complete in 99.1% of the final study population.
For the purpose of this analysis, patients were divided into two groups according to marital status at time of TAVI: married or in a stable relationship, henceforth “married”; and unmarried, which included divorced, separated, widowed and single patients.
The primary endpoint of the study was cardiac death or need for hospitalization for congestive heart failure (CHF) at one year. Secondary endpoints were all-cause and cardiac mortality, as well as re-hospitalization for CHF at one year.
Statistical analysis
Continuous variables are expressed as mean ± SD or as median (interquartile range) and were compared using the unpaired Student’s t-test or Mann-Whitney U test, as appropriate. Discrete variables were compared using the chi-square test or Fisher's exact test, as necessary. Survival distribution during follow-up was estimated using the Kaplan-Meier method and compared with the log-rank test. A Cox proportional regression model with computation of hazard ratios (HR) and 95% Confidence Intervals (CI) was used to assess the association of marital status with the primary endpoint. To avoid overfitting, selection of covariates in the multivariate Cox regression model was performed using the least absolute shrinkage and selection operator regression method after entering all baseline characteristics as candidates (R package “glmnet”, version 2.0-13). The resulting variables for the multivariate Cox regression model were marital status, age, New York Heart Association (NYHA) III/IV, chronic obstructive pulmonary disease (COPD), glomerular filtration rate, peripheral artery disease, previous stroke, previous coronary artery bypass graft (CABG), SAVR, previous malignancy, previous pacemaker, as well as left ventricular ejection fraction (LVEF), aortic valve area, mean transvalvular gradient and pulmonary hypertension. Missing baseline data were imputed using the predictive mean matching function (R package mice, version 2.46). Hosmer-Lemeshow test was used in a binomial logistic regression to evaluate whether expected and observed event rates in subgroups are well calibrated (Chi-square 3.6, P=0.89). The proportional hazards assumption was tested using the cox.zph function (R package “survival”, version 2.43-3) and revealed that the assumption of proportionality was not violated (marital status: rho 0.12363, Chi-square 1.14, P=0.29; global P=0.67).
To account for gender related differences on the effect of marital status a subgroup analysis was conducted for male and female patients. The selection of covariates for computing multivariate models for these subgroups were performed as described above.
A two-sided P value <0.05 was considered statistically significant for all analyses. IBM SPSS Statistics version 24 (SPSS Inc., Chicago, IL, USA) and R (Version 3.4.3, R Foundation for Statistical Computing, Vienna, Austria) were employed.
Results
Patient population, and in-hospital outcome according to marital status
A total of 779 patients with known marital status underwent transfemoral TAVI and were included in the analysis. Mean age was 80.7±5.9 years, 47.8% were female and median logistic EuroScore was 12.7% (8.13–19.39%). Among the study population 56.7% were married or in a stable relationship at the time of procedure. Table 1 depicts baseline characteristics according to marital status, showing significant differences between the two groups. Compared to married patients, unmarried patients were older (82.4±5.5 vs. 79.5±5.8 years; P<0.001), more often female (73.3% vs. 28.3%; P<0.001), and presented with a higher logistic EuroScore [13.1% (9.5–21.5%) vs. 11.7% (7.0–18.5%); P<0.001] reflecting a higher burden of comorbidities. Furthermore, patients in the unmarried group were more symptomatic, i.e., more individuals presented with NYHA functional class III/IV at baseline compared to married patients (69.7% vs. 60.6%; P=0.009). Conversely, married patients had higher rates of previous clinical manifestation for coronary artery disease, previous myocardial infarction, previous percutaneous coronary intervention, as well as previous malignancy. While LVEF did not significantly differ between the groups, unmarried patients displayed smaller aortic valve areas.
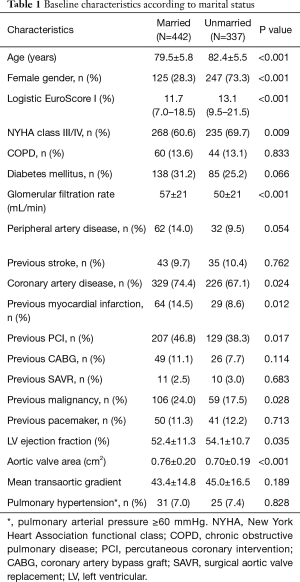
Full table
Overall, procedures were performed under general anesthesia in 64.7% and balloon-expandable prostheses were deployed in 82.0% of cases. Device success was reached in 89.6% of cases and in-hospital mortality was 1.4%. Procedural and in-hospital outcome showed no significant differences according to marital status and are displayed in Table 2.
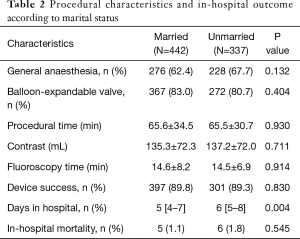
Full table
Outcome at one year
At one year, all-cause mortality in the whole population was 10.5%. Table 3 displays outcomes at one year according to marital status. The unmarried population showed higher rates of the composite of cardiac death and CHF (18.7% vs. 12.0%; P=0.011; Figure 1A). While there was no difference in all-cause mortality (10.7% vs. 10.4%; P=0.879), unmarried patients more frequently experienced hospitalization for CHF at one year compared to married patients (14.1% vs. 7.8%; P=0.007). Figure 1B shows Kaplan-Meier survival curves for hospitalization for CHF according to marital status. Neither stroke rate nor the composite of death and stroke varied according to marital status (Figure 1C,D).
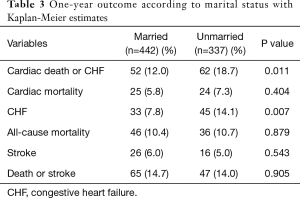
Full table
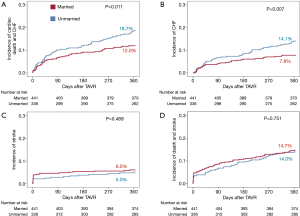
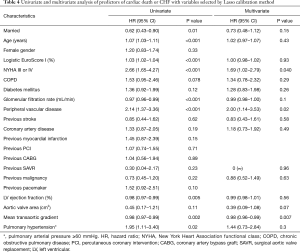
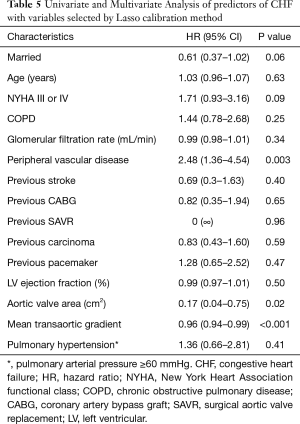
Results of the univariate and multivariate analyses for the primary endpoint are represented in Table 4. After multivariable adjustment, only NYHA class III/IV, peripheral artery disease and mean transaortic gradient persisted as independent predictors of the primary endpoint. Marital status was borderline significant with regard to CHF (HR 0.61; 95% CI: 0.37–1.02; P=0.06; Table 5) but not the primary endpoint (HR 0.73; 95% CI: 0.48–1.12; P=0.15).
Full table
Full table
Gender related outcome
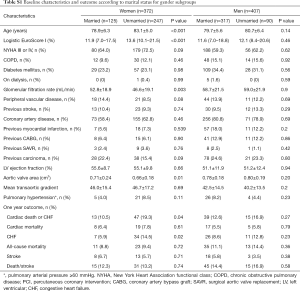
Subgroup analyses were performed to assess gender-related differences in outcome after TAVI depending on marital status. Baseline characteristics and outcome according to marital status for each gender are shown in Table S1. While there were neither differences in baseline characteristics nor in outcomes according to marital status in the male population, significant differences were identified in women: unmarried female patients were older, had a higher preoperative risk score assessed by logistic EuroScore, worse renal function, and smaller aortic annuli compared to married patients. Rates of cardiac death or CHF (19.3% vs. 10.5%; P=0.038) were higher in unmarried women during the first year after TAVI and this group more often required hospitalization for CHF during the first year after TAVI (14.5 vs. 5.9%; P=0.022).
Full table
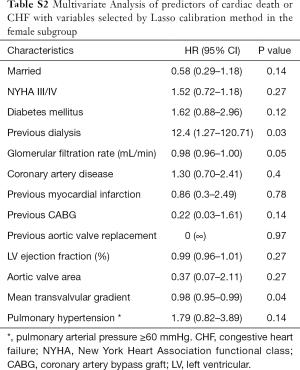
A multivariate analysis was performed to identify independent risk predictors for the primary endpoint in both subgroups and is depicted in Tables S2 and S3 for women and men, respectively. For the female subgroup only previous dialysis, glomerular filtration rate and mean transvalvular gradients were predictors for the primary endpoint, while marital status showed no significant impact (HR 0.58; 95% CI: 0.29–1.18; P=0.14). In the male subgroup age, NYHA class III/IV and peripheral artery disease were independent predictors for the primary endpoint.
Full table
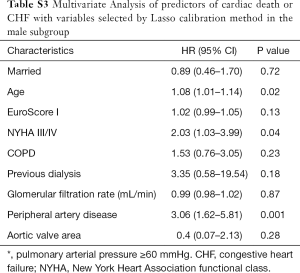
Full table
Regarding CHF, marital status in females persisted as independent predictor (HR 0.37; 95% CI: 0.14–0.96; P=0.04) along with older age, decreased glomerular filtration rate, smaller aortic valve area, lower transvalvular gradient and higher pulmonary pressure (Table S4). Marital status showed no significant association with the primary endpoint in the male subgroup (Table S5).
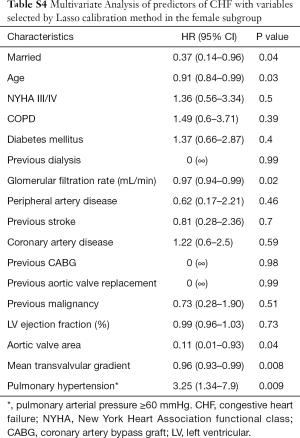
Full table

Full table
Discussion
To our knowledge, this is the first analysis investigating the association between marital status and outcome in patients undergoing TAVI. Compared to the married population, unmarried patients displayed a higher risk of cardiac death or CHF at one year after TAVI which was due to more frequent hospitalizations for CHF. This effect was mainly driven by the outcome in female patients where marital status persisted as an independent factor of the primary endpoint even after multivariable adjustment.
In general, a trend towards lower rates of events in married patients has been observed in a variety of diseases. A study performed two decades ago in patients undergoing coronary artery bypass surgery revealed that married patients were 2.5 times more likely to be alive after 15 years compared to unmarried patients (13). Furthermore, a recent study in patients undergoing percutaneous revascularization also reported higher cardiovascular event rates in unmarried compared to married patients (14). Our results are in line with these studies showing that unmarried patients have higher event rates during the first year after TAVI.
The underlying reasons for an association between marital status and clinical outcomes remain speculative so far. An influence of psycho-social as well as biological factors has been postulated. Oncologists have reported higher rates of distress in unmarried patients (17). It is plausible, that this observation might not be restricted to patients suffering from cancer. Another important factor is that being unmarried might be associated with reduced social support. As a result, being married has been reported to be associated with a higher probability of medication adherence and a lower likelihood of smoking (18). As medication adherence was not investigated in this study, it was not possible to analyze whether this factor could be relevant in our population.
Another potential explanation is a confounding effect due to older age of unmarried, mostly widowed patients. In our cohort unmarried patients were older than married patients and furthermore displayed a higher operative risk in terms of a higher logistic EuroScore. Nevertheless, particularly in female patients, marital status persisted as an independent predictor of CHF, even after multivariable adjustment. Moreover, unmarried patients displayed smaller aortic valve areas and were more symptomatic which might be a result of advanced disease due to late admission. Being married is likely associated with increased social support resulting in an earlier presentation at cardiology departments compared with unmarried counterparts lacking spouses recommending presentation. This hypothesis is further supported by the fact that adjusting for differences between the overall study groups resulted in loss of statistical significance although a trend towards lower incidence of the outcome persisted in married individuals.
Taken together, we conclude that unmarried patients undergoing TAVI are at higher risk for unfavorable outcomes during follow-up after TAVI. This may be due to an advanced disease status and lack of social support. Whether closer follow-up with enhanced medical care for unmarried patients improves clinical outcomes remains to be investigated.
Limitations
Albeit enrolling more than 700 patients and being the first analysis to assess the influence of marital status on clinical outcome after TAVI, this study has several limitations. First, this is a single center, retrospective, non-randomized study with intrinsic potential confounders. Mortality in the population with unknown marital status was significantly higher than in the study population (32.3% vs. 10.5%; P<0.001), potentially suggesting a selection bias. Secondly, there are significant differences in baseline characteristics between the two groups, especially gender and age, which may have influenced the outcome. Thirdly, we only had access to information on marital status and relationships to partners; however we were unable to determine whether patients were living in nursing homes or with other close family members, e.g., children. Finally, we did not have information about changes in marital status during time of follow-up. Thus, we cannot exclude that changes in marital status might have influenced the outcome.
Conclusions
This first analysis on the influence of marital status on outcome after TAVI revealed that, albeit not being an independent predictor, unmarried patients are at higher risk for hospitalization for CHF at one year after TAVI. Although this study has some limitations, these results indicate that, similar to other cardiovascular procedures, unmarried patients might demand more intensive medical care than married patients. Whether intensified management of unmarried patients is able to improve outcomes remains unknown.
Acknowledgments
This work was supported by the German Research Foundation (DFG) and the Technical University of Munich within the funding programme Open Access Publishing.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: All patients were provided written informed consent prior to the procedure and were included in the AVIATOR TAVI registry (NCT01390675; institutional ethics review board no. 5081/10).
References
- Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011;364:2187-98. [Crossref] [PubMed]
- Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2016;374:1609-20. [Crossref] [PubMed]
- Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or Transcatheter Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2017;376:1321-31. [Crossref] [PubMed]
- Holmes DR Jr, Brennan JM, Rumsfeld JS, et al. Clinical outcomes at 1 year following transcatheter aortic valve replacement. JAMA 2015;313:1019-28. [Crossref] [PubMed]
- Van Belle E, Juthier F, Susen S, et al. Postprocedural aortic regurgitation in balloon-expandable and self-expandable transcatheter aortic valve replacement procedures: analysis of predictors and impact on long-term mortality: insights from the FRANCE2 Registry. Circulation 2014;129:1415-27. [Crossref] [PubMed]
- Herrmann HC, Thourani VH, Kodali SK, et al. One-Year Clinical Outcomes With SAPIEN 3 Transcatheter Aortic Valve Replacement in High-Risk and Inoperable Patients With Severe Aortic Stenosis. Circulation 2016;134:130-40. [Crossref] [PubMed]
- Zahn R, Gerckens U, Linke A, et al. Predictors of one-year mortality after transcatheter aortic valve implantation for severe symptomatic aortic stenosis. Am J Cardiol 2013;112:272-9. [Crossref] [PubMed]
- Rheude T, Pellegrini C, Michel J, et al. Prognostic impact of anemia and iron-deficiency anemia in a contemporary cohort of patients undergoing transcatheter aortic valve implantation. Int J Cardiol 2017;244:93-9. [Crossref] [PubMed]
- Wong CW, Kwok CS, Narain A, et al. Marital status and risk of cardiovascular diseases: a systematic review and meta-analysis. Heart 2018;104:1937-48. [Crossref] [PubMed]
- Seymour CW, Iwashyna TJ, Cooke CR, et al. Marital status and the epidemiology and outcomes of sepsis. Chest 2010;137:1289-96. [Crossref] [PubMed]
- Aizer AA, Chen MH, McCarthy EP, et al. Marital status and survival in patients with cancer. J Clin Oncol 2013;31:3869-76. [Crossref] [PubMed]
- Hadi Khafaji HA, Al Habib K, Asaad N, et al. Marital status and outcome of patients presenting with acute coronary syndrome: an observational report. Clin Cardiol 2012;35:741-8. [Crossref] [PubMed]
- King KB, Reis HT. Marriage and long-term survival after coronary artery bypass grafting. Health Psychol 2012;31:55-62. [Crossref] [PubMed]
- Barbash IM, Gaglia MA Jr, Torguson R, et al. Effect of marital status on the outcome of patients undergoing elective or urgent coronary revascularization. Am Heart J. 2013;166:729-36. [Crossref] [PubMed]
- Schultz WM, Hayek SS, Samman Tahhan A, et al. Marital Status and Outcomes in Patients With Cardiovascular Disease. J Am Heart Assoc (Internet) 2017. doi: . [Crossref]
- Kappetein AP, Head SJ, Généreux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur J Cardiothorac Surg 2012;42:S45-60. [Crossref] [PubMed]
- Goldzweig G, Andritsch E, Hubert A, et al. Psychological distress among male patients and male spouses: what do oncologists need to know? Ann Oncol 2010;21:877-83. [Crossref] [PubMed]
- Trivedi RB, Ayotte B, Edelman D, et al. The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J Behav Med 2008;31:489-97. [Crossref] [PubMed]


