
Verification of meta-analysis and propensity-matched analysis comparing stereotactic body radiation therapy versus surgery for early stage lung cancer
Stereotactic body radiation therapy (SBRT) has been recognized as a standard radical treatment for medically inoperable patients with stage I non-small cell lung cancers (NSCLCs). However, evaluation of SBRT in medically operable patients has shown widely varying results. Evidence-based guidelines published by the American Society for Radiation Oncology (ASTRO) in 2017 (1) prudently expressed that SBRT is not recommended as an alternative to surgery outside of a clinical trial setting. Contrastingly, the National Comprehensive Cancer Network (NCCN) guidelines published in 2018 (2) presented that SBRT is recommended for patients who are medically inoperable or who refused to undergo surgery after thoracic surgery evaluation. SBRT has been reported to achieve primary tumor control and overall survival (OS) rates that are comparable to those achieved with lobectomy by nonrandomized and population-based comparative studies involving older patients. SBRT is an appropriate option for patients with high surgical risk [those able to tolerate sublobar resection but not lobectomy (e.g., age ≥75 years, poor lung function)]. Additionally, a combined analysis of two randomized trials that compared SBRT with lobectomy in operable patients (3) was ignored in the ASTRO guidelines but was referred to in the NCCN guidelines. How are physicians and patients meant to interpret these guidelines?
Verification of a recent meta-analysis
Recently, Cao et al. reported a systematic review and meta-analysis of SBRT versus surgery for NSCLC patients (4). The main points described in this meta-analysis and the corresponding verifications are given below.
Point 1: the current evidence suggests that surgery is superior to SBRT in terms of mid- and long-term clinical outcomes
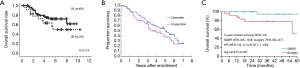
Personal verification: this suggestion is doubtful. The results of OS argued hear (4) and in other major meta-analysis (5,6) were shown in Figure 1. The OS associated with SBRT in medically operable patients reported in the study argued hear (4) (Figure 1A) was much poorer than that reported in the retrospective survey, prospective phase II, and randomized studies by Onishi et al. (7) (Figure 2A), Nagata et al. (8) (Figure 2B), or Chang et al. (9) (Figure 2C), respectively. Age was excluded from the criteria, therefore the highest age was 87, 91, and 82 years old, respectively in each of these studies shown in Figure 2. Nevertheless, the OS was much higher than that reported in the meta-analysis. Furthermore, the OS associated with SBRT in medically operable patients in this meta-analysis was inferior to that in inoperable patients in the JCOG 0403 study (8). This is an absurd conclusion. The reason for worse OS may be the presence of medically inoperable patients in the SBRT subgroup, who had some characteristics that made them eligible for surgery but also had characteristics that made them ineligible for surgery; however, the latter characteristics were not detected with the used inclusion criteria. Although these 3 studies (7-9) had small study populations (et al. reported an SBRT-associated OS that was comparable to surgery-associated OS (10). With regards to follow-up duration, the studies by Onishi (7) and Nagata (8) had median follow-up durations of >50 months. However, I agree that SBRT needs long-term (>10 years) clinical outcomes of a big number of patients. Contrastingly, Zheng et al. (5) reported a completely reverse result of meta-analysis shown in Figure 1B, and Chen et al. (6) reported that overall survival depended on first-author specialty in a meta-analysis of propensity score studies (Figure 1C).

Most pulmonary surgeons do not consider SBRT to be comparable to surgery in terms of overall survival, because SBRT is only a focal therapy that has been historically contradicted for stage I NSCLC cases (11) not involving histopathological examination of regional lymph nodes. However, SBRT is considered to have immunogenic effects, in addition to the DNA-mediated effect of X-rays (12). This may be one of the mysterious reasons why SBRT-associated OS is comparable to surgery-associated OS.
Point 2: SBRT is associated with low perioperative mortality
Personal verification: this assertion is not doubtful; however, severe SBRT-related complications have been reported in cases involving centrally located tumors (13). Generally, surgery can be used to treat such tumors.
Point 3: however, the improved outcomes after surgery may be at least partly due to an imbalance in baseline characteristics
Personal verification: This is a very precise expression. Performance status and frailty are not fully matched in most propensity score matching studies. Medical operability is judged differently by institutions and physicians (14). A few patients in the SBRT cohort who were judged as being medically operable would have had different physical status compared to that of patients in the surgical cohort.
Point 4: future studies should aim to provide histopathologic confirmation of malignancy and should compare SBRT with minimally invasive anatomical resections
Personal verification: the aforementioned studies on SBRT for medically operable patients (Figure 2) reported better OS than that reported by the meta-analysis by Cao et al., even though all cases enrolled in these studies were histopathology-proven (7,8). Verstegen reported no differences between pathologically proven and unproven cohorts (15). Furthermore, from the viewpoint of a radiation oncologist, OS must only be compared in cases in which histopathology was confirmed “before surgery”; this is because some cases in the surgery group show ground-glass nodules (GGNs) that are generally proven to be non-invasive or minimally invasive tumor post-operation and that result in good prognosis(16); it is difficult to confirm GGN histopathology by preoperative biopsy. One of the reasons for better prognosis in the surgical cohort may be the higher proportion of patients with GGNs than that in the SBRT cohort.
“Not recommended” is not “contradicted”
What is the definition of a particular guideline and how should it be applied for patient care? In the field of cancer treatment, a standard treatment is defined as an orthodox treatment or a treatment that has been used for the longest time period in terms of time after a comparison study. Because of individual measurements other than survival time, the standard treatment always cannot be considered as the best choice for all patients. In addition, SBRT generally has an advantage in terms of better quality of life and low medical cost (17). Therefore, even with strict adherence to the ASTRO guidelines (1), selection of SBRT for early stage NSCLC patients who prefer SBRT to surgery, which is recommended by the NCCN guidelines (2), is considered acceptable and reasonable. Actually, Haque et al. reported an increase in radiotherapy utilization and a decrease in surgical utilization for treatment of early stage NSCLCs after radiation oncologists incorporated SBRT as a treatment option in the United States (18).
Collaboration between pulmonary surgeons and radiation oncologists: “SBRT is recommended as an alternative to surgery in clinical trials”
The final comparison of SBRT vs. surgery must be performed in a randomized setting. “SBRT is not recommended as an alternative to surgery outside of a clinical trial”, as mentioned in the ASTRO guidelines (1), could be interpreted as “SBRT is recommended as an alternative to surgery in clinical trial”. Currently, the following four randomized studies have been comparing SBRT with surgery for early stage lung cancer: NCT02984761; Veterans Affairs Lung Cancer Surgery Or Stereotactic Radiotherapy (VALOR), NCT02984761; JoLT-Ca Sublobar Resection versus Stereotactic Ablative Radiotherapy (SABR) for Lung Cancer (STABLE-MATES), NCT02468024; Radical Resection vs. Ablative Stereotactic Radiotherapy in Patients with Operable Stage I NSCLC (POSTILV), NCT01753414; and SABR versus surgery for stage I NSCLC (SABRTooth) (19). Data from these trials will be useful for making multidisciplinary decisions and for obtaining proper informed consent from early stage NSCLC patients who are fit enough to undergo lung cancer surgery. Therefore, for collecting reliable evidence, increased mutual understanding and strong collaboration is essential between thoracic surgeons and radiation oncologists.
Conclusions
SBRT is not contradicted in operable patients with early-stage NSCLCs, even from the viewpoint of evidence-based medicine. SBRT can be applied in clinical practice based on the patient’s choice. SBRT should be examined in clinical trials as well as through meta-analyses and propensity-matched studies.
Acknowledgments
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Videtic GMM, Donington J, Giuliani M, et al. Stereotactic body radiation therapy for early-stage non-small cell lung cancer: Executive Summary of an ASTRO Evidence-Based Guideline. Pract Radiat Oncol 2017;7:295-301. [Crossref] [PubMed]
- National Comprehensive Cancer Network. Non-small cell lung cancer. Clinical practice guidelines in oncology. Available online: National Comprehensive Cancer Network Inc. Available online: https://www.nccn.org/
- Chang JY, Senan S, Paul MA, et al. Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Oncol 2015;16:630-7. [Crossref] [PubMed]
- Cao C, Wang D, Chung C, et al. A systematic review and meta-analysis of stereotactic body radiation therapy versus surgery for patients with non-small cell lung cancer. J Thorac Cardiovasc Surg 2019;157:362-73.e.
- Zheng X, Schipper M, Kidwell K, et al. Survival outcome after stereotactic body radiation therapy and surgery for stage I non-small cell lung cancer: a meta-analysis. Int J Radiat Oncol Biol Phys 2014;90:603-11. [Crossref] [PubMed]
- Chen H, Laba JM, Boldt RG, et al. Stereotactic Ablative Radiation Therapy Versus Surgery in Early Lung Cancer: A Meta-analysis of Propensity Score Studies. Int J Radiat Oncol Biol Phys 2018;101:186-94. [Crossref] [PubMed]
- Onishi H, Shirato H, Nagata Y, et al. Stereotactic body radiotherapy (SBRT) for operable stage I non-small-cell lung cancer: can SBRT be comparable to surgery? Int J Radiat Oncol Biol Phys 2011;81:1352-8. [Crossref] [PubMed]
- Nagata Y, Hiraoka M, Shibata T, et al. Prospective Trial of Stereotactic Body Radiation Therapy for Both Operable and Inoperable T1N0M0 Non-Small Cell Lung Cancer: Japan Clinical Oncology Group Study JCOG0403. Int J Radiat Oncol Biol Phys 2015;93:989-96. [Crossref] [PubMed]
- Chang JY, Senan S, Paul MA, et al. Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Oncol 2015;16:630-7. [Crossref] [PubMed]
- Komiyama T, Onishi H, Shioyama Y, et al. Japanese multicenter study of stereotactic body radiotherapy for 661 medically operable patients with stage I non-small cell lung cancer. J Thorac Oncol 2015;10:S210.
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22. [Crossref] [PubMed]
- Navarro-Martín A, Galiana IL, Berenguer Frances MA, et al. Preliminary study of the effect of stereotactic body radiotherapy (SBRT) on the immune system in lung cancer Patients unfit for surgery: Immunophenotyping analysis. Int J Mol Sci 2018;19. [Crossref] [PubMed]
- Timmerman R, McGarry R, Yiannoutsos C, et al. Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. J Clin Oncol 2006;24:4833-9. [Crossref] [PubMed]
- Verma V, Rusthoven CG. The fundamental problem of confounding by medical operability in retrospective comparisons of surgery versus stereotactic body radiation therapy for early-stage lung cancer. J Thorac Dis 2018;10:S2176-80. [Crossref] [PubMed]
- Verstegen NE, Lagerwaard FJ, Haasbeek CJ, et al. Outcomes of stereotactic ablative radiotherapy following a clinical diagnosis of stage I NSCLC: comparison with a contemporaneous cohort with pathologically proven disease. Radiother Oncol 2011;101:250-4. [Crossref] [PubMed]
- Lee HY, Lee KS. Ground-glass opacity nodules: histopathology, imaging evaluation, and clinical implications. J Thorac Imaging. 2011;26:106-18. [Crossref] [PubMed]
- Louie AV, van Werkhoven E, Chen H, et al. Patient reported outcomes following stereotactic ablative radiotherapy or surgery for stage IA non-small-cell lung cancer: Results from the ROSEL multicenter randomized trial. Radiother Oncol 2015;117:44-8. [Crossref] [PubMed]
- Haque W, Szeja S, Tann A, et al. Changes in Treatment Patterns and Overall Survival in Patients With Early-Stage Non-Small Cell Lung Cancer in the United States After the Incorporation of Stereotactic Ablative Radiation Therapy: A Population-based Analysis. Am J Clin Oncol 2018;41:259-66. [PubMed]
- Snee MP, McParland L, Collinson F, et al. The SABRTooth feasibility trial protocol: a study to determine the feasibility and acceptability of conducting a phase III randomised controlled trial comparing stereotactic ablative radiotherapy (SABR) with surgery in patients with peripheral stage I non-small cell lung cancer (NSCLC) considered to be at higher risk of complications from surgical resection. Pilot Feasibility Stud 2016;2:5. [Crossref] [PubMed]


