Changing trends in aortic valve procedures over the past ten years—from mechanical prosthesis via stented bioprosthesis to TAVI procedures—analysis of 50,846 aortic valve cases based on a Polish National Cardiac Surgery Database
Introduction
Aortic valve (AV) pathology is the most common type of heart disease in industrialized countries. In contrast to other common types of heart disease, including coronary artery disease (CAD), heart failure or hypertension, conservative medical therapy is insufficient, and progressive disease often requires interventions (1).
The prevalence of AV pathology increases with aging and in recent years the number of AV procedures have also increased (2). However, older age is associated with a higher frequency of comorbidity with increased risks associated with interventions (1). Surgical aortic valve replacement (AVR) is still the gold standard for treatment of AV pathology, however transcatheter aortic valve implantation (TAVI) offers a new treatment option for patients considered high risk for surgery (3).
Therefore, with the worldwide growth in AV procedures, herein we present changes in 10-year observations for AV pathology intervention/treatment trends, regarding patient characteristics, AV pathology, type of procedure, type of implanted prosthesis, technical issues and outcomes based on 50,846 cases from a multicentre Poland registry.
Aim
The aim of the study was to assess and characterize changes in trends in AVR in Poland in the last ten years.
Methods
The study population consisted of 50,846 consecutive adult patients (over the age of 18 years) who underwent AVR between January 2006 and August 2016 in all cardiac surgery units in Poland. The analysis consisted of all AV procedures, including isolated AV surgery, combination procedures and patients who had a prior valve operation. Operative mortality was defined as death within 30 days after the procedure.
The authors had full access to the data, take responsibility for its integrity, and have read and agree to the manuscript as written.
This study will only collect retrospective data information that has been recorded in Polish National Cardiac Surgery Database that is obligatory in Poland. The Polish Society of Cardiothoracic Surgeons approved the research project. All the data has been anonymized. Because of the size of the research group and approval from the Polish Society of Cardiothoracic Surgeons, no patients informed contest was needed.
Study databases
Data for this study was collected retrospectively based on the standardised form of the Polish National Database of Cardiac Surgery Procedures (KROK).
The data collected included age, gender, body mass index (BMI), ejection fraction (EF), previous percutaneous coronary intervention (PCI), Canadian Cardiovascular Society (CCS) class, New York Heart Association (NYHA) class, smoking status, diabetes mellitus (DM), arterial hypertension, hypercholesterolaemia, asthma, chronic obstructive pulmonary disease (COPD).
On the basis of the form of the National Database of Cardiac Surgery (KROK), a computer database was built for further statistical analysis.
Missing data
We excluded patients if records for outcomes (i.e., mortality/survivors) were missing. The completeness of each record was counted: records were only analysed where the percentage of complete data was higher than 90%. Records that were lower than 90% were excluded from analysis. Almost all the data collected was more than 90% complete.
Statistical analysis
Descriptive statistics were performed, and all data were expressed as mean ± standard deviation. Continuous variables were checked for normal distribution with the Shapiro-Wilk test. To assess the differences between two continuous variables, Student’s t-test (for normally distributed values), or the Mann-Whitney U-test (for non-normally distributed values) were applied. Statistical analysis was performed with STATISTICA 10.0 (StatSoft, Tulsa, OK, USA). A two-sided P value <0.05 was considered statistically significant.
Results
Patient characteristics
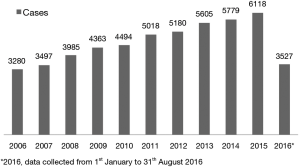
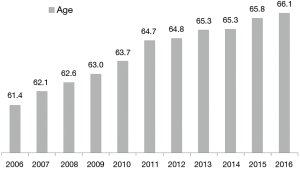
Among 247,364 consecutive adult patients who underwent cardiac surgery procedures during the study period, 50,846 underwent an AV procedure (20.6%). Each year, the number of procedures increased significantly from 3,280 cases performed in 2006 to 6,118 cases performed in 2015 (Figure 1). Patients’ mean age increased significantly during 10 years of observation, from 61.4 years in 2006 to 66.1 years in 2016 (P<0.001) (Figure 2). Detailed patient characteristics are presented in Table 1.

Full table
AV pathology
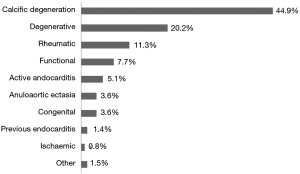
Aortic stenosis was observed in 73.4% of cases (99% data complete), and aortic insufficiency in 80.3% of cases, in whom trivial stenosis was observed in 19.7%, mild stenosis in 22.4%, moderate stenosis in 22.3% and severe stenosis in 15.8% of cases (98% data complete). The most common AV pathology was calcific degeneration observed in 44.9% of cases. Other types of valve pathology are presented in Figure 3.
Procedure
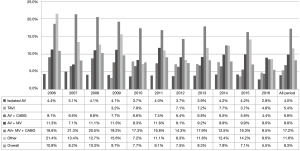
The most common procedure was isolate surgical AVR in 61.2% patients, followed by AVR + coronary artery bypass grafting (CABG) in 23.9% of patients, AVR + mitral valve replacement (MVR) in 7% of patients and TAVI in 2.3% of patients. Detailed data are presented in Figure 4.
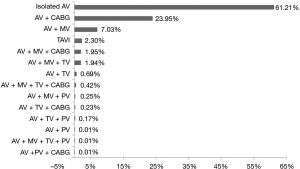
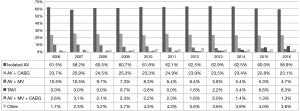
There were significant changes in the type of procedures performed each year (P<0.001). The highest increase was observed in the TAVI procedure, from 0% in 2006 to 8.3% in 2016. The highest decrease was observed in AVR + MVR, from 10.5% in 2006 to 4.7% in 2016. Detailed data of all procedures, including all other procedures performed during this time are presented in Figure 5. Elective procedures were performed in 78.2% cases and 4.39% procedures were reoperations.
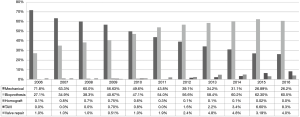
Type of prosthesis
From 2006 to 2016, AVR was performed in 94.8% of cases, TAVI in 2.3%, AV repair in 1.5%, homografts in 0.3% and others in 1.1% of cases. The proportion of prosthetic valves changed from 71.8% mechanical prosthesis vs. 27.1% biological prosthesis in 2006 to 26.4% mechanical prosthesis vs. 60.8% biological prosthesis in 2016. The TAVI procedure had a rapid growth in last four years, from 1.2% in 2012 to 8.8% in 2016. These results were statistically significant (P<0.001) (Figure 6).
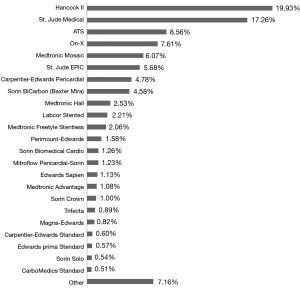
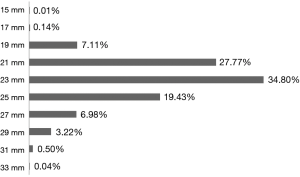
During the 10-year observation, the most commonly used prosthesis was the Hancock II bioprosthesis implanted in 19.9% of patients. The second most common was the Saint Jude Mechanical prosthesis and the third most common was the ATS Medical mechanical prosthesis. All other mechanical and biological prostheses used during this study are presented in Figure 7. The most common size of implanted prosthesis was 23 mm (34.8%), followed by 21 mm (27.77%) and 25 mm (19.43%). All other valve sizes used between 2006–2016 are presented in Figure 8.
Hospitalization
Mean time on ICU was 3.25 days, and mean hospitalization time was 13.04 days. Detailed procedure characteristics and hospitalization data are presented in Table 2. In-hospital mortality significantly decreased (P=0.034) from 10.9% in 2006 to 8.3% in 2016.
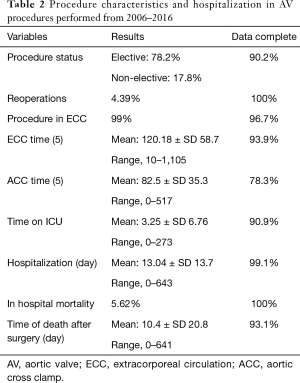
Full table
Throughout the observation period, in-hospital mortality was: 4.0% in isolated surgical AVR, 5.4% in TAVI, 6.8% in AVR + CABG, 9.8% in AVR + MVR, 17.2% in AVR + MVR + CABG, and 11.6% in other procedures (Figure 9).
Discussion
We present contemporary real-life trends in AV procedures over the last ten years in Poland, one of the biggest countries of central Europe, where every year more than 27,000 procedures are performed in 37 centres (6).
Currently, surgical AV procedures are the second most commonly performed cardiac surgery procedures and the number of procedures are likely to increase over time (6,7). Over the course of the study period, more than 20% of procedures (50,846 cases) in Poland were AV procedures. The absolute number of patients undergoing AV procedures in each year increased significantly from 3,280 cases performed in 2006 to 6,118 cases performed in 2015. Similar trends are also observed all over the world (7).
AV disease is the most common acquired valvular disease in elderly patients (8). Currently in Poland, the expected life expectancy of the population of 60 years old is 19 years for men and 21 years for women. In the aging population, it is reasonable to expect that the number of patients seeking treatment for AV disease will also increase in the coming years (2). In our observations, the mean patient age increased significantly from 61.4 years in 2006 to 66.1 years in 2016. However, Polish patients seems to be younger than American patients undergoing these procedures during a similar time period (7). With the aging of patients, there is also an increased risk of coexisting disease. In our study, in the last ten years, the most common comorbidities was hypertension (70.3%), hyperlipidaemia (43.3%) and DM type 2 (23.4%), diseases that are significant risk factors for heart disease and postoperative complications (2,7-11).
Aortic stenosis was observed in 73.4% of cases. The mean transaortic gradient was 80.72 mmHg and was twice as high as the current mean gradient eligible for surgery (1). Severe aortic insufficiency was observed in 15.8% of cases. It should be noted that the mean EF was 52.7%, therefore we may assume that most of the patients undergoing operations had good left ventricular hemodynamic function. Unfortunately, in our database, there was no information on the prevalence of mixed AV disease, and therefore information on the reason for the AV procedure is incomplete.
Intraoperative examination showed the most common AV pathology was valve calcification present in 44.9% of patients and degenerative dysfunction in 20.2% of patients. The prevalence of congenital AV disease was 3.6% and was nearly twice as high as figures described in the literature (12,13). The higher prevalence of bicuspid valves in our study is due to the fact that we present intraoperative examinations, while other studies present mostly results of echocardiography examinations, underestimating case of bicuspid valves (14).
Isolated surgical AVR was performed in 61.2% of cases, and the remainder were combined procedures: CABG + AVR was performed in 23.95% of cases and AVR + MVR was performed in 7.1% of cases. TAVI was only performed in 2.3% of cases. Overall, the number of TAVI procedures may seem low during a 10-year observation period, however the TAVI procedure was first performed in Poland in 2008 (15), six years after first TAVI implantation in the world. From 2008, the TAVI procedure has rapidly grown in popularity from <0.01% cases in 2008 to 8.3% in 2016. In contrast to the TAVI growing trend, the 10-year period saw a 1.6% decrease in the number of isolated surgical AVR from 60.5% in 2008 to 58.9% in 2016. This figure likely represents a stable trend, indicating that the number of indications for the TAVI procedure is increasing. It should be highlighted, that in Poland, for economic reasons, TAVI procedure are reserved only for high risk patients. However, based on the rapidly increase in the rate of TAVI procedures must nowadays in Poland must be treated not as an alternative option for surgical AVR, but as an equal treatment option in high risk patients. In the future, the use of TAVI may overtake that of surgical AVR as the frequency of implanted biological valves is increasing, while mechanical valve implantation is decreasing. However in Poland, surgical AVR still remains the standard treatment options for moderate and low risk patients. This is in contrast with current ESC/EACTS guidelines for AV disease treatment (16). Techniques modification and continuous development of TAVI prosthesis and the publication of several randomized trials, comparing surgical and TAVI treatments, not only in elderly high-risk patients, but also in intermediate and low risk patients (16-18). The results of The PARTNER 3 (19) and EVOLUT (20) were superior or comparable following surgical AVR among patients with severe aortic stenosis at low surgical risk.
The current study presents a changing proportion of mechanical vs. bioprosthetic valves from 71.8% vs. 27.1% in 2006 to 26.4% vs. 60.8% in 2016, respectively. An increased rate of bioprosthetic valve implantation has been observed in the last decade (4,7,21). However, other databases present higher percentages of implanted procedures in each year. Brown and colleagues (4) reported a 78.4% rate of bioprosthetic valve implantation in 2006, Dunning and colleagues (21) 78% in 2009 and Thourani and colleagues (7) 83.8% in 2010. Compared to the present study, the percentage of implanted mechanical valves in Poland is still very high. However, the cited studies present results only for isolate AVR, not in all AV procedures as is the case in the present study. Therefore, from our clinical observations, the overall percentage of implanted bioprosthetic valves in surgical AVR should be higher. The guidelines of the American College of Cardiology and the American Heart Association state that despite a slight advantage of mechanical valves, the increase in bioprosthetic valve implantation is likely due to an older patient population undergoing surgical AVR, perceived improvements in valve durability, and a desire to avoid short-term and long-term anticoagulation, if possible (7,22-24).
Our study shows that in current cardiosurgical practice the role of homografts is marginal, constituting 0.8% of cases. Homografts were implanted more commonly in previous years, likely due to acceptable long term results (25). However, homograft implantation technique is difficult and current bioprosthetic valves have similar outcomes (26). Preservation of the native valve, rather than mechanical valve use may be advantageous, allowing the avoidance of anticoagulation and fewer complications of the operated valve (5,11,23).
From near fifty thousand AV prostheses implanted in the last ten years in Poland, the most common implanted prosthesis was the Hancock II (bioprosthesis), and the second most common was the St. Jude Mechanical Valve (mechanical prosthesis). Our study shows that in Poland, where there are more than 38 cardiac surgery centres, the prosthesis market is huge with a lot of different therapeutic valve options available (23,24,27-30). However, the current study did not examine the effect of valve type on operative outcomes.
Our study also showed that small aortic prostheses, size 15–19 mm, were implanted only in 7.25% of cases. According to the study, this group is a high risk of postoperative PPM (31). The most common implanted prostheses were medium-sized (21–25 mm) implanted in 85% of cases. Although the current study did not examine the effect of prosthesis size and prevalence of postoperative PPM.
In the last ten years, in-hospital mortality significantly decreased for all AV procedures. Importantly, in-hospital mortality reductions were observed even in older patients’ groups. Advances in pre- and post-operative care have led to the possibility that an increasing number of elderly patients can be operated on safely and with a satisfactory outcome (9,32). In isolated surgical AVR, mean in-hospital mortality was 4.0% and was higher than results from American or British databases (7,21). The mean in-hospital mortality in the TAVI group was 5.4%. However, these results are not comparable due to the differences in patient populations included in the studies. In surgical AVR patients, the mean patient age was lower compared to patients undergoing TAVI and the mean Euroscore should be much lower.
Study limitations
This study has several limitations. The most important limitation is the lack of Euroscore or STS results. In the last ten years, the Euroscore was replaced by the Euroscore II. Additionally, in Poland different centres replaced the Euroscore at different times. Therefore, Euroscore results in our database are not comparable and were not analysed to avoid misleading the reader. Additionally, in our database there too many instances of absence of any Euroscore data. Secondly, in some cases medical data were incomplete. However, the size of the sample (n=50,846) suggests that a few instances of incomplete data would not have a statistically significant effect on the outcomes. Thirdly, this study has all of the limitations associated with the collection of data from 37 centres.
Conclusions
- This study demonstrates a 46% increase in the number of patients undergoing all types of AV procedure in Poland over a 10-year period. The most common procedure was isolated surgical AVR, performed in 61.2% of cases.
- From 2008, the TAVI procedure rapidly grew in popularity to 8.3% in 2016.
- The mean patient age increased significantly as well as the number of cases performed every year.
- The most common valve pathology was valve calcification; congenital valve dysfunction was only diagnosed in 3.7% of patients.
- In last ten years, there was significant increase in the use of bioprosthesis.
- In last ten years, in-hospital mortality significantly decreased for all AV procedures from 10.9% in 2006 to 8.3% in 2016.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The Polish Society of Cardiothoracic Surgeons approved the research project (No. 002,10.11.2018). All the data has been anonymized. Because of the size of the research group and approval from the Polish Society of Cardiothoracic Surgeons, no patients informed contest was needed.
References
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC)., European Association for Cardio-Thoracic Surgery (EACTS)., Vahanian A, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33:2451-96. [Crossref] [PubMed]
- Faggiano P, Antonini-Canterin F, Baldessin F, et al. Epidemiology and cardiovascular risk factors of aortic stenosis. Cardiovasc Ultrasound 2006;4:27. [Crossref] [PubMed]
- Villablanca PA, Mathew V, Thourani VH, et al. A meta-analysis and meta-regression of long-term outcomes of transcatheter versus surgical aortic valve replacement for severe aortic stenosis. Int J Cardiol 2016;225:234-43. [Crossref] [PubMed]
- Brown JM, O'Brien SM, Wu C, et al. Isolated aortic valve replacement in North America comprising 108,687 patients in 10 years: changes in risks, valve types, and outcomes in the Society of Thoracic Surgeons National Database. J Thorac Cardiovasc Surg 2009;137:82-90. [Crossref] [PubMed]
- Al-Atassi T, Hynes M, Sohmer B, et al. Aortic root geometry in bicuspid aortic insufficiency versus stenosis: implications for valve repair. Eur J Cardiothorac Surg 2015;47:e151-4. [Crossref] [PubMed]
- Maruszewski B. Main cardiac surgery procedures performer in Poland in 2014 (according to the National Registry of Cardiac Surgery Procedures—KROK, Warsaw, Poland 2015). Kardiochir Torakochir Pol 2015;12:288-91.
- Thourani VH, Suri RM, Gunter RL, et al. Contemporary real-world outcomes of surgical aortic valve replacement in 141,905 low-risk, intermediate-risk, and high-risk patients. Ann Thorac Surg 2015;99:55-61. [Crossref] [PubMed]
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation 2011;123:e18-209. [Crossref] [PubMed]
- Litwinowicz R, Bartus K, Drwila R, et al. In-hospital mortality in cardiac surgery patients after readmission to the intensive care unit: a single-center experience with 10,992 patients. J Cardiothorac Vasc Anesth 2015;29:570-5. [Crossref] [PubMed]
- Litwinowicz R, Bryndza M, Chrapusta A, et al. Hyperbaric oxygen therapy as additional treatment in deep sternal wound infections - a single center's experience. Kardiochir Torakochirurgia Pol 2016;13:198-202. [Crossref] [PubMed]
- Aicher D, Schafers HJ. Aortic valve repair--current status, indications, and outcomes. Semin Thorac Cardiovasc Surg 2012;24:195-201. [Crossref] [PubMed]
- Tadros TM, Klein MD, Shapira OM. Ascending aortic dilatation associated with bicuspid aortic valve: pathophysiology, molecular biology, and clinical implications. Circulation 2009;119:880-90. [Crossref] [PubMed]
- Lewin MB, Otto CM. The bicuspid aortic valve: adverse outcomes from infancy to old age. Circulation 2005;111:832-4. [Crossref] [PubMed]
- Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Eur J Echocardiogr 2009;10:1-25. [Crossref] [PubMed]
- Zembala M, Wilczek K, Przybylski R, et al. POL-TAVI First--Polish report on transcatheter aortic valve implantation (TAVI) of Edwards-Sapien prosthesis in the first 19 high risk patients with severe aortic stenosis and comorbidities. Kardiol Pol 2009;67:936-40. [PubMed]
- Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. Rev Esp Cardiol (Engl Ed) 2018;71:110. [Crossref] [PubMed]
- Aroney C. TAVI or Not TAVI-in Low Risk Patients? That Is the Question. Heart Lung Circ 2017;26:749-52. [Crossref] [PubMed]
- Bagienski M, Kleczynski P, Dziewierz A, et al. Early- and mid-term outcomes after transcatheter aortic valve implantation. Data from a single-center registry. Postepy Kardiol Interwencyjnej 2016;12:122-7. [Crossref] [PubMed]
- Mack MJ, Leon MB, Thourani VH, et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med 2019;380:1695-705. [Crossref] [PubMed]
- Popma JJ, Deeb GM, Yakubov SJ, et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med 2019;380:1706-15. [Crossref] [PubMed]
- Dunning J, Gao H, Chambers J, et al. Aortic valve surgery: marked increases in volume and significant decreases in mechanical valve use--an analysis of 41,227 patients over 5 years from the Society for Cardiothoracic Surgery in Great Britain and Ireland National database. J Thorac Cardiovasc Surg 2011;142:776-82.e3. [Crossref] [PubMed]
- Bonow RO, Carabello BA, Chatterjee K, et al. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2008;118:e523-661. [PubMed]
- Bartuś K, Litwinowicz R, Kuśmierczyk M, et al. Primary safety and effectiveness feasibility study after surgical aortic valve replacement with a new generation bioprosthesis: one-year outcomes. Kardiol Pol 2018;76:618-24. [PubMed]
- Filip G, Litwinowicz R, Kapelak B, et al. Patient-prosthesis mismatch after minimally invasive aortic valve replacement. Kardiol Pol 2018;76:908-10. [Crossref] [PubMed]
- Sadowski J, Kapelak B, Bartus K, et al. Reoperation after fresh homograft replacement: 23 years' experience with 655 patients. Eur J Cardiothorac Surg 2003;23:996-1000; discussion 1000-1. [Crossref] [PubMed]
- Melina G, De Robertis F, Gaer JA, et al. Mid-term pattern of survival, hemodynamic performance and rate of complications after medtronic freestyle versus homograft full aortic root replacement: results from a prospective randomized trial. J Heart Valve Dis 2004;13:972-5; discussion 975-6. [PubMed]
- Martens S, Sadowski J, Eckstein FS, et al. Clinical experience with the ATS 3f Enable® Sutureless Bioprosthesis. Eur J Cardiothorac Surg 2011;40:749-55. [PubMed]
- Englberger L, Carrel TP, Doss M, et al. Clinical performance of a sutureless aortic bioprosthesis: five-year results of the 3f Enable long-term follow-up study. J Thorac Cardiovasc Surg 2014;148:1681-7. [Crossref] [PubMed]
- Breitenbach I, Wimmer-Greinecker G, Bockeria LA, et al. Sutureless aortic valve replacement with the Trilogy Aortic Valve System: multicenter experience. J Thorac Cardiovasc Surg 2010;140:878-84, 884.e1.
- Bartuś K, Litwinowicz R, Kuśmierczyk M, et al. Primary safety and effectiveness feasibility study after surgical aortic valve replacement with a new generation bioprosthesis: one-year outcomes. Kardiol Pol 2018;76:618-24. [PubMed]
- Filip G, Bartuś K, Litwinowicz R, et al. Cardiac surgery Early clinical outcomes of the surgical treatment of patients with aortic stenosis and small aortic annuli. Kardiochir Torakochirurgia Pol 2013;10:199-203. [Crossref]
- Nicolini F, Agostinelli A, Vezzani A, et al. The evolution of cardiovascular surgery in elderly patient: a review of current options and outcomes. Biomed Res Int 2014;2014:736298. [Crossref] [PubMed]