
Delayed traumatic diaphragmatic rupture: diagnosis and surgical treatment
Introduction
A traumatic diaphragmatic rupture is a rare, but severe disease that results from blunt or penetrating trauma to the abdomen and chest. With delayed treatment, the abdominal organs can move through the new opening into the thoracic cavity, resulting in respiratory compromise and ischemia to the affected abdominal organs. A delayed traumatic diaphragmatic rupture is usually found months or years after the trauma and may be misdiagnosed due to its nonspecific clinical features and radiological findings (1). We analyzed the clinical presentations, surgical management, and outcomes of 40 patients diagnosed with a delayed traumatic diaphragmatic rupture in the Peking Union Medical College Hospital and reviewed our experiences with the diagnosis and treatment of these patients.
Methods
We reviewed 40 patients from the Peking Union Medical College Hospital who were diagnosed with a delayed traumatic diaphragmatic rupture and underwent surgery between January 2000 and December 2018. The clinical information from the hospital records was retrospectively reviewed. All patients underwent a routine examination which included routine blood tests, electrolyte measuring, coagulation profile, chest X-ray, and a chest-abdominal computed tomography (CT). Once the diagnosis of diaphragmatic rupture was confirmed, the patients received a thoracotomy depending on the site of injury and the imaging features.
Results
Patient features
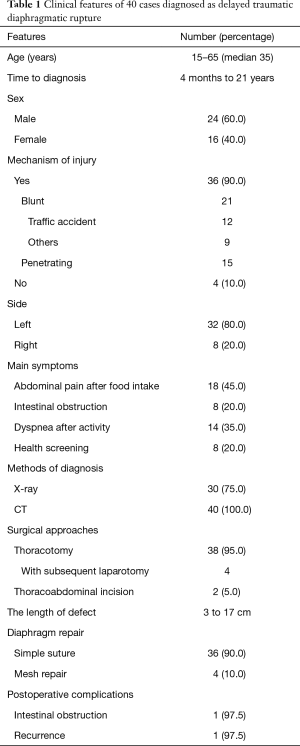
Forty patients were enrolled in this study. There were 24 males and 16 females, with a median age of 35 years (range, 15–65 years). Thirty-six patients complained of injuries, and the symptoms from the patients begun 4 months to 21 years after the primary injury. Blunt injuries were the cause in 21 patients, including 12 road traffic accidents. Fifteen patients had a penetrating trauma. Thirty-two patients had herniation on the left side of the diaphragm, while 8 had herniation on the right side. Most patients claimed that they received an X-ray and CT examination, but there were no signs of a diaphragmatic rupture. The patients who suffered blunt trauma and had no hydropneumothorax according to examination, received a conservative treatment and recovered. For penetrating injuries, such as knife stabbing, or combined with hydropneumothorax, chest drainage was used. Thirty-two patients presented with similar symptoms, including abdominal pain after food intake (n=18), dyspnea after activity (n=14), and intestinal obstruction (n=8) (Table 1).
Full table
Diagnosis and treatment
All of the patients received an X-ray and chest-abdominal CT examination. Thirty patients showed diaphragmatic elevation or hydropneumothorax upon X-ray detection. Herniation of the abdominal organs into the pleural cavity was found in all 40 patients through CT. Furthermore, 24 patients had segmental diaphragmatic defects that were identified through a 3-dimensional construction CT scan.
One patient was operated on as an emergency case, while 39 cases underwent an elective surgical intervention. Thirty-eight patients underwent a thoracotomy, including 4 cases which required a subsequent laparotomy, and 2 who underwent a thoracoabdominal incision operation. The locations of the diaphragm rupture varied with each other, mostly at the costophrenic angle and centrum tendineum. The length of the defect ranged from 3 to 17 cm. The surgical treatment included a hernia reduction, pleural drainage, and the repair of the diaphragmatic defect. The diaphragmatic defects were closed directly in 36 patients and a polypropylene mesh was used in 4 patients.
Postoperative complications and follow-up
All of the patients recovered after surgery. One patient suffered acute intestinal obstruction and received a laparotomy 19 days after the first operation. We found fibrous adhesions in the gastric antrum, and an emergent enterodialysis was performed. The mean length of the postoperative hospital stay was 11 days (range, 5–26 days). One patient experienced a hernia recurrence 2 years later. She received a thoracotomy, which identified a diaphragm defect at the previous site. We repaired the defect with a polypropylene mesh to decrease the tension. She was discharged 7 days after surgery.
Discussion
A traumatic diaphragmatic rupture is extremely rare, with an incidence rate of less than 1%, secondary to trauma (2). It is reported that up to 66% of patients present with a missed diaphragmatic rupture due to the difficulty involved in diagnosing traumatic diaphragmatic injuries. Delayed presentation is the single most important contributor to increased mortality, which can be as high as 30% (3). Various hypotheses can explain the delayed diaphragmatic rupture. Traumatic diaphragmatic rupture is rare and is frequently misdiagnosed as a nonspecific clinical manifestation. It is reported that 19% of diaphragmatic ruptures were missed during the initial laparotomy. The diaphragmatic defect may be detected only when a herniation occurs. Delayed rupture of a devitalized or infected diaphragmatic muscle may occur several days after the initial injury. Therefore, a high clinical index of suspicion is needed to diagnose and manage the diaphragmatic rupture, even with a remote history of high-velocity injury, especially in those who present with severe trauma, such as a multiple rib fracture, lacerations of the liver and spleen, or a history of penetrating injury.
A delayed diaphragmatic rupture may present with obstructive symptoms due to having incarcerated organs and diaphragmatic defects; also, it is likely the patient will experience chest pain, upper abdominal pain, breathlessness, and vomiting (4). These symptoms are nonspecific, meaning that the diagnosis is often delayed or missed. Therefore, a detailed patient history and careful physical examination are necessary for a proper diagnosis. Auxiliary examination plays a vital role in the diagnosis of a delayed diaphragmatic rupture. A chest radiograph and upper gastrointestinal radiography are the preferred methods for the initial diagnosis of a diaphragmatic rupture. However, the sensitivity for detecting a suspected diaphragmatic rupture in a simple chest radiograph examination is only about 25% to 50% (5). CT signs of a diaphragmatic rupture include segmental diaphragmatic defects, dangling diaphragm, herniation through a defect, collar sign and other symptoms. The diagnostic performance improves with the use of the helical CT with 3-D reconstruction (sensitivity, 82–87%; specificity, 72–99%) due to of the higher quality of the axial images (6). In our study, the sensitivity of chest radiography was 75%, and all of the patients were diagnosed by CT scan, with a sensitivity of 100% in the diagnosis of a delayed diaphragm rupture. Helical CT with 3-D reconstruction may also help us to find any diaphragmatic defects, which is essential for a differential diagnosis with diaphragmatic eventration. The subphrenic viscera is still below the diaphragm with no defect. Thus, a spiral CT scan is the most critical examination in the diagnosis and differential diagnosis of diaphragmatic rupture or hernia.
Surgical management is the most successful and effective treatment for a delayed diaphragmatic rupture. The surgical treatment includes reducing any herniated viscera, repairing the diaphragm and restoring the circulation, respiration and digestive functions. Surgical approaches, such as thoracotomy, laparotomy, and thoracotomy with laparotomy, are often used for the treatment of a diaphragmatic rupture. Laparotomy is usually used due to the complete exploration of the abdominal viscera, though it is easier to reduce the herniated tissues and repair the diaphragm via thoracotomy when there are no abdominal injuries (7). Thus, for a delayed diaphragmatic rupture, we tend to choose a thoracotomy as the first surgical approach. We believe that most patients with delayed diaphragmatic ruptures have no acute rupture and injury of the abdominal viscera; therefore, there is little purpose in conducting laparotomy. More importantly, the separation of adhesions and the repair may be safer and more productive by thoracotomy due to the heavier adhesions between the herniated viscera, the diaphragm, and the lung tissues. Thoracoscopy and laparoscopy are also used in a few cases, but more research is needed using a minimally invasive approach. The repair of the hernial defect can be achieved with non-absorbable suturing material as recommended. While simple sutures are sufficient in smaller defects, larger defects need a synthetic mesh to decrease the tension.
Diaphragmatic rupture of the right side is rare; however, once it occurs, the surgical procedure for its correction is challenging (8). In our study, all 32 patients with a left diaphragmatic hernia could be repaired by thoracotomy. However, 4 out of the 8 patients with a right diaphragmatic hernia had difficulty in achieving a reduction through the chest, so hepatobiliary surgeons were called to assist in the treatment with laparotomy. Therefore, for patients with a right diaphragmatic rupture and hernia, a preoperative surgical plan should be made more cautiously, with multidisciplinary preparations.
In our study, 1 patient suffered an acute intestinal obstruction postoperatively and received an emergency laparotomy after the failure of conservative therapy. A fibrous adhesive strip was found around the gastric antrum leading to the obstruction. The possible reasons for this initial failure may be the difficulty involved and the insufficient exploration of the abdominal viscera by thoracotomy. During follow-up, 1 patient experienced recurrence 2 years later. The patient complained of dyspnea, and a chest-abdominal CT examination suggested that the diaphragmatic hernia had recurred. Intraoperative exploration revealed that the abdominal viscera had herniated from the diaphragm defect at a previous site; thus, a polypropylene mesh patch was used to reduce the tension. Therefore, clinicians should be cautious in choosing the method of diaphragm repair. When the defect is significant, a mesh repair is needed to complete a tension-free repair. However, more randomized controlled studies are needed to monitor the recurrence of diaphragmatic hernia.
Delayed diaphragmatic rupture with diaphragmatic hernia is rare and has a mysterious nature. Therefore, it is crucial to investigate the patient’s history carefully. The diagnosis should be made with the consideration of a combination of clinical symptoms and physical signs. Chest and abdominal CT with 3-D reconstruction examination can significantly improve the accuracy of diagnosis. Once the diagnosis is confirmed, surgical treatment should be conducted immediately, and the surgical approach and diaphragm repair methods employed should be carefully evaluated before surgery. If necessary, multidisciplinary cooperation in surgical treatment should be ensured to reduce the mortality rate caused by complications.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from all patients.
References
- Mizobuchi T, Iwai N, Kohno H, et al. Delayed diagnosis of traumatic diaphragmatic rupture. Gen Thorac Cardiovasc Surg 2009;57:430-2. [Crossref] [PubMed]
- Kuo IM, Liao CH, Hsin MC, et al. Blunt diaphragmatic rupture--a rare but challenging entity in thoracoabdominal trauma. Am J Emerg Med 2012;30:919-24. [Crossref] [PubMed]
- Kishore GS, Gupta V, Doley RP, et al. Traumatic diaphragmatic hernia: tertiary centre experience. Hernia 2010;14:159-64. [Crossref] [PubMed]
- Peer SM, Devaraddeppa PM, Buggi S. Traumatic diaphragmatic hernia-our experience. Int J Surg 2009;7:547-9. [Crossref] [PubMed]
- Shanmuganathan K, Killeen K, Mirvis SE, et al. Imaging of diaphragmatic injuries. J Thorac Imaging 2000;15:104-11. [Crossref] [PubMed]
- Desir A, Ghaye B. CT of blunt diaphragmatic rupture. Radiographics 2012;32:477-98. [Crossref] [PubMed]
- Kuy S, Juern J, Weigelt JA. Laparoscopic repair of a traumatic intrapericardial diaphragmatic hernia. JSLS 2014;18:333-7. [Crossref] [PubMed]
- Chughtai T, Ali S, Sharkey P, et al. Update on managing diaphragmatic rupture in blunt trauma: a review of 208 consecutive cases. Can J Surg 2009;52:177-81. [PubMed]


