Emergency operation of a patient with spontaneous rupture and massive hemorrhage of pleural solitary fibrous tumor
Solitary fibrous tumor (SFT) is a rare pleural disease with asymptomatic clinical course. A case of pleural SFT with spontaneous rupture and massive hemorrhage, which was treated by emergency operation, is described.
Case report
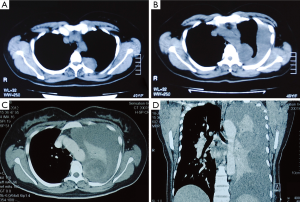
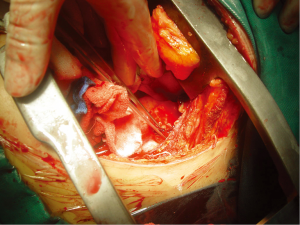
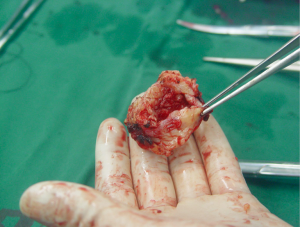
A tumor was found in a 48-year-old woman’s left thorax by routine physical examination. Her medical history was unremarkable without exposure to asbestos. Chest computed tomography (CT) scan showed a mass of 2.8 cm × 2.5 cm near the descending aorta in the left thorax without hydrothorax (Figure 1A). She refused consent for the operation at first. After two months she was sent to the hospital again for sudden dyspnea and chest pain. Chest CT scan showed the mass with the same size and moderate amount of pleural effusion (Figure 1B). Closed thoracic drainage in the left thorax was taken and massive bloody fluid was revealed. Hemoglobin in blood routine test gradually descended from 46 to 43 g/L despite blood transfusion. Enhanced chest CT scan showed large amount of pleural effusion in the left thorax, mediastinum was compressed to the right side, with no sign of aorta rupture or dissection (Figure 1C,D). Left posterolateral thoracotomy through the fifth intercostal spaces was performed immediately for hemostasis and resection of the tumor. About 2,500 mL blood was sucked in the left thorax. The left lung was normal. The tumor was found originated from the parietal pleura, the diameter was 3 cm, top of the it was ruptured and bleeding. We completely resected the tumor and the parietal pleura on the chest wall between the fourth and fifth ribs near the descending aorta (Figures 2,3). The tumor was not connected with the visceral pleura and lung. Hemoglobin rosed to 106 g/L by blood transfusion after surgery.
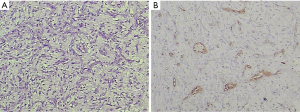
Histopathologically, spindle-shaped cells with demarcated nuclear membranes and dispersed chromatin in vesicular nuclei were observed. Mitoses were rare. Immunohistochemical staining showed that the tumor was expressing vimentin, CD34, CD31, and Bcl-2, cytokeratin was negative (Figure 4A,B). The tumor was pathologically diagnosed as benign localized pleural SFT. The patient discharged eight days after the operation. She is currently healthy after surgery.
Discussion
Solitary fibrous pleural tumor is a rare form of pleural disease. SFT represents less than 5% of pleural tumors and occurs most often in the visceral (80%) and parietal pleura (20%). It is considered to be originated from the mesenchymal cells of the sub-mesothelial connective tissue of the pleura. According to immunohistochemical analysis, vimentin, CD34, CD99 and Bcl-2 are positive in pleural SFT, which are markers of mesenchymal cells; however, cytokeratin is negative, which is found in mesotheliomas. These results indicate that SFT originates from mesenchymal cells rather than mesothelial cells (1). In our case, immunohistochemical analysis showed vimentin, CD34 and Bcl-2 were positive, which was the identical character of SFT.
SFTs often have an asymptomatic clinical course. The tumor usually grow into a huge mass before local compression symptoms developed, especially in patients without routine physical examinations. Tumors larger than 10 cm would occupy a large space and compress other thoracic structures, which may cause symptoms such as dyspnea, chest pain, cough, and fatigue. About 50% of patients reported in the literature are symptomatic (2). Uncommonly hypertrophic pulmonary osteoarthropathy and hypoglycemia are also caused. Hypertrophic osteoarthropathy, called Pierre Marie-Bamberger syndrome, is associated with the abnormal production of hyaluronic acid by the tumors. Hypoglycemia is caused by the insulin-like growth factor 2, which is secreted by the tumors (3). In our case, the patient had no symptom at first. When the tumor ruptured spontaneously, dyspnea and chest pain appeared until the operation was done to remove the tumor and relieve the compression of hemorrhage in her left thorax. The cause of spontaneous rupture is not clear. The only blood supply may come from vessels in the partial pleura and chest wall. One possible reason is that the top of the tumor tends to necrosis and bleeding because of insufficient blood supply along with growing of the tumor.
Occasional recurrences have been reported not only in malignant cases but also in benign cases, even though it is small percentage (1.4%) (4). Now the patient recovers very well after emergency operation, close follow-up is indicated because of the possibility of recurrence.
Conclusions
We report a case of a patient with spontaneous rupture and massive hemorrhage of pleural SFT. Although the tumor is small and benign, surgical resection could be considered for bleeding could be caused and presented as dyspnea and chest pain.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Harrison-Phipps KM, Nichols FC, Schleck CD, et al. Solitary fibrous tumors of the pleura: results of surgical treatment and long-term prognosis. J Thorac Cardiovasc Surg 2009;138:19-25. [PubMed]
- Guo J, Chu X, Sun YE, et al. Giant solitary fibrous tumor of the pleura: an analysis of five patients. World J Surg 2010;34:2553-7. [PubMed]
- Shaker W, Meatchi T, Dusser D, et al. An unusual presentation of solitary fibrous tumour of the pleura: right atrium and inferior vena cava compression. Eur J Cardiothorac Surg 2002;22:640-2. [PubMed]
- Magdeleinat P, Alifano M, Petino A, et al. Solitary fibrous tumors of the pleura: clinical characteristics, surgical treatment and outcome. Eur J Cardiothorac Surg 2002;21:1087-93. [PubMed]


