
Waste not, want not: diagnostic material found in suction syringe aspirate during endobronchial ultrasound guided transbronchial needle aspiration
Introduction
Lung cancer is the leading cause of mortality among those with cancer, and its diagnosis is of paramount importance (1). Endobronchial ultrasound guided transbronchial needle aspirate (EBUS-TBNA) is a procedure commonly performed with minimal complications and is recommended by major societies as an initial modality for staging patients diagnosed with non-small cell lung cancer (NSCLC) (2-5). It also serves as an acceptable diagnostic tool in patients with sarcoidosis and lymphoma (6,7).
Various technical procedural aspects of EBUS-TBNA have been evaluated with respect to their effect on diagnostic yield. EBUS needle size was addressed by multiple large studies that showed no significant difference in the yield between 21 and 22 gauge needles, however the 21-gauge needle increased the quantity of the yield in addition to preserving the architecture of the cells, which may arguably improve cytogenetic analysis in lung cancer (8-14). Presence versus absence of the needle stylet during the procedure did not alter the outcome in terms of diagnosis or number of lymphocytes or malignant cells (15).
The number of needle passes required for optimization of molecular analysis has not been clearly established, but current recommendations are to acquire additional samples beyond the routine specimens (7). A study by Yarmus et al. in 2013 suggests that four passes with ROSE may be optimal (16). In the era of personalized medicine with targeted therapeutics and immunotherapy it is important to maximize our yield of diagnostic material.
In addition to the aforementioned studies on evaluating the ramifications of specific techniques during the procedure, one study evaluated the diagnostic effect of using a suction syringe and found no statistically significant difference (17). Regardless, EBUS-TBNA is still commonly taught and performed with the application of a suction syringe to the needle during specimen acquisition. On occasion, during the process of agitating the needle within the target lymph node some material (typically hemorrhagic) is inadvertently collected in the suction syringe. It is not clear what the diagnostic value of this suction syringe aspirate is, and therefore there is no standard evidence-based recommendations on how best to handle and/or analyze the specimen.
In some centers this suction syringe aspirate is pooled along with the primary specimens in sequential order, but in others it is wasted. Given the lack of clarity around the diagnostic value of the suction syringe aspirate, and a lack of guidelines in appropriate handling of this material, we decided to pool it throughout our EBUS-TBNA procedures in a separate container and send it for individual analysis.
Methods
This study was an electronic health record (EHR)-based retrospective review. The study was approved by our institutional review board (1171269-2). This retrospective review included EBUS-TBNA cases performed at Creighton University Medical Center between January 2015 and July 2018. All procedures were completed by 4 pulmonologists with or without the assistance of fellows.
EBUS-TBNA was performed on an outpatient basis under deep sedation with the presence of a trained anesthetist. All patients had an artificial airway in place during the procedure in the form of either an endotracheal tube or a laryngeal mask airway, at the discretion of the proceduralist. Routine bronchoscopic airway inspection was completed using an Olympus BF-1T180 prior to using the linear array ultrasonic bronchoscope (Olympus BF-UC180F) to complete a comprehensive mediastinal and hilar lymph node examination. A dedicated 19, 21, or 22-gauge needle was then used in all cases to perform transbronchial needle aspiration on all nodal stations noted to be greater than 10 mm in short axis diameter proceeding in a presumed N3, N2, N1 sequence. The specific needle that was used was determined by the performing pulmonologist based on routine clinical criteria and physician preference.
After initial insertion of the needle into the target node, the stylet was removed and negative pressure was applied with a suction syringe set at −10 cm water pressure. The needle was agitated within the lymph node from 5–10 times. Suction was then closed, the needle was retracted, and the primary specimen was collected in either Cytolyt, saline, formalin, or Roswell Park Memorial Institute medium (RPMI) based on the clinical indication, or was used for slide preparation for rapid on-site cytological evaluation when appropriate.
If any visible material was aspirated into the suction syringe during a needle pass, an aliquot of 2–3 cc of saline was used to flush the material from the suction syringe into a separate Cytolyt specimen container. This process was repeated iteratively throughout the procedure and the final specimen was labeled “pooled suction syringe aspirate” and sent for separate cytological evaluation. No efforts were made to intentionally collect material in the suction syringe beyond routine practice. No intentional trauma was induced to cause bleeding. Therefore, the majority of procedures did not have suction syringe aspirate collected.
Statistical analysis
Continuous variables are presented as median and interquartile range, whereas categorical variables are presented as frequency and percent. Diagnostic yield was defined as any diagnosis. Percent agreement was calculated as the percent in which the pooled aspirate diagnosis agreed with the EBUS diagnosis, presented alongside the Wilson score confidence interval. All statistical analyses were conducted using SAS v. 9.4.
Results
A total of 314 patients underwent EBUS-TBNA under the supervision of 4 pulmonologists at Creighton University Medical Center during the dates of inclusion. Of the 314 patients, 44 (14%) had suction syringe aspirate collected during the procedure and are included in this study. The median age was 68 years (IQR: 46–76 years) and 24 (54.5%) patients were female. The percent agreement of any diagnosis based on the pooled aspirate was 90.9% (95% CI: 78.7–97.2%). The percent agreement was a 100% for lymphocytes, 86.7% for malignancy, and 77.8% for granulomatous inflammation. The percent agreement was 100% for squamous cell carcinoma, small cell lung cancer and for the one case of metastatic cancer. It was 75% for adenocarcinoma. Non-caseating granulomatous inflammation had an agreement of 83.3%, 50.0% for histoplasmosis and 100.0% for necrotizing lymphadenitis. The details of percent agreement between the pooled aspirates and EBUS diagnoses are provided in Table 1.
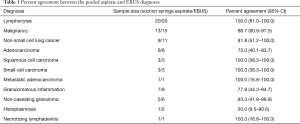
Full table
We encountered a total of six cases where the suction syringe aspirate and the diagnosis were not in agreement. There were only three cases where the pooled aspirate was non-diagnostic, and the final diagnoses in those cases were histoplasmosis, granulomatous inflammation, and adenocarcinoma respectively. Interestingly, in 2 cases (4.5%) patients were diagnosed with granulomatous inflammation based solely on the suction syringe aspirate given that all the routine needle biopsies showed only lymphocytes. In the last case, the suction syringe aspirate revealed only lymphocytes which was discordant with the lymph nodes which were diagnostic for adenocarcinoma. Cases of disagreement between diagnoses obtained from the lymph nodes compared with the pooled aspirates are provided in Table 2.
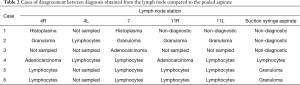
Full table
Discussion
The value of using suction during EBUS-TBNA has been drawn into question, however it is still commonly utilized. In theory, the value of suction is that it increases the amount of diagnostic material collected during EBUS-TBNA, but it has the potential to increase bleeding and theoretically cause a paradoxical decrease in diagnostic yield. A randomized prospective study done in this regard showed no difference in yield, adequacy or diagnosis when using suction (18). According to the guidelines, EBUS-TBNA may be performed with or without suction, with an emphasis on operator expertise and clinical decision making (7). Suction syringe aspirate collected during EBUS-TBNA has previously had unknown diagnostic significance. As such, there are no specific guidelines with respect to the collection and analysis of this material. This study was performed to determine whether this material has potential diagnostic value.
Our retrospective analysis included 44 patients who underwent EBUS-TBNA and had suction syringe aspirate collected during their procedures. We found that the percent agreement of the above-mentioned diagnoses was as high as 90.9 percent based on the suction syringe aspirate. The high rate of concomitant diagnostic material found in the suction syringe aspirate supports the common practice of adding this material to the primary EBUS-TBNA specimens collected iteratively throughout the procedure. However, it was very surprising to note that nearly 5% of our cases had the final diagnosis established solely on the results of the suction syringe aspirate, and these cases would have been non-diagnostic if the suction syringe aspirate had been wasted.
The American Joint Committee on Cancer (AJCC) 8th edition of TNM staging did not change the description of the nodal stations, but the presence of nodal metastasis continues to have significant prognostic implications (19). Hence, given the presence of diagnostic material in the suction syringe one must use the same caution with the suction syringe as they do with the needle when going out of sequence with N1 to N3 stations, given the possibility of upstaging a patient if the syringe were accidentally used out of sequence. If for any reason during an EBUS-TBNA procedure there is a need to sample a higher order nodal station after a lower order nodal station has already been sampled, a new needle and a new suction syringe should be used as to avoid erroneously upstaging the patient.
Apart from the risk of contaminating specimens and inadvertently upstaging patients, the results of our study support the practice of sequentially pooling the suction syringe aspirate with the primary specimens during EBUS-TBNA in order to maximize the amount of diagnostic material which may allow for additional molecular analysis, though this is speculative and requires further research. EBUS-TBNA has been previously shown to provide reasonable diagnostic material for molecular testing for NSCLC (20,21). A study by Rooper et al. along with others demonstrated that most EBUS-TBNA specimens provide adequate sample for subtyping NSCLC and performing cytogenetic analysis. While this should be individualized on a case by case basis, there is usually enough tissue for molecular analysis after completion of Immunohistochemistry (IHC) (22-25). It is logical, however to make every effort to optimize the amount of diagnostic material collected during EBUS-TBNA to assure sufficient substrate for molecular testing, which is why we recommend pooling any suction syringe aspirate with the primary specimen during EBUS-TBNA based on the results of this study.
Our study has several limitations, namely its retrospective nature, small sample size, single-center design, and that we were unable to assess the suction syringe aspirate’s adequacy for molecular analysis. Our sample size was small given that the collection and analysis of the material was performed in the routine care of patients with the standard procedural approach to be as atraumatic as possible. Only a minority of our EBUS cases resulted in collection of a suction syringe aspirate given that no additional efforts were made to intentionally cause trauma in an effort to collect suction syringe aspirate beyond what was inadvertently collected during the routine course of our procedures.
Conclusions
Based on results of this study we recommend that material collected in the suction syringe during EBUS-TBNA be collected, handled and analyzed along with the primary specimens. The suction syringe aspirate contains additional diagnostic material more than 90% of the time, and it may represent the sole diagnostic material in nearly 5% of cases. Likewise, the same degree of care that is taken during procedures that involve more than one needle to avoid inadvertent upstaging by contaminating specimens should also be taken when using more than one suction syringe. Further study is required to confirm these preliminary findings, and to determine if appropriate use of the suction syringe aspirate may increase the likelihood of specimen adequacy for molecular analysis and ancillary testing.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors have agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by our institutional review board (1171269-2).
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin 2016;66:7-30. [Crossref] [PubMed]
- Kayawake H, Chen-Yoshikawa TF, Oda H, et al. Complications of endobronchial ultrasound-guided transbronchial needle aspiration. Ann Thorac Surg 2017;104:e363-5. [Crossref] [PubMed]
- Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: diagnosis and management of lung cancer: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e211S-50S. [Crossref] [PubMed]
- Detterbeck FC, Lewis SZ, Diekemper R, et al. Executive summary: diagnosis and management of lung cancer: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:7S-37S. [Crossref] [PubMed]
- Vilmann P, Frost Clementsen P, Colella S, et al. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2015;48:1-15. [Crossref] [PubMed]
- Agarwal R, Srinivasan A, Aggarwal AN, et al. Efficacy and safety of convex probe EBUS-TBNA in sarcoidosis: a systematic review and meta-analysis. Respir Med 2012;106:883-92. [Crossref] [PubMed]
- Wahidi MM, Herth F, Yasufuku K, et al. Technical aspects of endobronchial ultrasound-guided transbronchial needle aspiration: CHEST guideline and expert panel report. Chest 2016;149:816-35. [Crossref] [PubMed]
- Oki M, Saka H, Kitagawa C, et al. Randomized study of 21-gauge versus 22-gauge endobronchial ultrasound-guided transbronchial needle aspiration needles for sampling histology specimens. J Bronchology Interv Pulmonol 2011;18:306-10. [Crossref] [PubMed]
- Nakajima T, Yasufuku K, Takahashi R, et al. Comparison of 21-gauge and 22-gauge aspiration needle during endobronchial ultrasound-guided transbronchial needle aspiration. Respirology 2011;16:90-4. [Crossref] [PubMed]
- Yarmus LB, Akulian J, Lechtzin N, et al. Comparison of 21-gauge and 22-gauge aspiration needle in endobronchial ultrasound-guided transbronchial needle aspiration: results of the American College of Chest Physicians Quality Improvement Registry, Education, and Evaluation Registry. Chest 2013;143:1036-43. [Crossref] [PubMed]
- Giri S, Pathak R, Yarlagadda V, et al. Meta-analysis of 21-versus 22-G aspiration needle during endobronchial ultrasound-guided transbronchial needle aspiration. J Bronchology Interv Pulmonol 2015;22:107-13. [Crossref] [PubMed]
- Rotolo N, Cattoni M, Crosta G, et al. Comparison of multiple techniques for endobronchial ultrasound-transbronchial needle aspiration specimen preparation in a single institution experience. J Thorac Dis 2017;9:S381-5. [Crossref] [PubMed]
- Jeyabalan A, Shelley-Fraser G, Medford AR. Impact of needle gauge on characterization of endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) histology samples. Respirology 2014;19:735-9. [Crossref] [PubMed]
- Saji J, Kurimoto N, Morita K, et al. Comparison of 21-gauge and 22-gauge needles for endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. J Bronchology Interv Pulmonol 2011;18:239-46. [Crossref] [PubMed]
- Scholten EL, Semaan R, Illei P, et al. Stylet use does not improve diagnostic outcomes in endobronchial ultrasonographic transbronchial needle aspiration: a randomized clinical trial. Chest 2017;151:636-42. [Crossref] [PubMed]
- Yarmus L, Akulian J, Gilbert C, et al. Optimizing endobronchial ultrasound for molecular analysis. How many passes are needed? Ann Am Thorac Soc 2013;10:636-43. [Crossref] [PubMed]
- Harris K, Maroun R, Attwood K, et al. Comparison of cytologic accuracy of endobronchial ultrasound transbronchial needle aspiration using needle suction versus no suction. Endosc Ultrasound 2015;4:115-9. [Crossref] [PubMed]
- Casal RF, Staerkel GA, Ost D, et al. Randomized clinical trial of endobronchial ultrasound needle biopsy with and without aspiration. Chest 2012;142:568-73. [Crossref] [PubMed]
- Rami-Porta R, Asamura H, Travis WD, et al. Lung cancer—major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 2017;67:138-55.
- Folch E, Yamaguchi N, VanderLaan PA, et al. Adequacy of lymph node transbronchial needle aspirates using convex probe endobronchial ultrasound for multiple tumor genotyping techniques in non–small-cell lung cancer. J Thorac Oncol 2013;8:1438-44. [Crossref] [PubMed]
- Raad S, Bendaly E, Nuguru S, et al. Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration Use for the Subclassification and Genotyping of Non-small Cell Lung Cancer. Chest 2016;150:707A. [Crossref]
- Garcia-Olivé I, Monsó E, Andreo F, et al. Endobronchial ultrasound-guided transbronchial needle aspiration for identifying EGFR mutations. Eur Respir J 2010;35:391-5. [Crossref] [PubMed]
- Rooper LM, Nikolskaia O, Carter J, et al. A single EBUS-TBNA procedure can support a large panel of immunohistochemical stains, specific diagnostic subtyping, and multiple gene analyses in the majority of non–small cell lung cancer cases. Hum Pathol 2016;51:139-45. [Crossref] [PubMed]
- Nakajima T, Yasufuku K, Nakagawara A, et al. Multigene mutation analysis of metastatic lymph nodes in non-small cell lung cancer diagnosed by endobronchial ultrasound-guided transbronchial needle aspiration. Chest 2011;140:1319-24. [Crossref] [PubMed]
- van Eijk R, Licht J, Schrumpf M, et al. Rapid KRAS, EGFR, BRAF and PIK3CA mutation analysis of fine needle aspirates from non-small-cell lung cancer using allele-specific qPCR. PLoS One 2011;6:e17791. [Crossref] [PubMed]


