
Letter to the Editor
Novel air leak test and step-by-step strategy for preventing the air leak in lung surgery
Receiving sincere comments from experts in the field on technology that shows new direction and possibility can be a great foundation for further development. Three (1-3) editorials expressed their curiosities and concerns for our study (4) as follows.
- Will Yang’s bubble solution (YBS) be also successful in securing vision in real human thorax? Of course, some degree of visual disturbance due to lung inflation is inevitable. However, it is believed that vision disturbance can be easily and safely solved by pressing the lung with an appropriate lung retractor (Figure 1) and dividing the inspected area into lobes with spraying the solution partially and sequentially. Again, the biggest problem in conventional water submersion test (WST) is that the water itself which fills the chest cavity blinds the view and raises the threshold of air bubbles through the water pressure.
- Can the air leak inspection work well even on the irregular lung surface or large tear site such as interlobar or intersegmental surface? YBS is a slightly viscous but fairly fluidic substance. Therefore, the solution can be easily sprayed in any type of lung surface and form the bubble if there is an air leak. The reason why we designed the experiment with needle lung injury was to simulate small air leakage because a large amount of air leak would be easier to locate.
- How does the remaining bubble solution affect the fibrin glue substance? We also wonder about that part. However, it is expected that the remaining solution will be washed away due to the hydrophilic property of Pluronic® F-127 (PF127) if simple water irrigation is used. The hemostasis material, such as fibrin glue may be used without any adverse effects. In addition to the safety issue for the human body, experiments will be needed to see whether the adhesion of fibrin glue will be weakened or not when the solution is resprayed on the fibrin clot area.
- How long does it take to test the whole lung? Water irrigation is usually necessary to remove blood before the WST after pulmonary lobectomy to avoid the blood-red water. The process of filling the warm distilled water is repeated until the confirmation of no air leak. However, if you use the YBS, you can start it immediately, and you can save time by water irrigation only once at the end because you can check it with a small volume of solution.
- Changes in the state of the solution according to the temperature: YBS should be stored in a refrigerator for maintaining the fluidic status. In-vivo animal experiments are indispensable to understand how the solution changes in the environment within the thorax with a body temperature of 36.5-Celsius degree. That will be our next step.
- Cost-effectiveness of YBS compared to WST: the manufacturing cost for YBS will indeed be more expensive than sterile distilled water. However, PF127 and indocyanine green have been used usefully in the pharmaceutical industry without the issue of cost. Furthermore, if the YBS test can reduce the air leak duration days after lung surgery, it will be a more significant benefit in the end in terms of hospitalization and quality of life.
- What is the best strategy for air leakage? That is another debate, but if there is a pinpoint air leak, we use fibrin glue or TachoComb® (CSL Behring, Tokyo, Japan). If there is a laceration or denuded lung, it is repaired with absorbable (Polydioxanone, PDS®II 4-0, Ethicon, Somerville, NJ, USA) double layered continuous suture. If the suture could be imperfect due to the surrounding hilar structure, we have combined free pericardial fat pad coverage with imperfect suture (5) (Figure 2).
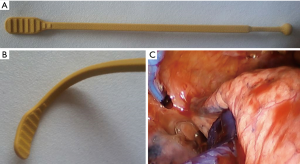
Figure 1 Dr. Yang’s invention for lung or esophageal retraction. (A,B) Custom-made flexible silicone reusable retractor for VATS (Korean patent number 10-1549973). (C) Safe and secure lung compression by our flexible lung retractor in VATS. VATS, video-assisted thoracic surgery.
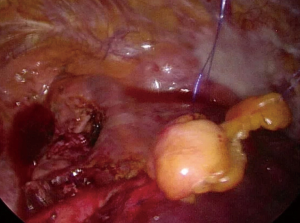
Figure 2 Free, not pedicled, pericardial fat pad reinforcement for air leak control in the interlobar fissure area after left upper lobectomy.
In conclusion, for reducing the incidence of the prolonged air leak in VATS lung surgery, air leak detection method must be done correctly and accurately.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Kawai H. Problems with using the air leak test with Yang’s bubble solution during video-assisted thoracic surgery. J Thorac Dis 2019;11:630-1. [Crossref] [PubMed]
- Kaaki S, Pysyk C, Gilbert S. Will bubbling decrease the muddling?-a promising technique to detect air leak intra-operatively. J Thorac Dis 2019;11:S1206-7. [Crossref] [PubMed]
- Eberlein M, Baldes N, Bölükbas S. A novel air leak test using surfactant: a step forward or a bubble that will burst?. J Thorac Dis 2019;11:S1119-22. [Crossref] [PubMed]
- Yang HC, Chang HY. Novel air leak test using surfactant for lung surgery. J Thorac Dis 2018;10:6472-4. [Crossref] [PubMed]
- Matsumoto I, Ohta Y, Tsunezuka Y, et al. Free pericardial fat pads can act as sealant for preventing alveolar air leaks. Ann Thorac Surg 2005;80:2321-4. [Crossref] [PubMed]
Cite this article as: Yang HC, Chang HY. Novel air leak test and step-by-step strategy for preventing the air leak in lung surgery. J Thorac Dis 2019;11(8):E106-E108. doi: 10.21037/jtd.2019.08.68


