Evolving from conventional video-assisted thoracoscopic lobectomy to uniportal: the story behind the evolution
Diego Gonzalez-Rivas personal experience: how the idea of uniportal VATS lobectomy was born
“Humans are allergic to change. They love to say, we’ve always done it this way. I try to fight that. That’s why I have a clock on my wall that runs counter-clockwise.”
—Grace Hopper
When I started my training in thoracic surgery in 1999, I realized that the post-operative period for patients were very painful and hard because the incision we used to operate was very large, about 15 cm with rib spreading. So very often I thought of ways on how to improve this post operational period of our sick patients. In short, what could we do to reduce this pain and facilitate a better quality of life?
“There is always a way to do it better, so find it.”
—Thomas Edison
So I started to study the origins of thoracoscopic surgery and this approach started to fascinate me. In the year 1910, Jacobaeus, described the first thoracoscopy to release adherences in patients suffering from tuberculosis. Before him, Kelling had done this in 1901 in dogs but not in humans. He did not publish this though and therefore Jacobaeus is claimed to be the first surgeon to use thoracoscopy in 1910. For many years this procedure was relegated to diagnostics and therapeutic procedures up till 1992 when Giancarlo Roviaro decides to do the first lung resection to surgically treat lung cancer through small incisions, looking at a screen and no rib spreading. He went from an aggressive open surgery to a minimally invasive surgery by using only three small incisions enabling the patient to a better postoperative recovery. This revolutionized the world of thoracic surgery. He was criticized for many years by the more traditional surgeons who considered themselves more prestigious than him by claiming that this procedure was not a total oncological procedure.
Time proved him right. Giancarlo Roviaro believed in his idea that the post-operative period of his patients could be improved by doing surgery with small incisions. His experience doing surgery through small incisions showed him this was not only possible but that his patients had much less pain and faster recovery after surgery.
The medical community did not see it this way and many years had to go by before he was recognized for his work. This is the story of medicine and in general of mankind.
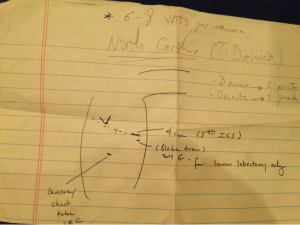
I decided I had to learn this technique so I searched which hospital in the world had the most video surgery experience. So, in 2007 I went to Los Angeles in the United States and learned the surgical technique through 3-4 incisions with one of the most expert surgeons of the world (Dr. Robert Mckenna) and I put to it practice at my hospital. When we gathered enough experience I decided I had to improve my technique further, so I went back again to New York. By chance, I met a person there who changed my way of thinking. I had gone to New York to improve my three incisions technique and this person told me they were doing two incisions at Duke University Medical Center in North Carolina. This thought really confused me as I couldn’t understand how surgery could be done through two incisions only. In my head I had the concept that three incisions were necessary: utility incision for instrumentation, inferior port for the camera and posterior incision for holding the lung. I wasn’t able to think differently so I asked this person to draw it on a piece of paper (Figure 1).
After I returned to Spain this piece of paper kept me thinking and rethinking about how this could be done. I couldn’t understand it. I decided then to go to Duke. I contacted the chief surgeon at Duke and he answered that he didn’t accept people whom he did not know so you can imagine my disappointment. I couldn’t accept a “no” for an answer so I persisted. I had to meet him. I decided to go to a congress that he would attend so I could meet him in person. I attended the annual meeting of the American Thoracic Society to meet Dr. Damico, and after an unforgettable conversation I asked him about the possibility to visit his institution and then I was accepted. Thanks to persistence Dr. D’Amico and I are very good friends and we organize courses together. Thanks to the persistence of an idea. If I wouldn’t have believed in this I would’ve never met him and I wouldn’t be where I am nowadays.
So it is important to never stop thinking and to never let your ideas go if you believe they are important.
However, thinking differently has produced a lot of troubles to those who came up with new ideas or innovations. A clear example of this was Galileo—Galileo during his time dared to say that the world was round and as a consequence was sentenced to be arrested for a long time at home. In order escape from this punishment he had to reject his idea and say all was a lie.
Another example of innovation and ideas, this time in relation to medicine, was Semmelweis. This person discovered asepsis. He tried to convince his colleagues that if people washed their hands their patients would have less post-operative infections. He was expelled from the international scientific community and finally died from an infection (after cutting himself during an autopsy).
Obviously, people who think differently, who are visionaries are the ones who change the world. The founder of Apple, Steve Jobs was a visionary and he became a genius. He pronounced these words:
“Here’s to the crazy ones, the misfits, the rebels, the troublemakers, the round pegs in the square holes the ones who see things differently—they’re not fond of rules. You can quote them, disagree with them, glorify or vilify them, but the only thing you can’t do is ignore them because they change things, they push the human race forward, and while some may see them as the crazy ones, we see genius, because the ones who are crazy enough to think that they can change the world, are the ones who do”.
But think differently especially in the medical world can be very risky because we are affecting the most valuable asset human beings have, health. I knew though, that I had to think differently because I was a restless person and I liked to innovate.
During the double port technique I was working most of the time with the camera located through the utility incision because I realized that I had a better direct view. So I thought: for lower lobes, all instruments and staplers are inserted through the utility incision but the view came from another perspective, not anatomic. Why not have the same view as we have during an open thoracotomy approach? Thus, in June 2010 after thinking a lot I decided to do the first lobe resection through one single port. I placed all instrumentation and the camera through the same utility incision. I realized during the surgery that I felt comfortable, with a better view and was able to finish it completely very fast. The evolution of the patient was excellent, discharged on the second postoperative day with no pain. This motivated me to continue further with this approach. When I first published it in an international journal the conclusion I drew was that this surgery was only meant for tumors in the lower lobes. For the upper lobes I thought we needed new technology to access them due to angulation a physical problem. Nothing further from reality. In time, with the evolution I realized that if we thought differently and we exposed the lung in a different way, no new technology was needed. Thus, all surgery could be done, and so we did. We published all our cases and results in the most important journals and textbook of thoracic surgery. Thanks to team work, we could teach our technique to our colleagues and residents who were starting.
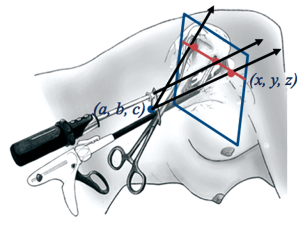
In 2012, in an international congress, an Italian surgeon called Luca Bertolaccini with a background in physics and fascinated by our technique made a physical and mathematical demonstration with equations of why our uniportal technique (through one incision) was better than other techniques which were being used by some of the best surgeons in the world. The advantage of using the camera in coordination with the instruments is that the vision is directed to the target tissue, bringing the instruments to address the target lesion from a straight perspective, thus we can obtain similar angle of view as for open surgery (Figure 2). Conventional three port triangulation makes a forward motion of video-assisted thoracic surgery (VATS) camera to the vanishing point. This triangulation creates a new optical plane with genesis of dihedral or torsional angle that is not favorable with standard two-dimension monitors. Instruments inserted parallel to the videothoracoscope also mimic inside the chest maneuvers performed during open surgery. This mathematic explanation made me understand many things, such as why I felt so comfortable that first time, why were we able to teach the technique and reproduce it successfully in other parts of the world.
We were invited to many different countries to give conferences: China, Taiwan, Korea, Rusia, Israel, Indonesia, Brazil, Chile, Colombia, Turkey, United States, France, Italy, Germany. What first started as a curiosity, a special ability of one surgeon—I heard this thousands of times—in time it became a reproducible technique which all members of my department performed. This created even more interest. The uniportal technique was adopted in other parts of the world and we received even more demand. It’s not because the technique was interesting for being a unique thing, but it’s being applied all over the world and its expansion continues.
During all this time we’ve had many obstacles. It hasn’t been a walk through the park. Because when you’re doing a new technique, you need to design many new things in your head. You need to learn how to expose the lung properly, you need to search for strategies, how to teach these and not only that—the obstacles posed by people, surgeons of prestige who see themselves threatened by this novel technique because they are unable to learn it. Then critics and envies happen opposition takes place.
Because every innovation comes with restriction. Therefore, these obstacles made us grow and all critics from other colleagues we heard predicting the future such as: you’re not going to reach anywhere; this technique doesn’t have any future ended in nothing.
Life is full of erroneous predictions—In 1913 the president of the Michigan bank advised Henry Ford’s lawyer not to invest in Ford Motor Company arguing that the horse was here to stay and the automobile was just a fad. Luckily this person didn’t listen to the advice. He invested and became a multimillionaire.
We’ve always followed the philosophy of never be intimidated by the obstacles and be always open to progress. Because we never know what the future will bring. The next generation will be with the robotic technology, single port devices, wireless cameras. We are sure of this because the future will be the minimum invasiveness. This is why we believed in our idea. Who knows if in the future we will have devices of robotic surgery at home? What we can’t do is close ourselves to evolution and make predictions on things that won’t work.
I’ve learned that in life if you walk alone, you will get there faster but if you walk in company you will get further. And without the support of the people who love you and a good team, we would’ve never been able to reach where we are now. Who would’ve told us that from a small corner of Spain, with the several colleagues against our innovation, after a lot of work, dedication and confidence we would do something that was going to bring revolution to surgery in the world.
This is why the key is to think differently, measure risks, be innovative, believe in an idea, fight for it and overcome obstacles, because “Impossible is nothing”.
“Intelligence is the ability to adapt to change.”
—Stephen Hawking
Coruña University and Minimally Invasive Thoracic Surgery Unit (UCTMI) experience: a coordinated teamwork
We started to perform VATS lobectomies in our department in 2007 after learning the technique at Cedars Sinai, LA (1). After performing over 80 lobectomies with three ports, we eliminated the posterior incision, and subsequently performed most lobectomies through only two ports according to the technique described by D’Amico (2). But the final step of the surgical evolution in our unit, to minimize chest wall trauma, was the uniportal approach for major lung resections.
We developed the technique to perform major pulmonary resections by uniportal approach in June 2010 (3) thanks to the previous experience in double-port VATS for lobectomy and single-port technique for minor procedures (wedge resections, pneumothorax, etc). Initially only lower lobes cases were selected.
This evolution in the approach from three ports to single port technique required a new learning curve: different lung exposure and learning how to coordinate the instruments and the camera with no interference during surgery. As with all new surgical procedures, there was a certain learning curve component but not comparable to the one experienced when starting a VATS program (4).
For double port VATS lower lobectomies all the instrumentation and stapler insertion are performed through the utility incision. Therefore we decided to insert the optic through the utility incision working in coordination with instruments to perform a single incision lobectomy. The first case we performed was accomplished in 90 minutes and the patient was discharged on the second postoperative day with no complications (3). When several lower lobes cases were performed with good results, the upper lobes were attempted (5). With gained experience the more complex resections were accomplished (6) (Figure 3).

Results (4 years’ experience)
- June 2010-April 2014: 362 uniportal lobectomies (>900 total uniportal VATS);
- 2.4% conversion rate;
- Most frequent resection: RUL;
- Mean surgical time: 150.62 [40-310] min;
- Mean number of lymph nodes: 14.8 [5-38];
- Mean nodal stations: 4.7 [3-8];
- Median chest tube: 2 days;
- Median hospital stay: 3 days;
- Complications: 69 patients.
Tips and tricks: the uniportal approach can be adopted following two different ways
- Learning from conventional VATS to uniportal (our evolution)
- Remove the posterior port;
- Adopt the double port technique;
- For lower lobectomies place the camera at the posterior part of utility incision;
- Use bimanual instrumentation with curved instruments;
- For upper lobectomies place the camera through utility incision and use inferior port only for stapler insertion or for instrumentation;
- Use the inferior port only to expose the lung (camera, staplers and instrumentation through the incision);
- Remove the inferior port;
- Use vascular clips when no angle for staplers;
- Always insert the staplers with angulation for vascular division;
- Start with lower lobectomies (female and thin patients preferably).
- Learning from open approach to uniportal (uniportal mimics the open maneuvers)
- Adopt the Anterior small thoracotomy approach (10-12 cm incision);
- Add the thoracoscope to thoracotomy (use monitor view and open direct view during surgery);
- Remove rib spreader (same incision). Move instruments and camera along the 10 cm incision;
- Reduce progressively the size of incision after gained experience.
Future
The future of the thoracic surgery is to reduce the surgical and anesthetic trauma. We truly believe on the use of the single port technique for major pulmonary resections because we understand that the future goes in that direction, i.e., robotics and single-port. We expect further development of new technologies like sealing devices for all vessels and fissure, robotic arms that open inside the thorax and wireless cameras, which will probably allow the uniportal approach to become the standard surgical procedure for major pulmonary resections in most thoracic departments. The combination of nonintubated or awake thoracoscopic surgery and single-port VATS technique is promising because it represents the least invasive procedure for pulmonary resections (8). Thanks to avoidance of intubation, mechanical ventilation and muscle relaxants the anesthetic side effects are minimal allowing to most of the patients to be included in a fast protocol avoiding the stay in an intensive care unit.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1, 100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Video-Conference during international symposium on uniportal VATS held in Coruña. Asvide 2014;1:304. Available online: http://www.asvide.com/articles/317
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014. [Epub ahead of print]. [PubMed]