The challenging management of lung choriocarcinoma
Introduction
As part of the group of pregnancy related tumors, choriocarcinoma (CCA) is a trophoblastic neoplasm arising from placenta with secondary haematogenous spread into lungs, brain, liver, kidneys, intestine, pelvis and vagina. It is characterized by a fast course with reasonably satisfactory prognosis. Symptoms can vary from cough, shortness of breath and haemoptysis to menorrhagia, gastrointestinal bleed and devastating neurological deterioration depending on the site of invasion of the metastatic disease. It is associated with notable and sometimes soaring levels of serum b-HCG. In addition to chemotherapy, surgical intervention would sometimes be indicated especially in sizeable distant lesions resistant to chemotherapy.
Case report
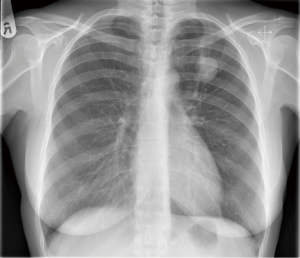
A 42-year-old female school teacher presented to our department with recent onset of cough, shortness of breath on physical exertion and haemoptysis. She had a smoking history of ten cigarettes per day for the last 15 years and a recent pregnancy giving birth to a healthy girl 6 months prior to onset of symptoms. Sputum sample was positive for blood but negative for growth of microorganisms. CXR demonstrated an isolated left upper lobe lung lesion (Figure 1), confirmed on subsequent CT scan of the chest. A PET CT image revealed mild metabolic activity within the lung lesion (Figure 2). A CT guided biopsy of the lesion was inconclusive and the patient underwent a left thoracotomy with lingula sparing upper lobectomy and systematic lymph node dissection. The postoperative course was complicated by chylothorax that was treated conservatively with octreotide and a low fat diet. Histology report was extremely interesting demonstrating largely ischemic, ill-defined necrotic tumor with variable cellular component ranging from giant, irregular and symplastic cells with multiple hyperchromatic nuclei to the other, smaller and rounder cells with clear cytoplasm, well defined borders, central hyperchromatic nuclei and abundant atypical mitosis. The above represented syncytia and cytotrophoblastic cells, respectively and were strongly suggestive of the diagnosis of metastatic CCA possibly arising from a primary gestational endometrial carcinoma especially on the background of the recent pregnancy. Raised serum BHCG levels (3,200 UI/L) further confirmed the diagnosis. Further investigation from the gynaecology team including transvaginal ultrasound was negative for a lower abdominal or pelvic mass. At this point, she developed the loss of peripheral vision and the subsequent MRI scan of the brain showed 2 mm lesion in the brain. The neurosurgical opinion was sought that concluded no surgical intervention due to a very small lesion and the patient was commenced on the combined chemotherapy (low dose etoposide and cisplatin initially and EMA/CO on week 2). Patient underwent three courses of chemotherapy treatment with duration of 6 weeks resulting in a complete resolution of the physical symptoms and normalization of the BHCG serum levels. A repeat PET CT scan was negative and she was discharged home with a 6-month follow-up outpatient appointment and 2 weekly BHCG level monitoring by the GP in the community.
Discussion
Gestational trophoblastic diseases (GTD), as a broad term encompassing both benign and malignant growths arising from products of conception in the uterus, may be classified as hidatidiform moles (HM) which contain complete and partial HM and gestational trophoblastic neoplasia comprising invasive mole, CCA, placental site trophoblastic tumor (PSTT) and epithelioid trophoblastic tumor (ETT) (1,2). The reported incidence of GTD varies widely worldwide, from a low of 23 per 100,000 pregnancies (Paraguay) to a high of 1,299 per 100,000 pregnancies (Indonesia) (2). However, at least part of this variability is caused by differences in diagnostic criteria and reporting. The reported incidence in the United States is about 110 to 120 per 100,000 pregnancies. Some textbooks speculate more generalized idea that in Europe and North America the incidence of CCA is higher ranging from 1 in 40,000 pregnancies to 9.3 in 40,000 in South East Asia and Japan (3).
Variety of the risk factors have been implicated by different studies ranging from smoking, exogenous hormones and low body mass to associations between different maternal and paternal blood groups, genetic and environmental factors. However, on reviewing the modern literature, the most commonly described predisposing factors seem to be pregnancy, previous abortions or ectopic pregnancies with the biggest of them all being previous molar pregnancy and an early or late maternal age (2). Nevertheless, early identification of the high risk groups and decision for giving prophylactic chemotherapy remains a challenge as there is no clear cut indication for testing individuals extensively without presence of significant symptoms.
Immunohistochemical markers can further confirm the diagnosis of CCA with tumors staining strongly for HCG and inhibin alpha in the trophoblast, human placental lactogen (HPL) and inhibin alpha in intermediate trophoblast, and cytokeratin in all trophoblast cells (4). Approximately 75% of the CCA demonstrate distant body metastasis on diagnosis most commonly to lungs and brain.
The most commonly referred classifying and staging tool for GTD appears to be the WHO modifying scoring system adapted by FIGO anatomical staging (Tables 1,2) (5).
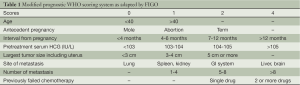
Full table
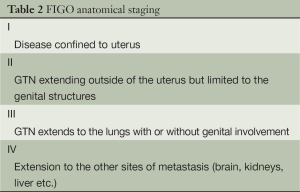
Full table
In our example, modified WHO score was 14, FIGO stage IV putting the patient in an exceptionally high risk. Ordinarily, in similar circumstances, treatment with polychemotherapy must be commenced with an immediate effect. There are no randomized trials comparing regimens in common use to establish superiority of one chemotherapeutic agent over another. Therefore, literature does not permit firm conclusions about the best therapeutic regimen (6). EMA/CO (etoposide, methotrexate and dactinomycin/cyclophosphamide and vincristine) is the most commonly used regimens (7,8). Concomitantly, vigorous serum BHCG level control must follow and close observation for potential symptoms to ensure initially falling, and then normal levels of HCG and possible need for surgical intervention in the event of debilitating recurrent metastatic disease resistant to chemotherapy.
All in all, it can be concluded that, all women post pregnancy and especially with the presence of significant risk factors (i.e., previous abortions, ectopic pregnancy, molar pregnancy, age more than 35) presenting with hemoptysis must be carefully worked up for CCA, or at the least it should be one of the main differential diagnosis.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Ngan HY, Kohorn EI, Cole LA, et al. Trophoblastic disease. Int J Gynaecol Obstet 2012;119:S130-6. [PubMed]
- Altieri A, Franceschi S, Ferlay J, et al. Epidemiology and aetiology of gestational trophoblastic diseases. Lancet Oncol 2003;4:670-8. [PubMed]
- Principles and practice of gynecologic oncology. In: Barakat RR, Berchuck A, Markman M, et al. eds. 6th Edition. Epidemiology of gynecologic cancers. Demographic patterns. Host Factors. Chapter 1:21.
- Principles and practice of gynecologic oncology. In: Barakat RR, Berchuck A, Markman M, et al. eds. 6th Edition. Gestational trophoblastic disease: Molar pregnancy. Chapter 27:889-92.
- FIGO Committee on Gynecologic Oncology. Current FIGO staging for cancer of the vagina, fallopian tube, ovary, and gestational trophoblastic neoplasia. Int J Gynaecol Obstet 2009;105:3-4. [PubMed]
- Deng L, Yan X, Zhang J, et al. Combination chemotherapy for high-risk gestational trophoblastic tumour. Cochrane Database Syst Rev 2009;CD005196. [PubMed]
- Bower M, Newlands ES, Holden L, et al. EMA/CO for high-risk gestational trophoblastic tumors: results from a cohort of 272 patients. J Clin Oncol 1997;15:2636-43. [PubMed]
- Lurain JR, Singh DK, Schink JC. Management of metastatic high-risk gestational trophoblastic neoplasia: FIGO stages II-IV: risk factor score > or = 7. J Reprod Med 2010;55:199-207. [PubMed]