Primary mucoepidermoid carcinoma of the thymus presenting with myasthenia gravis
Case presentation
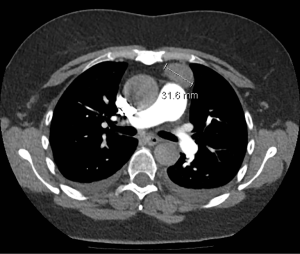
A 47-year-old female was referred for surgical resection of an anterior mediastinal mass which was found incidentally on a computed tomography pulmonary angiogram (CTPA). She presented with worsening shortness of breath and fatigue whilst under investigation for autoimmune hepatitis under the hepatologist. As part of the medical work up, she underwent a CTPA which ruled out a pulmonary embolus, but confirmed the presence of a well-rounded anterior mediastinal mass which was largely homogenous (Figure 1). In view of her ongoing symptoms of fatigue and breathlessness, she was also reviewed by the neurologists and was subsequently diagnosed with myasthenia gravis, confirmed on electromyography (EMG) and blood tests showing elevated titres of acetylcholine receptor antibodies.
She underwent surgical resection of her anterior mediastinal mass via median sternotomy without immediate complication. She had an uneventful recovery and was discharged on the sixth post-operative day.
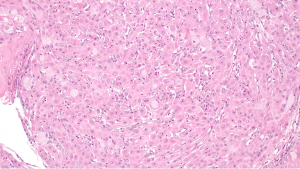
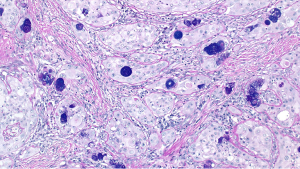
Histological analysis revealed a 31 mm diameter unencapsulated tumor with an infiltrative margin (Figure 2). There was evidence of sheets and trabeculae of bland squamous cells, large polygonal and columnar cells with eosinophilic cytoplasm, round nuclei with vascular chromatin and prominent nucleoli. Nuclear inclusions were present in occasional cells. Histological and immunochemical analysis were consistent with a well-differentiated mucoepidermoid carcinoma (MEC) (Figure 3). Background tissue was mostly atrophic with no evidence of a thymoma.
The patient then underwent magnetic resonance imaging (MRI), which excluded a head and neck primary, confirming a primary MEC of the thymus. She continues to have symptoms of myasthenia gravis which are well controlled with her pre-operative medication. The patient did not require any chemotherapy or radiotherapy post-operatively and remained well after the operation. She has been scheduled for a surveillance CT scan in 9 months.
Discussion
MEC are most commonly found in salivary glands as first described by Stewart et al. in 1945 (1), there has since been reports of these neoplasms arising in other sites including larynx, bronchus and oesophagus. Primary MEC of the thymus is a rare malignant epithelial neoplasm and less than 30 cases have been reported in the literature (2-4). There are no apparent associations with other conditions or paraneoplastic syndromes. There has been only one reported case of combined MEC of the thymus and thymoma with a background of myasthenia gravis (2), that patient’s symptoms of myasthenia gravis resolved completely following resection of his combined thymic carcinoma and thymoma. There has been no reported case of MEC of the thymus alone with concurrent myasthenia gravis. It is uncertain why our patient has myasthenia gravis and if it is related to her thymic malignancy, or if it is purely a coincidence that she had a thymic mass and her myasthenia gravis may be related to other underlying autoimmune processes in view of her ongoing autoimmune hepatitis. In view of the rare nature of this condition, it appears difficult to draw any conclusive evidence at present.
Patients with MEC of the thymus commonly present with respiratory symptoms including exertional dyspnea and chest pain, others remain asymptomatic and are incidentally found to have an anterior mediastinal mass on routine chest radiography. Radiologically, MEC of the thymus are often well-circumscribed, homogenous masses in the anterior mediastinum with multi-locular cystic structures observed on computed tomography (CT) scans of the thorax (3). This can vary depending on tumor grade and there have been cases where local invasion to adjacent structures are observed (4,5). These tumors are characterized histologically by squamoid mucin-producing cells with intermediate type cells. Histological analysis also revealed that these tumors vary from well- to poorly-differentiated. Poorly-differentiated, high grade tumors have greater propensity for local invasion and distant metastasis and often have rapid progression of the disease despite aggressive subsequent treatment with chemotherapy resulting in mortality.
The Masaoka staging system for thymomas is also commonly used for thymic carcinomas. The stages are as follows: stage 1, grossly and microscopically encapsulated mass; stage 2, invasion of mass beyond thymic capsule; stage 3, macroscopic invasion of neighbouring organs; stage 4a, pleural or pericardial dissemination; stage 4b, haematogenous or lymphatic dissemination. This is often useful in determining prognosis as higher stage patients have much poorer 5-year survival rates.
Surgical resection is the mainstay of treatment for low-grade tumors, some requiring radiotherapy to prevent local recurrence or disease progression. In cases where complete surgical resection is not possible, treatment with local radiotherapy appears to have a positive prognosis for low-grade disease as well (6). There is also suggestion in the literature that thymic tumors may be chemosensitive for high grade disease (7). However, as these tumors are fairly uncommon and vary greatly between cases, there is no established treatment regimen that has proven effective beyond anecdotal evidence.
Although extremely rare, MEC of the thymus should be considered in a list of differential diagnosis for anterior mediastinal masses. As it is difficult to achieve a diagnosis based on radiological findings alone, early surgical excision is recommended, not only to achieve histological diagnosis but also to prevent local invasion or further disease progression.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Stewart FW, Foote FW, Becker WF. Muco-Epidermoid Tumors of Salivary Glands. Ann Surg 1945;122:820-44. [PubMed]
- Wu SG, Li Y, Li B, et al. Unusual combined thymic mucoepidermoid carcinoma and thymoma: a case report and review of literature. Diagn Pathol 2014;9:8. [PubMed]
- Yasuda M, Yasukawa T, Ozaki D, et al. Mucoepidermoid carcinoma of the thymus. Jpn J Thorac Cardiovasc Surg 2006;54:23-6. [PubMed]
- Nonaka D, Klimstra D, Rosai J. Thymic mucoepidermoid carcinomas: a clinicopathologic study of 10 cases and review of the literature. Am J Surg Pathol 2004;28:1526-31. [PubMed]
- Kim GD, Kim HW, Oh JT, et al. Mucoepidermoid carcinoma of the thymus: a case report. J Korean Med Sci 2004;19:601-3. [PubMed]
- Stefanou D, Goussia AC, Arkoumani E, et al. Mucoepidermoid carcinoma of the thymus: a case presentation and a literature review. Pathol Res Pract 2004;200:567-73. [PubMed]
- Ogawa K, Toita T, Uno T, et al. Treatment and prognosis of thymic carcinoma: a retrospective analysis of 40 cases. Cancer 2002;94:3115-9. [PubMed]


