
Comparison of blood flow in single and sequential vein grafts during off-pump coronary artery bypass
Introduction
Coronary artery bypass grafting (CABG) surgery is one treatment for coronary artery disease. The results of this procedure depend on the patency of vein grafts. Because of the paradoxical patency of vein grafts in the terminal anastomosis of the sequential grafts (end to side), single or sequential graft procedure in CABG is used by different surgeons (1).
Now transit-time flow measurement (TTFM) is the most commonly used method for intraoperative assessment of graft patency during OPCAB. Several studies have reported grafts blood flows by transit-time flowmetry (2-13), and TTFM also could predict the graft failure in the short (8,9) and medium term (10). Nonetheless, little information is available comparing the surgical results of isolated and sequential grafts (4,11) in posterior descending artery (PDA) in one patient. To assess the performance of sequential saphenous vein grafts, a comparison of mean blood flows (MBF) and pulsatility index (PI) of single versus sequential grafts in the same patient was carried out by TTFM during OPCAB by a single surgeon.
Methods
The study was approved by the Ethics Committee of Beijing Anzhen Hospital (2015027X).
Patients Selection
The inclusion criteria of the study were the patients with isolated OPCABG, exactly 4 anastomoses in left anterior descending (LAD), diagonal artery (DIAG), obtuse marginal artery (OM) and PDA respectively done, the saphenous vein diameter not less than 4mm. From April, 2015 to December 2015, in our team the senior author (GU, CX) performed isolated OPCABG on 250 patients, in which 128 with triple-vessel coronary heart disease were included in this study. There were 96 males (75%) and 32 females. Mean age was 66±8 (range, 54–80) years old. The patients’ clinical data are listed in Table 1. Other patients (n=122) with valve disease (n=21), aortic disease (n=2), congenital heart disease (n=2), not exactly 4 anastomoses (n=80), and bad quality of the saphenous vein (n=17) would be excluded.
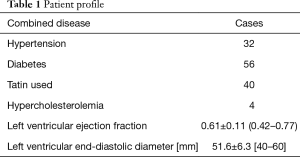
Full table
Surgical technique
The operation was performed through a median sternotomy in all cases. After systemic heparinization (1 mg/kg), the pedicled LIMA and the greater saphenous vein (SVG) were harvested by the skilled cardiac surgeon. Proximal end-to-side anastomosis with 6-0 prolene between the SVG and aorta was done by applying a side-biting clamp to temporarily arrest part of the aorta before coronary artery grafting. An epicardial stabilizer was applied to immobilize the target vessel site for grafting, a bull-dog clamp was used to temporarily arrest coronary artery proximal to arteriotomy. No intracoronary shunt was used after arteriotomy for safeguarding arterial endothelium. Warm saline was used to flush the site to reveal surgical field. The LIMA was always grafted to the LAD end-to-side, the sequential SVG anastomoses were constructed side-by-side in the diagonal branch, obtuse marginal branch and end-to-side in PDA. All LIMA and distal vein anatomoses were sutured with 8-0 prolene (Johnson and Johnson, Shanghai, China).
TTFM technique
With care taken to fit the graft caliber, the size of the probe was chosen as #3 (the inner diameter is 3 mm) and #4 (the inner diameter is 4 mm). In all cases, TTFM was recorded at a systemic systolic pressure of 110±5 mmHg. The flow probe was placed around LIMA or vein graft at 1.5–2.0 cm proximal to the anastomosis of LAD or PDA to measure the graft blood flow data. The bulldog clamp was used to temporarily arrest the graft distal to the anastomosis of DIAG, then put the probe around the graft at 1.5–2.0 cm proximal to the anastomosis to measure the DIAG graft data. In the same way, the graft blood flow data to OM were measured. All data were recorded when they were stable. The TTFM technique was used as described in literature (2-7) (Figure 1).
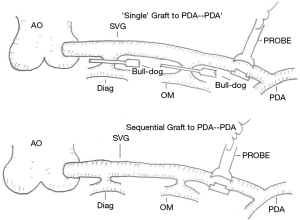
- TTFM of ‘single graft’: Two bull-dog clamps were used to temporarily arrest the anastomoses of diagonal and obtuse marginal branches close to the SVG graft, thus the sequential graft became a ‘single graft’. The MBF rate and PI of grafts to PDA were recorded as MBF-PDA’ and PI-PDA’ in this ‘mimic’ single graft.
- After successfully recording the ‘single graft’ data, the bull-dog clamps were immediately removed, and the ‘single graft’ was restored to the sequential graft. Under the same condition, the MBF and PI of grafts to PDA were recorded as MBF-PDA and PI-PDA (Figure 2).

Follow-up
All patients were followed up in out-patient clinic at 6 months after surgery. All of them underwent coronary artery CTA to evaluate the grafts.
Statistics
Statistical analysis was performed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA). The two groups were compared by using paired 2-trailed test for continuous variables. A P value of less than 0.05 was considered statistically significant.
Results
Clinical outcomes
All the patients recovered uneventfully and were extubated 1 day after surgery. There were no perioperative myocardial infarction and no obviously infection in patients. They were discharged in a week after surgery.
Graft flow rate to PDA
MBF rate of ‘single graft’ and sequential graft directed to PDA are listed in Table 2. There were no significant differences in the mean flow rate between the two groups (P=0.472) (Table 2).
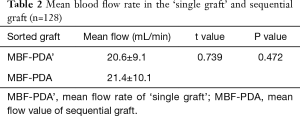
Full table
PI to PDA
PI of ‘singe graft’ and sequential graft directed to PDA are listed in Table 3. There were no significant differences in the PIs between two groups (P=0.941) (Table 3).
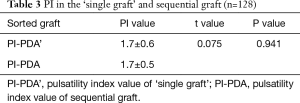
Full table
Other grafts
In all patients, LIMA was used as graft to LAD (end-to-side), and the greater saphenous vein was used in grafts to DIAG and OM (side-by-side). The values of mean flow and PI were listed in Table 4.
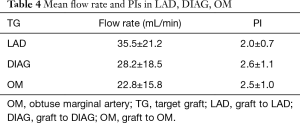
Full table
Follow-up
Coronary artery CTA in all patients at six months after surgery showed that all grafts were patent.
Discussion
Most of clinical studies show that the mid- and long-term results of off-pump CABG are the similar to that of on-pump CABG (14-17). However, debates still remain among cardiac surgeons regarding whether single graft or sequential graft is suitable in OPCAB for patients with multi-branch coronary artery disease. Recently TTFM is widely used clinically. Studies indicate that the data of graft hemodynamics by TTFM could evaluate the quality of anastomoses of graft in surgery, also could predict the short-term and mid-term patency of grafts (8-10). Thus, in this study we used the TTFM in OPCAB to compare the hydrodynamic data of the single and sequential grafts to PDA in the same patient.
In this study, after all anastomoses had been completed, the bull-dogs were used to temporally arrest the anastomoses of SVG graft to the diagonal and OM close to the vein graft, thus the sequential graft became a ‘single graft’ to PDA. TTFM was used to measure the MBF rate and PI in this ‘mimic single’ graft. To rule out the influence of systemic hemodynamics, the heart should be in a stable and remain in the same position when TTFM was used to measure the two grafts. So, once the ‘single graft’ data were recorded, the bull-dogs were removed instantly, the ‘single graft’ was restored to a sequential graft, TTFM was used to measure the MBF rate and PI in sequential graft to PDA.
Our results show that there were no significant differences in the MBF between the ‘single’ and sequential grafts to PDA. The MBF is proportional to the gradient pressure of two ends of the graft, and inversely proportional to the resistance of the target vessel, so the MBF was relative to the inner diameter of the target vessel, blood viscosity and the thickness of blood vessel. The index of MBF could demonstrate the increased rate of blood flow to the myocardium, which is the target that the coronary artery supplies. MBF combined with other index (such as PI) could reflect the quality of the anastomosis. In our study, the MBF rates of a ‘single graft’ were as much as a sequential graft, which approximated 21 mL/min, enough to supply the ischemic myocardium (18). TTFM was introduced clinically to study the graft blood flow rate many years ago. Series studies have shown that the MBF of main sequential graft is greater than that of a single graft (11,12). In sequential graft, the more anastomoses, the greater the MBF rate of proximal main graft. Our research reinforces the previous findings because the MBF rates were alike whether in ‘single graft’ or sequential graft to PDA.
PI is another important index to evaluate the quality of anastomosis. PI is expressed as (blood flowmax − blood flowmin)/MBF. Any imperfect anastomosis, including kinked or twisted or stenotic grafts, could make a raise in PI. In the present study, there was no significant difference in the PI of ‘single’ and sequential grafts to the PDA. In two groups, the average PIs were around 1.7, less than average 5.0 (18), which implies good quality of the anastomoses. There are clinical studies showing that the results of TTFM is a predictor of a graft failure after CABG (8-10). So according to our TTFM results, the short- and mid-term patency of graft to PDA is the same in single grafts as in sequential grafts. In our study the blood flow direction of sequential SVG graft to PDA should be consistent as possible as the direction of PDA blood flow.
Although there is an argument in the mid-term and long-term patency of single or sequential SVG grafts to PDA, more clinical studies support that the mid- and long-term term patency of sequential SVG grafts show the better results (1). In sequential grafts, the surgeons worry about the occlusion in proximal anastomosis, which may result in large myocardial infarction. Actually, the blood flow rate in the proximal graft in sequential SVG is much greater than that in single SVG, which prevents proliferation of the coronary endothelium. A study has shown that proximal occlusion of a sequential graft might result in recurrence of angina, rather than a recurrent myocardial infarction in most clinical instances (19).
Given that OPCAB offers a shorter operative time, less SVG use, shorter hospital stay and only one anastomosis in ascending aorta, sequential SVG graft may be a better option for patients with partly calcified ascending aorta and/or SVG deficiency. Cardiac surgeon can choose a suitable surgical procedure according to their preference, technical proficiency and the condition individual patients.
Study limitations
One limitation of this study is that the length of the ‘mimic single’ SVG graft to the PDA is a little shorter than an actual single SVG graft, because when a single SVG graft is used to PDA, the graft will run along the right side of the heart. From a perspective of hemodynamics, the different length of the two vessels may slightly affect the flow rates and PI of the grafts. Of course, many factors can affect the graft patency. The graft blood flow index is one of these factors.
Conclusions
The results of this study show that in OPCAB there was no difference in the MBF rate and PI of single and sequential SVG grafts to the PDA. In one patient, either single or sequential graft can be selected to PDA. There is no difference in short-term and mid-term graft patency.
Acknowledgments
I would like to express my sincere thanks to Dr. MA, Weiguo who has provided editorial support on the paper.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethics Committee of Beijing Anzhen Hospital (2015027X).
References
- Li J, Liu Y, Zheng J, et al. The patency of sequential and individual vein coronary bypass grafts: a systematic review. Ann Thorac Surg 2011;92:1292-8. [Crossref] [PubMed]
- Shin H, Yozu R, Mitsumaru A, et al. Intraoperative assessment of coronary artery bypass graft: transit-time flowmetry versus angiography. Ann Thorac Surg 2001;72:1562-5. [Crossref] [PubMed]
- Morota T, Duhaylongsod FG, Burfeind WR, et al. Intraoperative evaluation of coronary anastomosis by transit-time ultrasonic flow measurement. Ann Thorac Surg 2002;73:1446-50. [Crossref] [PubMed]
- Schmitz C, Ashraf O, Schiller W, et al. Transit time flow measurement in on-pump and off-pump coronary artery surgery. J Thorac Cardiovasc Surg 2003;126:645-50. [Crossref] [PubMed]
- Kim KB, Kang CH, Lim C. Prediction of graft flow impairment by intraoperative transit time flow measurement in off-pump coronary artery bypass using arterial grafts. Ann Thorac Surg 2005;80:594-8. [Crossref] [PubMed]
- Leong DK, Ashok V, Nishkantha A, et al. Transit-time flow measurement is essential in coronary artery bypass grafting. Ann Thorac Surg 2005;79:854-7; discussion 7-8. [Crossref] [PubMed]
- Hassanein W, Albert AA, Arnrich B, et al. Intraoperative transit time flow measurement: off-pump versus on-pump coronary artery bypass. Ann Thorac Surg 2005;80:2155-61. [Crossref] [PubMed]
- Di Giammarco G, Pano M, Cirmeni S, et al. Predictive value of intraoperative transit-time flow measurement for short-term graft patency in coronary surgery. J Thorac Cardiovasc Surg 2006;132:468-74. [Crossref] [PubMed]
- Tokuda Y, Song MH, Ueda Y, et al. Predicting early coronary artery bypass graft failure by intraoperative transit time flow measurement. Ann Thorac Surg 2007;84:1928-33. [Crossref] [PubMed]
- Tokuda Y, Song MH, Oshima H, et al. Predicting midterm coronary artery bypass graft failure by intraoperative transit time flow measurement. Ann Thorac Surg 2008;86:532-6. [Crossref] [PubMed]
- Nordgaard H, Vitale N, Haaverstad R. Transit-time blood flow measurements in sequential saphenous coronary artery bypass grafts. Ann Thorac Surg 2009;87:1409-15. [Crossref] [PubMed]
- Kim HJ, Lee TY, Kim JB, et al. The impact of sequential versus single anastomoses on flow characteristics and mid-term patency of saphenous vein grafts in coronary bypass grafting. J Thorac Cardiovasc Surg 2011;141:750-4. [Crossref] [PubMed]
- Amin S, Pinho-Gomes AC, Taggart DP. Relationship of Intraoperative Transit Time Flowmetry Findings to Angiographic Graft Patency at Follow-Up. Ann Thorac Surg 2016;101:1996-2006. [Crossref] [PubMed]
- Boening A, Friedrich C, Hedderich J, et al. Early and medium-term results after on-pump and off-pump coronary artery surgery: a propensity score analysis. Ann Thorac Surg 2003;76:2000-6. [Crossref] [PubMed]
- Kirmani BH, Brazier A, Sriskandarajah S, et al. Long-Term Survival After Off-Pump Coronary Artery Bypass Grafting. Ann Thorac Surg 2016;102:22-7. [Crossref] [PubMed]
- Chaudhry UA, Harling L, Rao C, et al. Off-pump versus on-pump coronary revascularization: meta-analysis of mid- and long-term outcomes. Ann Thorac Surg 2014;98:563-72. [Crossref] [PubMed]
- Chu D, Bakaeen FG, Dao TK, et al. On-pump versus off-pump coronary artery bypass grafting in a cohort of 63,000 patients. Ann Thorac Surg 2009;87:1820-6; discussion 6-7.
- Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg 2014;46:517-92. [Crossref] [PubMed]
- Christenson JT, Schmuziger M. Sequential venous bypass grafts: results 10 years later. Ann Thorac Surg 1997;63:371-6. [Crossref] [PubMed]


